Scott Kerlin, M.S., Ph.D., with Ian Cameron BSC {Hons} MA, Bob Klaehn, M.D., DFAACAP, and Laura Henton, DNP, APRN, FNP-C
DES International Research Network
February 2026–Comprehensive Update–Academic Literature Review
I. Introduction: Since beginning my academic graduate studies more than 40 years ago, I have been engaged in researching the complexities of gender identity, as an outgrowth of my own interdisciplinary graduate education and my childhood experiences living with gender dysphoria and gender curiosity. Over the years I have learned that the scope of published research in this entire area is quite substantial.
Purpose of this Report
This research digest is a comprehensive bibliography of published scientific literature focusing on the multiple issues relating to gender identity in individuals, including clinical research, comprehensive assessment, biological and neurological components, medical and psychotherapeutic treatment, and other healthcare interventions. It is an extension of my historical investigation of biological factors influencing psychosexual and gender identity development in humans, a field to which I have been deeply focused since the 1990s.
About Dr. Kerlin and the Goal of My Research
I am a confirmed DES son, meaning that I have medically verified that I was exposed prenatally to the endocrine-disrupting drug diethylstilbestrol. I was born in the early 1950s, and I was medically treated for intersex condition at birth and in early childhood; I have also been treated for hypogonadism since my early 20s. Knowledge of this information led me in the 1990s, following completion of my PhD in 1992, to begin investigating the role of DES and similar endocrine-disrupting chemicals in shaping human sexuality and gender identity in humans. In 2005, I authored and presented my first major report, “Prenatal Exposure to Diethylstilbestrol (DES)in Males and Gender-Related Disorders: 5-Year Study.”
Having accepted many years ago that I had strong cross-gender feelings when I was a child, I have come to identify as gender-nonbinary. The journey of self-discovery and self-acceptance has not always been easy, but my depth of research investigation has aided my own compassion for others who have been asking questions similar to my own.
In the mid-1990s, I launched a private professional practice providing confidential supportive professional counseling and mental health services for individuals who identify as transgender, non-binary, LGBTQI+ and questioning with regard to their gender and sexual identity.
Over the years, I have interviewed and surveyed and surveying hundreds of individuals focusing their understanding on their own sexuality and gender identity. Through my interviews I learned that a significant proportion identified on the LGBTQ-Non-binary spectrum. My research was first documented by Deborah Rudacille, M.A., in her 2005 book The Riddle of Gender, and supported by the late Dr. Milton Diamond, Ph.D., Professor of Anatomy and Reproductive Biology at the John A. Burns School of Medicine at the University of Hawaii, Dr. Aaron Devor, Ph.D.,, (the inaugural Chair in Transgender Studies at the University of Victoria, and the founder and subject matter expert of the Transgender Archives, and most recently Dr. Charles Sultan, Professor of Endocrinology at M.D., Ph.D., Chief of the Pediatric Endocrine Unit at the University Hospital of Montpellier, France.
For me, the most essential understanding that represents my ongoing scientific investigation of gender identity is that there are major biological factors that underpin the development of gender identity in humans, as well as psychological factors.
Most recently, my research on gender identity is cited in two investigative publications, one of which (2024) I am co-author:
>> Gaspari, L., Soyer-Gobillard, M.-O., Kerlin, S., Paris, F., & Sultan, C. (2024). Early Female Transgender Identity after Prenatal Exposure to Diethylstilbestrol: Report from a French National Diethylstilbestrol (DES) Cohort. Journal of Xenobiotics, 14(1), 166-175. https://doi.org/10.3390/jox14010010
>> Soyer-Gobillard, M.-O., Gaspari, L. & Sultan, C. (2025), Gender identity disorders: a legacy of fetal exposition to Diethylstilbesterol, an Endocrine Disruptor Chemical. The European Society of Medicine Medical Research
Archives, online 13(3). https://doi.org/10.18103/mra.v13i3.6342 .
I strongly recommend this reference book: Wolf-Gould, C., Denny, D., Green, J. & Lynch K, eds., (2025) A History of Transgender Medicine in the United States: From Margins to Mainstream (Albany: State University of New York Press).
Our Co-Researchers:
(Our Consultant) Bob Klaehn, M.D.
I am a confirmed “DES son.” I was exposed to Diethylstilbesterol in utero during mid-fifties. My mother, a Registered Nurse, told me of my DES exposure after my first urology appointment at age 20. However, it took another 40+ years to fully include this information in my life’s narrative. After my second genitourinary cancer (Bladder Cancer in 2010 and Prostate Cancer in 2020), I began to research the subject in detail and began to re-interpret my life story based on the feminizing effect that DES has had on my neurons. Based on this research and ongoing therapy, I came out as genderqueer within the last few years.
Professionally, I am a Board-Certified Adult and Child Psychiatrist and a Distinguished Fellow of the American Academy of Child and Adolescent Psychiatry (AACAP). I retired from a career in clinical and administrative psychiatry, with a focus on the diagnosis, treatment and management of Autism Spectrum Disorder. I was Medical Director for the Arizona Division of Developmental Disabilities (DDD) for nearly fourteen years, providing medical management for the Medicaid Carve-out Health Plan for DDD-enrolled individuals. I also had the opportunity to provide “house calls” to develop comprehensive treatment for individuals with Autism or Intellectual Disability plus complex mental health issues across the state.
I am an active local, national and international speaker on topics in early childhood mental health and the diagnosis and treatment of persons with Autism Spectrum Disorder and other Developmental Disabilities. In December 2019, I presented four lectures during the international conference “At the Juncture of Psychiatry and Neurology: Disorders in Infants, Adolescents and Young Adults,” in Ivano-Frankivsk, Ukraine. I have continued to provide Continuing Medical Education to Ukrainian Psychiatrists throughout the pandemic and Russian invasion via the Internet.
I received my undergraduate degree in History and Science from The Johns Hopkins University in 1976 and my medical degree from Wayne State University in Detroit in 1980. I received my adult and child psychiatry training at the University of Wisconsin Hospital and Clinics. I am currently Clinical Assistant Professor of Psychiatry for the Creighton University School of Medicine – Phoenix.
About Ian Cameron BSC {Hons} MA
I am a DES son on the basis my mother told me. I have a range of autoimmune conditions, ASD, and an intersex condition, XXY Klinefelter, confirmed by a consultant. On that basis I have an interest in research into Diethylstilboestrol and intersex/gender topics. I was born in 1956 in London, England and often wondered why I felt I didn’t fit in, or belong anywhere, and that something was wrong with me , but not knowing what.
I have spent most of my working life in local government involved in landscape management, conservation and planning at a senior level. I started my working life in Horticulture and Botany.
I have a Bachelors degree in Biology and a Masters degree in Environmental Science, gained through study with the UK Open University.
About Dr. Henton
I am a confirmed DES daughter, meaning that I have medically verified that I was exposed in utero to the endocrine-disrupting drug diethylstilbestrol (DES). I was born in the late 1950’s in western Massachusetts, where my mother was treated in a high-dose cohort. I have received medical and surgical treatment for my DES-related gynecological structural and cellular abnormalities.
I have been working as a nurse since the early 1980’s in a wide variety of settings. I’ve obtained a BSN (Kent State University) & MSN (Walden University); more recently earned the Doctorate of Nursing Practice (DNP) in the Family Nurse Practitioner (FNP) track. I am now pursuing a post-doctorate Psychiatric/Mental Health Nurse Practitioner (PMHNP) certificate from Shepherd University.
II. Areas of Our Overarching Research Focus
How To Use This Report
[December Note: This section is under development, so far with 26 specific research questions and relevant published literature listed below. For each question, the literature that we have identified to have strongest relevance is identified by (Notable).]
Table of Contents
Chapter 1: Gender Identity and Transgender Research
Chapter 2: Gender Dysphoria
Chapter 3: Gender Incongruence
Chapter 4: Nonbinary Identities and Prevalence
Chapter 5: Measures of Gender Identity
Chapter 6: Gender Identity Research with Youths
Chapter 7: Support for People Exploring their Gender Identity
Chapter 8: Mental Health Assessment, Issues and Gender Identity
Chapter 9: Mental Health Treatments and Outcomes for Gender Dysphoria
Chapter 10: Gender-affirming Healthcare
Chapter 11: Additional Healthcare Topics for Transgender and Nonbinary Populations
Chapter 12: Older Adults & Gender Identity–Major Issues
Chapter 13: Resilience in People with Diverse Gender Identity
Chapter 14: Concealment, Stigma, and Disclosure of Gender Identity
Chapter 15: Suicide risk among gender-diverse individuals
Chapter 16: Gender Euphoria in Gender-diverse Individuals
Chapter 17: Gender Fluidity in Adults and Youths/Children
Chapter 18: Body image and medical surgery/transition for Gender-diverse Individuals
Chapter 19: Sexuality Among Transgender and Gender-diverse Individuals
Chapter 20: Sexual Function and Transgender Individuals
Chapter 21: Endocrine Disruptors: Links to Sexuality and Gender Variations in Humans
Chapter 22: Broadening Research on Transgender Identity, Health, and Support
Chapter 23: Disorders/Differences of Sexual Development (DSD) and Related Topics
Chapter 24: Studies of Personal Narratives on Self-discovery about Gender Identity
Chapter 25: Association Between Autism and Variations in Gender Identity
Chapter 26: What are the biochemical pathways that result in the Transgender Brain?
Here is a list of our principal major research questions for Chapters 1-26, each with a summary overview along with relevant studies that have assisted our summative inquiry.
Principal research questions:
>> (Chapter 1) How has gender identity and transgender identity been scientifically researched and investigated over the past few years, and what are the leading issues that continue to be explored in the published literature?
by Ian Cameron and Scott Kerlin
Overview: The process of gender identity development is a highly complex and dynamic experience for each individual. Researchers have covered a broad range of issues associated with identity formation, sometimes distinguishing “gender identity” from “transgender identity”.
Oda and Stiehl [2025] note that in the U.S., approximately 13 million individuals identify as part of a sexual and gender minority (SGM). This broad spectrum includes sexual orientation identities such as gay, lesbian, bisexual, queer, pansexual, and same-gender-loving, as well as gender identities such as transgender, gender non-conforming, bigender, and two-spirit. As behaviour analysts heed the call to engage in culturally competent practices that address diverse sexual orientation and gender identities (SOGI), they will likely consider collecting SOGI data as part of their practice. The benefits of SOGI data collection certainly exist. However, the historical oppression and increased vulnerability of SGM populations require a careful and thorough evaluation of ethical data collection practices to avoid harm and to ensure respectful and inclusive practices.
Given that the dominant discourse about these topics is still grounded in binary measures (Rushton et al., 2019), professionals may overlook the complexity of these constructs and the ongoing cultural competence necessary to address these topics effectively (National Academies of Sciences, Engineering, and Medicine, 2022). With soundly designed procedures and a clear rationale, SOGI data collection can both validate respondents’ identities and yield rich information related to these core identities. Conversely, poorly designed SOGI data procedures risk harming sexual and gender minority (SGM) respondents and can result in the collection of misrepresentation or data that may not accurately reflect the diversity of SOGIs.
Many behaviour-analytic domains may benefit from SOGI data collection, such as clinical practice, Organizational Behaviour Management (OBM), research, education, supervision, and public health. An obvious benefit is learning about respondents’ experiences and needs to better support them. Behaviour analysts must understand that SGM populations constitute a historically oppressed group that is particularly vulnerable to harm.
Self-report is the only socially valid method for SOGI data collection. Research studies and interventions are usually tied to ethical standards, guidelines, and legal policies related to confidentiality. Question framing can influence whether respondents understand the question, feel safe to answer honestly, and experience feelings of affirmation or harm when participating. Using open-ended questions or statements allow for the most descriptive and unbiased SOGI data collection.
From: What do measures of gender identity tell us about gender identity over time? Fisher, Wright and Sargeant [2024] British Journal of Developmental Psychology.
Gender identity is a multifaceted concept and is represented by a wide range of measures and constructs including both self-report and researcher observations of preferences and behaviours. However, despite their similar theoretical underpinning, gender identity measures are rarely found to correlate with one another, and contrasting patterns and trajectories are often found for each construct
The results of this review are consistent with wider research suggesting that distinct developmental patterns can be observed when using different constructs and measures of gender identity. Gender-diverse individuals have been present throughout history and experiences outside of the gender binary are found in cultures around the world.
There are a range of underlying assumptions about what ‘gender’ means and this can vary based on cultural and societal norms. Morgenroth and Ryan (2018) argue that conceptual understandings of gender fall into 3 categories: (1) evolutionary understandings based on biological sex, (2) social structural approaches based on societal norms and structures, and (3) social identity approaches based on gender as a social category with which an individual identifies. Across the research literature, ‘sex’ is often used to refer to the biological characteristics of an individual (e.g., chromosomes), while ‘gender’ typically refers to the societal and cultural meanings associated with femininity and masculinity (Lindqvist et al., 2021). The term ‘transgender’ is operationalized by Lindqvist et al. as ‘individuals whose assigned gender at birth does not correspond to their self-defined gender identity’. These ‘assigned genders’, given to infants at birth, are often based on a dichotomous binary categorization of gender and sex. Some cultures hold on to the belief that gender is a binary system and there are distinct differences between men and women. This can lead to discrimination, self-stereotyping, stereotype threat and institutional biases (Hyde et al., 2019).
With rising numbers of individuals whose experience cannot be defined using these binary categories, theories of gender identity have broadened, reflecting ideas of gender as a spectrum (Gülgöz et al., 2022) with multiple co-occurring constructs (Ho & Mussap, 2019). These perspectives date back to earlier works by Butler (1990) and West and Zimmerman (1987), who argued that ‘gender’ is a performance that we ‘do’ repeatedly based on societal stereotypes, reinforcing an illusion of binary sex. Viewing gender as a societal construct rather than a characteristic determined by biological sex has led to an affirmative model of care being used internationally with gender-diverse individuals, supporting an individual to consolidate their expressed gender (APA, 2015). These models are based on research suggesting that societal expectations and pressure to conform to gender norms have a negative impact on psychological outcomes. A greater awareness of how an individual’s gender identity develops over time, as evidenced by a combination of measures, may support a more nuanced understanding of gender identity development.
Another key finding of this systematic review is that when children reach middle childhood their self-identified gender tends to remain consistent over time (Hässler et al., 2022)
From: Sex/gender diversity and behavioral neuroendocrinology in the 21st century. Costo and Money [2024] Hormones and Behaviour
What does our science really say about sex and gender diversity? And further, what are the unintended consequences of research that involves sex/gender, particularly with regards to the lives of marginalized populations? Even if the science were settled on these matters (and we argue that it is not), to what extent is it appropriate to use research findings to decide who qualifies for protection against discrimination?
Most scientists who study topics like sexual differentiation or sexually selected traits arrive at the lab each day and divide their samples into two categories: female and male. This earnest and logical adherence to the dictum of precedent and the presumed laws of nature feels to many as an ordinary and self-evident ritual. The result is a methodology that relies on a binary before the study even begins.
One main purpose of sexual reproduction is thought to be to facilitate genetic diversity, and the phenotypes related to sexual reproduction itself are among the most plastic and diverse. The genes and other molecular mechanisms that drive sex-related differentiation and behavior are themselves extraordinarily unstable and vary strikingly across taxa, even among closely related species (Capel, 2017). Thus, evoking the existence of gametes and their obvious distinctions as a counterargument to sex/gender diversity is ineffective and distracts from the broader complexity. Moving away from traditional paradigms and toward those that help us understand diversity is a critical task whose time has come.
One well-intentioned approach to allow for broader conceptualizations of sex diversity has been to draw a sharp distinction between “biological sex” (a term with a long history of being used to deny rights; Clarke, 2022) and “gender.” This practice is problematic for two reasons. First, sex and gender are not easily separable in the context of biomedical studies (Pape, 2021)
Second, using either category as a “variable” interferes with precision because both concepts are constructs—amalgams of a variety of traits and other factors (Massa et al., 2023). A second approach to gender inclusivity within biomedicine has been advocacy for and implementation of policies mandating inclusion of females and males in biomedicine research. A false binary.
Studies that are inclusive to trans and gender-diverse (TGD) people are essential to the scientific record yet are notably rare. In addressing this issue, it is critical that studies are designed with a sensitivity to intervening factors affecting marginalized groups
In the words of Roughgarden (2004), “The biggest error of biology today is uncritically assuming that the gamete size binary implies a corresponding binary in body type, behavior, and life history.”
Dividing a sample into two crude categories, male and female, ignores and flattens this complexity, much of which depends on factors such as social context, environmental conditions, developmental time points, and model organisms. Region-by-region analysis of male and female-typical measures of single brains showed a mosaic pattern – within any one individual, areas usually considered to be sex-differentiated on the aggregate may look sex-conforming, nonconforming, or undifferentiated.
As more and more scientists comply with new sex-inclusive policies, the need for forward-thinking tools and training becomes more urgent. At this time in history, research affecting marginalized genders must be rigorous, reproducible, and gender-informed (Massa et al., 2023; McLaughlin et al., 2023; Pape, 2021; Pape et al., 2024; Richardson, 2022; Rich-Edwards et al., 2018). Roughgarden (2004) wrote: “Although biological differences can be found between the sexes and between people of differing gender expression and sexuality, biological differences can also be found between any two people. Behavioural neuroendocrinology has been at the forefront of discovery on the hormonal, genetic, and neural processes underlying sexual differentiation and sex differences in behaviour.
From: How Transgender Adolescents Experience Expressing Their Gender Identity Around New People: An Interpretative Phenomenological Analysis. Wilson, Malik and Thompson. [2021] Journal of Adolescent Research Sage Journals.
Transgender young people are individuals whose gender identity differs from the sex they were assigned at birth. In recent years, the number of adolescents seeking support with gender dysphoria (distress resulting from the incongruence between assigned and experienced gender) has significantly grown (Gender Identity Development Service [GIDS], 2021a). Gender expression to be a key experience of transgender young people that may impact upon the development of their gender identity and psychological well-being.
The establishment of identity is thought to be the primary developmental task of adolescence, during which young people explore different identities through social interactions and eventually form a more stable sense of self (Erikson, 1968). Exploring and expressing one’s gender in social relationships is, therefore, a key part of the development of our internal sense of gender identity. Research with transgender adults indicates that these ideas also apply to the development of transgender identity.
Gender expression and related social experiences have both positive and negative impacts upon the psychological well-being of transgender individuals. Kozee et al. (2012) propose that expressing oneself in a way that is congruent with one’s gender identity while feeling authentic and genuine is important to well-being, and in a study with transgender adults found greater gender congruency to be associated with reduced anxiety and depression, and greater life satisfaction. Gender expression is also important in providing opportunities for affirmation, or social recognition and support, of one’s gender identity. Sevelius’ (2013) gender affirmation framework proposes that social affirmation of gender is important in confirming transgender individuals’ sense of self, and further studies have found affirmation to be related to increased psychological well-being and self-confidence, and reduced dysphoria (Rood et al., 2016; Russell et al., 2018; Sevelius et al., 2021). However, by disclosing and expressing their gender identity, transgender youth also risk being disaffirmed or misgendered, and exposed to gender-based social oppression, stigma, and victimization.
Participants described feeling a need to conform to socially constructed expectations of masculinity to be recognized as male, both in their outward appearance and behaviour and more internally, such as the way they managed and expressed emotions. Most participants found being gendered correctly, or affirmed, to feel significant and positive in the moment, and to have a lasting effect on their emotional well-being and confidence. The feeling of exhausting hyperawareness shared by participants when initially expressing their gender, that became more natural over time. As found in studies of transgender identity development, rather than solely being a means to communicate gender and develop a social identity as male, gender expression also appeared to enable participants to explore, develop, and strengthen their internal sense of their gender identity. The findings also demonstrate that it is important transgender young people are supported to manage stress associated with expressing their gender identity around others.
Research is also warranted in exploring the causal links between experiences of affirmation and misgendering on well-being, and the influence of participant characteristics, such as demographics, access to support, and resilience/coping strategies, on the impact of these experiences.
From: More Than Social Stigma Meets the Eye: The Inherent Struggle of Sexual and Gender Identity Development Across the Lifespan, Bockting [2024] American Journal of Psychiatry.
The findings from this study are consistent with previous research that showed poorer mental health and well-being among plurisexual women. For example, in a longitudinal study of sexual minority women, bisexual and “mostly heterosexual” women were most likely to report hazardous drinking and depression. These findings are typically attributed to the lack of available group-level coping for plurisexual individuals (i.e., a community of gay and lesbian people is more developed and more readily available than a community of bisexual people).
In addition to social and environmental factors so well explicated in the minority stress model, there may be other reasons why changes in sexual or gender identity across the lifespan may be associated with psychological distress, poorer mental health, and decreased well-being. First and most generally, for many people, change is stressful. Among trans and nonbinary people, struggling with one’s gender identity was found to be associated with mental health concerns independent of social stigma. Second, without stress, there might be no growth.
A broader array of theoretical frameworks should be explored to guide the study of sexual and gender minority health and to elucidate developmental vulnerabilities and resiliencies across the lifespan of individuals in relation to their socioecological environment. Finally, we need to use the knowledge already gained to inform and test psychotherapeutic as well as social interventions to mitigate inequities and promote LGBTQ+ people’s health and well-being.
The genetics and hormonal basis of human gender identity. Batista and Loch. [2024] Archives of Endocrinology and Metabolism
Gender identity refers to one’s psychological sense of their own gender. Establishing gender identity is a complex phenomenon, and the diversity of gender expression challenges simplistic or unified explanations. For this reason, the extent to which it is determined by nature (biological) or nurture (social) is still debatable. The biological basis of gender identity cannot be modeled in animals and is best studied in people who identify with a gender that is different from the sex of their genitals such as transgender people and people with disorders/differences of sex development. Numerous research studies have delved into unraveling the intricate interplay of hormonal, neuroanatomic/neurofunctional, and genetic factors in the complex development of core gender identity. In this review, we explore and consolidate existing research that provides insights into the biological foundations of gender identity, enhancing our understanding of this intriguing human psychological trait.
Sexual differentiation involves the development of distinctions between males and females, a phenomenon observed widely in nature, including in human biology. A notable sexually dimorphic trait in humans is gender identity, defined as an individual’s intrinsic perception of themselves as female, male, or as a gender alternative to conventional male and female classifications. In cisgender individuals, the gender identity aligns with the gender assigned at birth and remains consistent throughout their lifespans. Conversely, transgender individuals may consistently or intermittently identify with a gender different from the one assigned at birth.
Given the intricate nature of this framework and its clinical implications, significant attention has been dedicated to understanding the origins of the sexual differentiation process. it is firmly established that biology plays a pivotal role. Accumulating evidence suggests that prenatal sex hormones exert a lasting impact on human sexual development, and heritability studies suggest the involvement of genetic components.
Human sexual development is a dynamic process regulated by genes and executed by endocrine mediators in the form of steroids and peptide hormones. The first stage of sexual development is determined by chromosomal sex (presence of the X or Y chromosome). This chromosome will influence the determination of gonadal sex, differentiating the bipotential gonad into ovaries or testes. The presence and expression of the SRY gene (located on the distal portion of the short arm of the Y chromosome) direct gonadal differentiation toward testes, forming Leydig and Sertoli cells. Sertoli cells produce anti-Müllerian hormone, which causes the involution of Müllerian derivatives, while Leydig cells produce testosterone, differentiating Wolffian ducts into vas deferens, epididymis, and seminal vesicles. The conversion of testosterone to dihydrotestosterone by the action of 5α-reductase type 2 occurs between the sixth and twelfth weeks of gestation and is essential for the development of male internal genital organs and the virilization of external genitalia.
Sexual development continues after gonadal differentiation with cerebral sexual differentiation, occurring in the second half of gestation, where gonadal steroids (especially testosterone) act, even in the prenatal period, causing organizational effects on the brain, leading to permanent changes in brain structure and sexual behaviour. Cerebral sexual development follows the same dynamics as gonadal development, where the presence of androgens is necessary for male development. Gender identity can arise from a complex interplay between nature (biology) and nurture (social).
The authors identified a unique link between TA repeats in ERα and gender dysphoria. Utilizing a binary logistic regression model, the study concluded that certain allele and genotype combinations of ERβ, ERα, and AR are implicated in the genetic basis of transgender identity. Specifically, male-to-female gender development requires AR, accompanied by ERβ, with an inverse allele interaction observed between ERβ and AR in the male-to-female population. Additionally, ERβ and ERα are associated with male gender identity in the female-to-male population, although no interaction between the polymorphisms was found. These findings underscore the significant role of ERβ in human brain differentiation.
Epigenetics explores how external factors influence gene expression and phenotype without altering the underlying DNA sequence, shedding light on how environmental cues shape biological traits across generations.
In the early stages of development, testosterone plays a crucial role in shaping the mammalian brain’s sexual differentiation, leaving lasting impacts on behaviour. In humans, testosterone levels rise in males from approximately weeks 8 to 24 of gestation and resurface during early postnatal development (mini puberty).
Conditions related to prenatal androgen exposure have been a model for studying the influence of sex steroids on gender behaviour. Differences/disorders of sex development (DSD) is a collective term for a group of relatively rare congenital conditions associated with an alteration in chromosomal, gonadal, or anatomic sex. In brief, 5α-reductase is the crucial enzyme for synthesizing dihydrotestosterone from testosterone. In foetuses lacking 5α-reductase, the conversion of testosterone to dihydrotestosterone does not occur during the critical period of external genitalia differentiation. Since dihydrotestosterone is essential for external genital virilization, their genitalia appear typically female or only mildly masculinized at birth. However, individuals with 5α-reductase type 2 deficiency still produce and respond to testosterone in a manner similar to unaffected males. They undergo virilization during puberty if their testes remain in place, subject to the effects of prenatal testosterone exposure.
Many sex differences in human brains are evident in the sizes of particular brain regions. The caudate nucleus, hippocampus, Broca’s area, anterior commissure, and right parietal lobe are larger in females than in males, while the hypothalamus, stria terminalis, and amygdala are larger in males than in females. Most sex differences in the brain have been investigated in regions important for sexual function and reproduction, such as the hypothalamus. The influence of gonadal hormones on the sexual differentiation of these structures has been studied extensively, for instance, in the case of the sexually dimorphic nucleus of the preoptic area. There is evidence that sex differences in cortical structure vary in a complex and highly dynamic way across the human lifespan.
Eliot and cols. believe that the human brain is not “sexually dimorphic” because differences between male and female brains are extremely subtle and variable. The term “dimorphism” has potent heuristic value, reinforcing the belief in categorically distinct organs: a “male brain” and a “female brain” that have been evolutionarily shaped to produce two psychologically distinct categories of people. A picture is emerging not of two brain types nor a continuous gradient from masculine to feminine, but of a multidimensional “mosaic” of countless brain attributes that differ in unique patterns across all individuals.
In conclusion, the exploration of gender identity reveals a multifaceted interplay between biological and social factors, highlighting the complexity of its development. Genetic studies have identified potential links between specific genes and transgender identity, shedding light on the genetic underpinnings of gender identity. Neuroanatomic and neurofunctional differences between sexes have been observed, suggesting possible neurobiological correlates of gender identity. Studies on transgender individuals’ brains have revealed structural shifts toward their gender identity, supporting the neurobiological basis of gender identity. Overall, the intricate nature of gender identity is influenced by several biological factors. However, the orchestration of gender identity encompasses multiple rhythms, lacking exclusivity or singularity. Instead, it manifests as a diverse and plural human phenomenon.
Doyle (2022) observes, “Identity sits at the core of transgender experience. Transgender people are those whose gender identity (and/or expression) does not match their gender assigned at birth, including non-binary and gender diverse individuals. For transgender people, internally recognizing and externally expressing an authentic gender identity can be a complex and shifting process, requiring careful navigation of potentially supportive or hostile social circumstances.”
Wilson, et al. (2021) recognize that the psychological nature of gender identity formation is a combination of individual (inner) and social (external/outer) factors.
Research on the biological factors associated with gender identity (for example, genetic, hormonal, physiological, neuroanatomy) continues to evolve, and can at times lead to conflicting or even controversial conclusions. Levin, et al., (2022) conclude “We question the utility of etiological studies in clinical care, given that transgender identity is not pathological. When etiological studies are undertaken, we recommend new, inclusive designs for a rigorous and compassionate approach to scientific practice in the service of transgender communities and the providers who serve them.”
Brumbaugh-Johnson & Hull, 2019 note that transgender individuals, in the “coming-out” process, “make strategic decisions regarding the enactment of gender and gender identity disclosure based on specific social contexts. Coming out as transgender is best conceptualized as an ongoing, socially embedded, skilled management of one’s gender identity.”
Highlighted References (Under development)
Key Literature References
(Notable) *** Sexual Orientation and Gender Identity (SOGI): A Tutorial on Ethical Data Practices (2025), by Fernanda S. Oda, published in Behavior Analysis in Practice
(Notable) {NEW} *** How Many Adults and Youth Identify as Transgender in the United States? (August 2025), from the UCLA Williams Institute School of Law
(Notable) *** Diverse Gender Identity Development: A Qualitative Synthesis and Development of a New Contemporary Framework (2024), by Molly Speechley, et al., published in the journal Sex Roles
(Notable) *** What do measures of gender identity tell us about gender identity over time? (2024) by Ellena Fisher, et al., published in the British Journal of Developmental Psychology
*** Beyond Wokeness: Why We Should All Be Using a More “Sensitive” Measure of Self-Reported Gender Identity (2024), by Melissa Marcotte, et al., published in the journal Psychological Reports
*** Neurobiological characteristics associated with gender identity: Findings from neuroimaging studies in the Amsterdam cohort of children and adolescents experiencing gender incongruence (2024), by Julie Bakker, published in the journal Hormones & Behavior
(Notable) *** Sex/gender diversity and behavioral neuroendocrinology in the 21st century (2024), by Kathleen V. Casto & Donna L. Maney, published in the journal Hormones & Behavior
(Notable) *** How Transgender Adolescents Experience Expressing Their Gender Identity Around New People: An Interpretative Phenomenological Analysis (2024), by Hannah Wilson, et al., published in the Journal of Adolescent Research
*** White American transgender adults’ retrospective reports on the social and contextual aspects of their gender identity development (2024), by Emily Herry, et al., published in British Journal of Developmental Psychology
*** Exploring gender diverse young adults’ gender identity development in online LGBTQIA + communities (2024), by Kieran (Kie) Cronesberry, et al., published in International Journal of Transgender Health
*** Gender identity importance in cisgender and gender diverse adolescents in the US and Canada (2024), by Natalie M. Wittlin, et al., published in the British Journal of Developmental Psychology
(Notable) *** More Than Social Stigma Meets the Eye: The Inherent Struggle of Sexual and Gender Identity Development Across the Lifespan (2024), by Walter O. Bockting, Ph.D., published in the American Journal of Psychiatry
(Notable) *** The Genetics and Hormonal Basis of Human Gender Identity (2024), by Rafael Loch Batista, et al., published in Archives of Endocrinology & Metabolism
*** Testosterone, Gender Identity and Gender-stereotyped Personality Attributes (2024), by Kathleen V. Casto, et al., published in Hormones & Behavior
(Notable) *** Transgender and Gender Diverse Identity Development in Pediatric Populations (2023), by Samantha Addante, published in Pediatric Annuals
*** Supporting Transgender/Gender Diverse Identity Development Through Embodied Exploration of Gender Euphoria, Joy, and Resilience, by Ray Ciancoitto (2023), unpublished Masters degree thesis, Sarah Lawrence College
*** Biological Studies of Transgender Identity (2023), by Rachel N. Levin, et al., published in the Journal of Gay & Lesbian Mental Health
(Notable) *** Coming Into Identity: How Gender Minorities Experience Identity Formation (2023), by Sonny Nordmarken, published in the journal Gender & Society
(Notable) *** Sexual orientation in transgender adults in the United States (2023), by Sari L. Reisner, et al., published in BMC Public Health
*** What does Transgender Mean to You? Transgender Definitions and Attitudes toward Trans People (2023), by V. N. Anderson, published in Psychology of Sexual Orientation and Gender Diversity
*** “Trans Enough”: Examining the Boundaries of Transgender-Identity Membership (2023), by David Kyle Sutherland, published in the journal Social Problems
(Notable) *** Transgender identity: Development, management and affirmation (2022), by David Matthew Doyle, published in the journal Current Opinion in Psychology
*** Broadening gender self-categorization development to include transgender identities (2022), by Emma F. Jackson, published in Social Development
*** Gender Identity Development in Children and Young People: A Systematic Review of Longitudinal Studies (2021), by Hannah Stynes, et al., published in the journal Clinical Child Psychology and Psychiatry
*** Sex, Gender and Gender Identity: A Re-Evaluation of the Evidence (2021), by Lucy Griffin, et. al, published in the journal BJPsych Bulletin
*** The Neuroanatomy of Transgender Identity: Mega-Analytic Findings From the ENIGMA Transgender Persons Working Group (2021), by Sven C. Mueller, et al., published in The Journal of Sexual Medicine
(Notable) *** Navigating identity: Experiences of binary and non-binary transgender and gender non-conforming (TGNC) adults (2020), by Chassity Fiani, et al., published in The International Journal of Transgender Health
*** Chapter 8 – Biological basis of gender identity (2020), by Alessandra Daphne Fisher & Carlotta Cocchetti, published in The Plasticity of Sex: The Molecular Biology and Clinical Features of Genomic Sex, Gender Identity and Sexual Behavior (ed: Marianne J. Legato)
*** Coming Out as Transgender: Navigating the Social Implications of a Transgender Identity (2019), by Stacey M. Brumbaugh-Johnson, published in the Journal of Homosexuality
*** Transnormativity and Transgender Identity Development: A Master Narrative Approach (2019), by Nova J. Bradford & Moin Syed, published in Sex Roles
(Notable) *** Hormones, Sexual Orientation & Gender Identity (2019), by NC Neibergall, et al., published in The Oxford Handbook of Evolutionary Psychology and Behavioral Endocrinology (2019), Chapter 12
*** Gender identity development among transgender and gender nonconforming emerging adults: An intersectional approach (2018), by L. E. Kuper, et al., published in International Journal of Transgenderism
(Notable) *** Neurobiology of gender identity and sexual orientation (2018), by C. E. Roselli, published in Journal of Neuroendocrinology
(Notable) *** Evidence Supporting the Biologic Nature of Gender Identity (2015), by Aruna Saraswat, et al., published in Endocrine Practice
*** Gender Identity Development: A Biopsychosocial Perspective (2014), by Annelou L. C. de Vries , published in Gender Dysphoria and Disorders of Sex Development: Progress in Care and Knowledge
*** (Historical) Witnessing and Mirroring: A Fourteen Stage Model of Transsexual Identity Formation (2004), by Aaron Devor, published in Journal of Gay & Lesbian Psychotherapy
>> (Chapter 2) How has the concept of gender dysphoria and related research evolved over time?
Overview, by Ian Cameron
Over the past 30 years, the concept of gender dysphoria and major research focusing on it has substantially evolved.
From: What is the Best Approach to Removing the Social Stigma from the Diagnosis of Gender Dysphoria? Milionis, C. [2025]. Health Care Analysis in Springer Nature.
Historically, the transgender population has faced prejudice and discrimination within society. The purpose of diagnostic terms is to direct clinical care and facilitate insurance coverage. However, the existence of a medical diagnosis for gender nonconformity can exacerbate the stigmatization of transgender people with adverse consequences on their emotional health and social life. Whether transgenderism and gender dysphoria are indeed a psychopathological condition or even any kind of nosological entity is a contested issue. Many advocates of human rights, trans activists, social scientists, and clinicians support either the removal of gender incongruence from the list of mental disorders or at least its transfer to a separate category. Reforming the classification is an intermediate step toward depathologization and permits access to transgender-related care. Nonetheless, it partly preserves the stigma associated with abnormality and puts the availability of psychiatric care at risk. A more radical approach dictates that the classification of diseases serves exclusively medical purposes and must be dissociated from the respect for the legitimacy of one’s autonomy and dignity. In the long term, only a swing in societal values can detach stigma from mental and physical illnesses. Enhancing collective respect for life, human rights, and diversity is the best way to achieve cohesion and well-being among members of society. Health professionals can be pioneers of social change in this field.
From: Mapping the evolution of gender dysphoria research: a comprehensive bibliometric study. Aria, M., D’Aniello, L., Grassia, M.G. [2024] Quality and Quantity in Springer Nature
The definition of gender dysphoria has been the subject of extensive scientific debate in various fields. The Diagnostic and Statistical Manual of Mental Disorders, 5th edition (DSM-V) characterizes gender dysphoria as a psychological condition due to a discrepancy between perceived and assigned gender. The scientific community has engaged in an extensive debate over the years regarding the classification of gender dysphoria, initially characterizing it as a gender identity disorder and subsequently removing it from the category of mental disorder.
This leads to various levels of discomfort, as individuals may feel uncomfortable with their biological sex, primary and secondary sexual characteristics, and social gender roles. Over the years, the scientific debate to establish a clear definition of gender dysphoria and explore the social and psychological consequences for people who experience dysphoria has been varied and has covered different fields of interest
According to the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-V), a diagnosis requires a condition persisting for over six months with a presence of at least two of these symptoms:
- Discomfort regarding the alignment of perceived sex and primary and secondary sexual characteristics.
- A desire to change one’s sexual characteristics.
- A wish to acquire the sexual characteristics of the opposite gender.
- An inclination to identify as the opposite gender.
- A longing to be acknowledged and treated as the opposite gender by others.
- A belief in possessing emotions and reactions typical of the opposite gender.
Additionally, the second criterion states that the condition must be associated with clinically significant distress or impairment in social, occupational, affective-relational, and other areas of life. People who experience gender dysphoria may identify themselves as transgender, nonbinary, or, more generally trans , but not all trans and intersex people experience gender dysphoria.
The research delves into the psychological, social, and medical aspects of gender dysphoria, exploring factors like self-acceptance, social support, mental health outcomes, and the effectiveness of different interventions and treatments. Scholars and researchers have engaged in extensive debates regarding gender dysphoria since the 1970 s, leading to a transformative shift in understanding the condition.
Recognizing the evolution of focus and related issues surrounding gender dysphoria is crucial for ongoing progress in the field and providing support to individuals experiencing this condition. Over time, there has been a significant shift in the understanding and approach to addressing gender dysphoria, reflecting an increasing awareness of gender identity. This research played a pivotal role in dispelling myths about sexual orientation, affirming that it is not a choice and is not influenced by psychological or social factors.
These studies highlighted the intricate nature of gender dysphoria, emphasizing its biological basis and establishing the groundwork for evaluating the efficacy of gender-affirming treatments in enhancing the quality of life for individuals with gender dysphoria.
Over the past two decades, shifts in trends and perceptions regarding gender dysphoria have been influenced by a multitude of events such as the LGBTQ + rights movements, the evolution of gender theories, and diagnostic revisions. One significant change in diagnosis involves a shift from a behavioural and sexual focus to a broader consideration of a person’s identity. This shift reflects the recognition that being transgender is not a mental disorder, with significant implications: reparative therapies, forced hospitalization, and sterilization, once aimed at altering or suppressing an individual’s gender identity, are now acknowledged as harmful and are no longer endorsed by the WHO.
Transitioning to ethical considerations, we acknowledge the unique challenges associated with researching gender dysphoria—a subject deeply entwined with personal identity, social stigma, and mental health. Our ethical approach to researching gender dysphoria is grounded in a commitment to do no harm, advance knowledge with compassion and respect, and contribute to a more inclusive and supportive society for all individuals, irrespective of their gender identity.
From: A narrative review of gender dysphoria in childhood and adolescence: definition, epidemiology, and clinical recognition. Clemente, Jasser and Koenig. [2024] Pediatric Medicine.
There is increasing evidence on the contributions of genetics, hormone influences and neurobiology on gender identity. Furthermore, data on the benefits of access to gender affirming therapy continue to emerge. Transgender youth are at increased risk of psychiatric comorbidities such as depression, anxiety, and life-threatening behaviors. As such, studies underscore the importance of early recognition, mental health support and medical intervention through hormone treatments for pubertal suppression and/or gender-affirming hormone therapy in decreasing mental health burdens and improving quality of life among the transgender youth.
Concepts of gender variance have evolved over the years and continue to do so. In the past 10 years alone, the number of transgender/gender-diverse children and adolescents has increased. Current data indicates approximately 0.1–0.2% of the general population consider themselves as transgender/gender non-conforming. Increased public awareness brought about by heightened media representation, de-stigmatization and increased understanding of gender and gender diversity, are among the proposed explanations for this upsurge in numbers. More youth considered as transgender and gender diverse, particularly those that experience gender dysphoria, seek transition-related medical care, thus there is a growing and continued need to improve knowledge and expertise in this topic.
What determines a person’s gender identity is likely influenced by multiple constructs, including biology, social interactions within one’s environment, as well as cultural dictates. Results of research focusing on biological determinants of gender development support the hypotheses of genetic, endocrine, and neuroanatomic influences on gender. Gender dysphoria was significantly associated with the number of alleles and genotypes that were studied. Another study by Fernández et al., assessed the role of oestrogen receptors alpha (ERα), beta (ERβ), androgen receptor (AR), and aromatase (CYP19A1) on brain differentiation of humans. They showed that specific genotype and allele combinations of these receptors are involved in the genetic basis of gender-diversity, and that ERβ plays an important role in brain differentiation of humans.
Previous studies that has looked into 2D:4D finger ratio in transgender individuals have contradictory results, however, in 2020, Siegmann et al. presented new data and results of a meta-analysis that showed higher (feminized) 2D:4D finger ratio in male to female transgender individuals when compared to the male controls
Similar to results of investigations on effect of genetics and hormone exposure, studies in neuroanatomy and functional neuroimaging in transgender individuals have been inconclusive; however, a main hypothesis for GD assumes that an individual’s perceived gender can be related to sexual differentiation of the brain and suggests that in transgender individuals, a deviation between sex differentiation of the brain and reproductive organs can occur, as a result of genetic factors and/or effects of testosterone during fetal development.
Children and adolescents with gender identity concerns and/or their families may also delay seeking advice or medical care which can be due to fear of stigma associated with being transgender or gender diverse, or due to lack to health care access. Primary care providers should be aware that children and adolescents who have gender dysphoria might be concerned about expressing their thoughts about their identity to their families and peers. This might be due to fear of social stigmatization from being labelled as a lesbian, gay, bisexual, transgender, and queer (LGBTQ). LGBTQ adults report that experiences of interpersonal discrimination and violence that can range from emotional, verbal and physical forms. The same is true for transgender youth, who also commonly report negative experience that directed toward expressing their gender identity in term of accessing appropriate bathroom facilities or participating in gender specific activities, and other forms of school victimization.
It is considered unethical for health care providers managing individuals with gender dysphoria to deliver care that aims to make them congruent with their sex assigned at birth. The process of gender transition refer to the act of altering one’s physical, social, and/or legal characteristics to match their affirmed gender identity. For pre-pubertal children, this transition is primarily a social process, adopting gender-affirming names, hairstyles, clothing, pronouns and use of restrooms or other facilities. During this social transition, continued assessment of the person’s feelings and response to the social transformation would allow both the individual and gender care provider to have a better understanding on how to proceed.
Hormonal therapy can be provided by an endocrinologist to either halt the progression, change, assist in acquiring with secondary physical characteristic of desired gender or both. The role of gender-affirmation surgery (GAS) usually comes after hormonal therapy. GAS is a group of surgical procedure that aims to affirm an individual’s body with their gender identity. These include subcutaneous mastectomy, breast augmentation, vaginoplasty, metoidioplasty, phalloplasty and facial feminization/masculinization surgery. Most of these surgeries are performed after the age of 18 except for “masculinizing” mastectomy, which can be done at the of 16. GAS have shown multiple benefits to the patients, including an improvement of quality of life, satisfaction with appearance and body image, and decrease in gender dysphoria. Being a major surgery, the decision of GAS must be shared between the surgeon and the patient, and must be based on deep awareness of the patient own goals, expectations, associated risks and complications, and after exploration of all the alternative therapy options.
From: The Misuse of Gender Dysphoria: Toward Greater Conceptual Clarity in Transgender Health. Ashley F. [2021] Perspectives on Psychological Science
The notion of gender dysphoria is central to transgender health care but is inconsistently used in the clinical literature. Clinicians who work in transgender health must understand the difference between the diagnosis of Gender Dysphoria as defined and described in the fifth edition of the Diagnostic and Statistical Manual of Mental Disorders and the notion of this term as used to assess eligibility for transition-related interventions such as hormone-replacement therapy and surgery. Unnecessary diagnoses due to the belief that a diagnosis is clinically required to access transition related care can contribute to stigma and discrimination toward trans individuals.
Gender dysphoria, which refers to the distress and dis comfort some trans people experience because of the discrepancy between their gender assigned at birth and gendered self-image, has been a centerpiece concept of trans health care in recent years. Yet wielding the unwieldy notion of gender dysphoria is an arduous task for even the most hardened of clinicians.
Noncorrespondence of gender identity and gender assigned at birth is increasingly understood as a matter of human diversity rather than as pathology. People naturally develop gender identities, and some people turn out to be trans as a result. The growing understanding of transgender identities as nonpatho logical builds on trans communities’ self-conception as normal people and is foundational in trans advocacy and scholarship. Many trans people are healthy and well-adjusted people. Applying the label of mental ill ness seems ill-suited. And although many trans people do suffer from mental-health issues, these tend to occur as a by-product of stigma and minority stress rather than because of transness.
From a depathologizing perspective, the distress in gender dysphoria is not indicative of mental illness but is a normal psychological response to having a body that does not correspond to one’s gendered self-image. Trans people’s gender identities are part of normal human diversity and, for some people, those gender identities involve gendered self-images that differ from their bodies. Because being trans is normal, resulting distress is understood as relating to the body rather than to the mind. Medical transition lessens or extinguishes gender dysphoria.
A few reasons may be given in support of giving a mental-health diagnosis. First, it may be argued that a diagnosis of gender dysphoria is helpful in guiding treatment. Second, it may be argued that the diagnosis is helpful in shielding surgeons from liability. Third, it may be argued that a diagnosis of gender dysphoria helps to identify trans patients in medical charts in hospital settings. However, trans patients have diverse medical needs, and not all trans patients are diagnosed or diagnosable with gender dysphoria.
A diagnosis of gender dysphoria is not required to access transition-related interventions in the WPATH Standards of Care. Unnecessary diagnoses of gender dysphoria are incompatible with the depathologizing animus of con temporary trans health.
From: How Early in Life do Transgender Adults Begin to Experience Gender Dysphoria? Why This Matters for Patients, Providers, and for Our Healthcare System. Zaliznyak M. et al. [2021] National Library of Medicine
The age at which transgender women (TW) and men (TM) first experience gender dysphoria (GD) has not been reported in a U.S. population of adults seeking genital gender-affirming surgery (gGAS). Because gender is an innate part of identity, we hypothesized that untreated GD would be a part of individuals’ earliest memories. Understanding GD onset can help guide providers with when and how to focus care to patients not yet identified as “transgender“.
Patients self-reported their earliest recollections of experiencing GD, earliest memories in general, and history of anxiety, depression, and suicide attempt. Our findings suggest that GD typically manifests in early childhood and persists untreated for many years before individuals commence gender transition. Diagnosis and early management during childhood and adolescence can improve quality of life and survival.
This study highlights how transgender adults tend to live many years with untreated GD before starting any form of gender-affirming transition (social, hormonal, or surgical). When we consider that life-years of any untreated condition are a robust predictor for morbidity and decreased quality of life, the number of life-years associated with GD and its associated morbidities is striking and serves as a compelling reason for intervention.
From: Gender Dysphoria: Overview and Psychological Interventions. Lavorato E, Rampino A, Giorgelli V. [2022] Practical Clinical Andrology in Springer nature.
In the DSM V, the condition known as “Gender Identity Disorder” becomes “Gender Dysphoria” in order to avoid the stigma of being labeled as carriers of psychopathology. Gender Dysphoria (GD) refers to mental discomfort deriving by incongruence between the expressed gender and the assigned one. The term Transgender refers to identities or gender expressions that differ from social expectations typically based on the birth assigned sex. Not all people living “Gender Variance” express psychological or physic discomfort. The personal gender identity develops influenced by emotionally significant relationships and by socialeducational environment, based on predisposing biological characteristics. Most of clinical and psycho-social studies agree on multifactorial nature of this process, focusing on the combined action of biological, psychological, social and cultural factors. The first symptoms of gender dysphoria may appear from first years of life and then they may persist in puberty and adulthood. The causes of Gender Dysphoria are still unclear.
Both psychosocial and biological factors have been called into question to explain the onset. The Gender Dysphoria Treatment aims to reduce, or to remove, suffering of person with GD and it is based on teamwork of psychologists, psychiatrists, endocrinologists and surgeons. The cure is, firstly, psychological and is provided by mental health experts. Hormone therapy can be prescribed to all people with persistent and well documented Gender Dysphoria if there are no medical contraindications; lastly, sex reassignment surgery. The formation and definition of transgender and transsexual identity obviously represents a specific complexity, to which is added an environmental, cultural and consequently individual and conditioning stigmatization.
Literature reports that Gender Dysphoria (GD)—defined as marked incongruence between one’s expressed gender and her/his assigned gender—is associated with psychological suffering characterized by anxiety, depression, impaired relationships, and suicidal ideation. The difference between one’s expressed gender and her/his physical sexual characteristics is expressed by the desire to get rid of them and/or to have the primary and secondary sexual characteristics of the opposite gender. The peculiarity of this disorder is the coexistence of medical aspects (biological sex) and psychological aspects (subjective experience). Previous studies highlight that psychological risk does not derive from the gender inconsistency, but from childhood traumatic experiences in different contexts, such as family, school, and because of non-recognition of psychological and sexual identity.
Therefore, Gender Dysphoria (GD) represents the condition of partial or complete discordance between assigned sex, based on external genitalia, and the gender recognized by the brain. So, it is characterized by suffering, malaise, and stress.
The term Transgender refers to identities or gender expressions that differ from social expectations typically based on the birth assigned sex. Transgender people can have a binary gender identity (identifying themselves as women if at birth they were men or as men if at birth they were women) or non-binary (identifying themselves with subjective combination of genres). Not all people living “Gender Variance” express psychological or physical discomfort. Most of them find balance between the perception of oneself and the subjective model of relationships. On the other hand, if there is a psychological or physical distress, the so-called Gender Dysphoria, the person could feel the need to adapt the external reality (anatomical and personal data) to his or her emotional inner world.
The biological sex is the set of all biological characteristics of being female or male (biological sex): the sex chromosomes (XY for males and XX for females), the gonads (testes for males and ovaries for females), external genitalia, and secondary sexual characteristics (development of breasts, presence of face hair, tone of the voice, etc.) which appear during the sexual development (puberty).
Gender is a more complex construct and refers to characteristics depending on cultural, social, and psychological factors that define typical behaviours for men and women. For most people, biological sex and gender identity match. The term transgender identifies people with gender identity other than biological sex: for example, a person born as male, but feeling female (or vice versa). The condition that gender identity differs from biological sex is known as gender incongruence. The gender incongruence is not a disorder. In the last edition of International statistical classification of diseases and related health problems (ICD-11), gender incongruence was declassified from the chapter of mental health and included in the chapter of sexual health. If psychological discomfort of gender incongruence is structured in persistent and specific symptoms with an associated alteration of the global functioning, that is Gender Dysphoria.
Gender Dysphoria appears as malaise and discomfort towards one’s body, felt as a stranger; the same sense of strangeness is experienced towards behaviours and attitudes that are typical of one’s sex, within which the person does not recognize her/himself. The first symptoms of gender dysphoria may appear from the very early years of life, 2–3 years.
Gender Dysphoria Criteria in Children
- A marked incongruence between one’s experienced/expressed gender and their assigned gender, lasting at least 6 months, as manifested by at least two of the following (one of which must be the first criterion):
- A strong desire to be of the other gender or an insistence that one is the other gender (or some alternative gender different from one’s assigned gender).
- In boys (assigned gender), a strong preference for cross-dressing or simulating female attire; or in girls (assigned gender), a strong preference for wearing only typical masculine clothing and a strong resistance to the wearing of typical feminine clothing.
- A strong preference for cross-gender roles in make-believe play or fantasy play.
- A strong preference for the toys, games, or activities stereotypically used or engaged in by the other gender.
- A strong preference for playmates of the other gender.
- In boys (assigned gender), a strong rejection of typically masculine toys, games, and activities and a strong avoidance of rough-and-tumble play; or in girls (assigned gender), a strong rejection of typically feminine toys, games, and activities.
- A strong dislike of one’s sexual anatomy.
- A strong desire for the physical sex characteristics that match one’s experienced gender.
- The condition must be associated with clinically significant distress or impairment in social, occupational, or other important areas of functioning. These behaviours in gender dysphoria are associated with deep suffering and distress at school and in relationships. Rather consistently, in children with gender dysphoria, anxiety and depression are common.
Gender Dysphoria Criteria in Adolescents
- A marked incongruence between one’s experienced/expressed gender and their assigned gender, lasting at least 6 months, as manifested by at least two of the following:
- A marked incongruence between one’s experienced/expressed gender and primary and/or secondary sex characteristics (or in young adolescents, the anticipated secondary sex characteristics).
- A strong desire to get rid of one’s primary and/or secondary sex characteristics because of a marked incongruence with one’s experienced/expressed gender (or in young adolescents, a desire to prevent the development of the anticipated secondary sex characteristics).
- A strong desire for the primary and/or secondary sex characteristics of the other gender.
- A strong desire to be of the other gender (or some alternative gender different from one’s assigned gender).
- A strong desire to be treated as the other gender (or some alternative gender different from one’s assigned gender).
- A strong conviction that one has the typical feelings and reactions of the other gender (or some alternative gender different from one’s assigned gender).
- The condition must also be associated with clinically significant distress or impairment in social, occupational, or other important areas of functioning. It is very difficult to have or suppress these feelings, and as a result, people with gender dysphoria may present with anxiety, depression, engage in self-harm, and have suicidal thoughts.
In both children and adults investigate as to whether a Sexual Development Disorder is present.
The causes of Gender Dysphoria are still unclear and both psychosocial and biological factors have been implicated. Currently, the most accepted hypothesis is that both factors contribute to its development [6, 7]. Even if social factors, such as education, environment, and events of life, are of great importance in emergence of gender dysphoria, there is still no experimental evidence to support this theory.
Other studies focused on brain area differences between male and female population and suggested that cerebral architecture of individuals with Gender Dysphoria resembles the one of individuals with the same gender identity rather than those with the same biological sex, thus suggesting that non-biological factors may play a predominant role in GD genesis.
Treatment of Gender Dysphoria aims to reduce, or remove, suffering based on teamwork of psychologists, psychiatrists, endocrinologists, and surgeons. Treatments are not always necessary and the treatment process is not the same for all people. Indeed, the procedure is different according to real needs of the individual.
First line treatment of GD in children and adolescents is psychological intervention that must be provided by mental health experts (child psychologists and neuropsychiatrists), especially if specialized in issues related to developmental age. Psychological support allows to face current problems and provides help to reduce emotional suffering sometimes allowing for more drastic treatment avoidance.
The approach to Gender Dysphoria in adolescence requires careful evaluation, with particular care in making differential diagnoses with other conditions in order to define individualized paths. For example, it is important to distinguish Gender Dysphoria from internalized homophobia that occurs in some adolescents who, failing to accept their homosexual orientation, may require a medical gender reassignment (GR). Depending on the cultural context, their belief system, or even stereotyped views of social arrangements, some homosexual adolescents may mistake their sexual orientation for gender identity, due to a history of borderline behaviours and cross-gender interests in childhood.
The treatment for adults should consist of; psychological support if necessary, feminizing or masculinizing hormone treatment (cross-sex therapy), Sex reassignment surgery.
A significant part of transgender people’s suffering originates precisely from the stigmatization deriving from a stereotyped vision of the concept of gender along with all additional stressors, connected to the stigma of gender non-conformity, and that may negatively affect the psycho-physical health of the individual. This phenomenon, known as Minority Stress, affects people belonging to social categories stigmatized and subjected to excessively high levels of stress, such as those derived from violence, discrimination, and stigmatization.
The formation and definition of transgender and transsexual identity have a high specific complexity, to which environmental and cultural stigmatizations add further complexity. However, it is essential to recognize that the transgender and transsexual evolutionary path preserves the typical dynamics of any identity construction process. Therefore, in clinical work with these people, it is important to consider both the identity structure of the person and the universal evolutionary processes. Approaching transsexual people with the prejudice of an absolute diversity in the formation of the self and identity can compromise the understanding of psychological processes behind while preventing from a fully empathic relationship, that is needed in order to establish a good therapeutic alliance.
Highlighted References (Under development)
Key Literature References
*** What is the Best Approach to Removing the Social Stigma from the Diagnosis of Gender Dysphoria? (2025), by Charalampos Milionis, published in Health Care Analysis
*** Perspectives about key measures of gender dysphoria based on interviews with people with lived experience of gender dysphoria (2025), by Karl Mears & Chris Ashwin published in International Journal of Transgender Health
*** Systematic review of prospective adult mental health outcomes following affirmative interventions for gender dysphoria (2025), by Lucas Shelemy, et al, published in International Journal of Transgender Health
*** An Integrated Framework for Conceptualizing and Measuring Gender Dysphoria: Development and Psychometric Evaluation of the Multidimensional Gender Dysphoria Measure (2025), by M. Paz Galupo, et al. published in American Psychologist
*** Predicting NSSI among trans young people: the role of transphobic experiences, body image, and gender dysphoria (2025), by Kirsty Hird, et al., published in International Journal of Transgender Health
*** Reevaluating gender-affirming care: biological foundations, ethical dilemmas, and the complexities of gender dysphoria (2025), by Marc J. Defant, published in Journal of Sex & Marital Therapy
(Notable) *** Mapping the Evolution of Gender Dysphoria Research: A Comprehensive Bibliometric Study (2024), by Massimo Aria, Luca D’Aniello, Maria Gabriella Grassia, Marina Marino, Rocco Mazza & Agostino Stavolo, published in the journal Quality & Quantity
*** Assessing Gender Dysphoria: Development and Validation of the Gender Preoccupation and Stability Questionnaire – 2(nd) Edition (2024), by Sarah Joy Bowman, et al., published in the Journal of Homosexuality
(Notable) *** A narrative review of gender dysphoria in childhood and adolescence: definition, epidemiology, and clinical recognition (2024), by Ethel Gonzales Clemente, et al., published in Pediatric Medicine
*** Physical and psychosocial challenges of people with gender dysphoria: a content analysis study (2024), by Zahra Ghiasi, et al., published in BMC Public Health
*** Gender-Related Minority Stress and Gender Dysphoria: Development and Initial Validation of the Gender Dysphoria Triggers Scale (GDTS) (2023), by Chloe Goldbach& Douglas Knutson, published in the journal Psychology of Sexual Orientation and Gender Diversity
*** Gender Dysphoria: Overview and Psychological Interventions (2023), by Elisabetta Lavorato, et. al, published in the textbook Practical Clinical Andrology (Carlo Bettocchi, et. al, editors)
*** Assessing Gender Dysphoria: A Systematic Review of Patient-reported Outcome Measures (2023), by Sarah Joy Bowman, et. al, published in the journal Psychology of Sexual Orientation and Gender Diversity
(Notable) *** The Misuse of Gender Dysphoria: Toward Greater Conceptual Clarity in Transgender Health (2021), by Florence Ashley, published in the journal Perspectives on Psychological Science
(Notable) *** How Early in Life do Transgender Adults Begin to Experience Gender Dysphoria? Why This Matters for Patients, Providers, and for Our Healthcare System (2021), by Michael Zaliznyak, et al., published in the journal Sexual Medicine
*** Trapped in the Wrong Body? Transgender Identity Claims, Body-Self Dualism, and the False Promise of Gender Reassignment Therapy (2021), by Melissa Moschella, published in The Journal of Medicine and Philosophy
(Notable) *** Age at First Experience of Gender Dysphoria Among Transgender Adults Seeking Gender-Affirming Surgery (2020), by Michael Zaliznyak, et al., published in JAMA Network Open
*** “Every Time I Get Gendered Male, I Feel a Pain in my Chest”: Understanding the Social Context for Gender Dysphoria (2020), by Galupo, M.P., Pulice-Farrow, L., & Lindley, L., published in the journal Stigma and Health
*** Gender Dysphoria: Definitions, Classifications, Neurobiological Profiles and Clinical Treatments (2020), by Giulio Perrotta, published in the International Journal of Sexual and Reproductive Health Care
(Notable) *** Etiological Factors and Comorbidities Associated with “Gender Dysphoria”: Definition, Clinical Contexts, Differential Diagnosis, and Clinical Treatments (2020), by Giulio Perrotta, published in the International Journal of Sexual and Reproductive Health Care
*** The Phenomenology of Gender Dysphoria in Adults: A Systematic Review and Meta-Synthesis (2020), by Kate Cooper, et. al, published in the journal Clinical Psychology Review
*** Gender Dysphoria in Adults: An Overview and Primer for Psychiatrists (2018), by William Byne, et. al, published in the journal Transgender Health
*** Epidemiology of Gender Dysphoria and Transgender Identity (2017), by Kenneth Zucker, published in the journal Sexual Health
>> (Chapter 3) What research has focused on gender incongruence, and how is it distinct from gender dysphoria?
Overview by Ian Cameron
Overview: Similar to gender dysphoria, gender incongruence (GI) is a condition in which an individual’s gender identity, role, and expression differ from their assigned sex (Oh, et al., 2023). Saffie & Bauerle (2023) observe that “The discordance between biological sex and gender identity has been conceptualized in multiple ways in the scientific literature: Transsexualism (DSM III), Transgenderism, Gender Identity Disorder (DSM IV and ICD X), Gender Dysphoria (DSM V), and Gender Incongruence (ICD XI).”
Schellenberg & Bombardier (2024) note “the two most influential contemporary diagnostic formulations– Gender Incongruence in the ICD-11 and Gender Dysphoria in the DSM-5-TR. These differences and much of the debate around the diagnoses are related to a dilemma: While gender diversity is not pathological, many trans and gender-diverse people still need a medical diagnosis to access health care and legal rights, and balancing stigma reduction and access to care poses a challenge. Requiring individuals to have psychotherapy before allowing access to care is no longer recommended.”
From: Etiology of gender incongruence and its levels of evidence: A scoping review protocol. Saffie JPR and Bäuerle NE. 2023. PLOS One.
Gender Incongruence refers to the discordance between biological sex and gender identity. Although it is possible to find literature reviews about the etiology of Gender Incongruence, almost all of these correspond to non-systematic narrative reviews, so they do not make explicit the methodology used in the collection and analysis of sources, even less its levels of evidence. In order to remedy this, we will conduct a scoping review to answer the question: what are the factors associated with gender incongruence and what level of evidence is there for each factor in the scientific literature?
In 1923, Magnus Hirschfeld introduced the concept of “transsexual” into professional literature to refer to a patient who presented a discordance between biological sex and gender identity [1]. He proposed that both homosexuality and transsexuality were due to natural sexual variability, explained by a set of hormonal factors originated in what he called “glandular orchestra”
The discordance between biological sex and gender identity has been conceptualized in multiple ways in the scientific literature: Transsexualism (DSM III), Transgenderism, Gender Identity Disorder (DSM IV and ICD X), Gender Dysphoria (DSM V), and Gender Incongruence (ICD XI).
Throughout these almost 100 years of research, significant correlations have been found between Gender Incongruence (GI) and biological, social and psychological phenomena, some of which have led researchers to propose etiological hypotheses of great interest. Some have proposed that gender incongruence stems from non-normative exposure to hormones in the womb. According to this view, the excess of testosterone in the female, or its defect in the male, could shape the brain in an unusual way, inclining these subjects toward the formation of gender incongruence. While others have postulated that GI could be induced by the family system. From this perspective, gender incongruence would be a response by the child to resolve an unconscious parental conflict, allowing for system homeostasis. There are also some theorists who postulate GI as a consequence of some clinical condition. For example, it has been postulated that the obsessiveness and rigidity of patients with ASD could lead them to a fixation with gender issues, facilitated by their difficulty in tolerating ambiguity. Finally, there are others who propose that multiple factors must be present for a GI to develop, and that each case may be uniquely configured.
This begs the research question: What are the factors associated with gender incongruence and what level of evidence is there for each factor in the scientific literature?
In the chapter on adolescents of the Standards of Care for the Health of Transgender and Gender Diverse People (8th edition), the following is stated: “A provider’s key task is to assess the direction of the relationships that exist between any mental health challenges and the young person’s self-understanding of gender care needs and then prioritize accordingly”. In this sense, the study of the factors associated with gender incongruence is a contribution to clinical assessment, even more so considering that: “mental health can also complicate the assessment of gender development and gender identity-related needs. For example, it is critical to differentiate gender incongruence from specific mental health presentations, such as obsessions and compulsions, special interests in autism, rigid thinking, broader identity problems, parent/child interaction difficulties, severe developmental anxieties, trauma, or psychotic thoughts. Mental health challenges that interfere with the clarity of identity development and gender-related decision-making should be prioritized and addressed”.
Since the beginning of the last decade, treatment for gender incongruence has consisted primarily in gender-affirming medical care. However, several international health authorities have raised concerns over the uncertain risk-benefit ratio of using hormonal interventions (specifically “puberty blockers” and cross-sex hormones) as the first-line treatment approach for young people under 18, and are restructuring their systems to prioritize psychotherapy as the first line of treatment. Even the principal investigator of the Dutch model has stated that “an individualized approach can be offered that differentiates who will benefit from medical gender affirmation and for whom (additional) mental health support might be more appropriate”. Moreover, the Dutch team itself has reached similar conclusions: “To ensure that each adolescent receives the treatment that best suits them, it is important to thoroughly explore all aspects of gender and general functioning with all adolescents before making decisions about further treatment. The conclusion of a previous study that gender-affirming treatment earlier in life may have benefits is not necessarily founded for everyone”.
These affirmations are consistent with the idea that gender incongruence responds to multiple etiologies, that these may be unique to each case, and that therefore, not everyone benefits from gender-affirming medical care as a first-line treatment. Understanding the etiology of GI would help clinicians decide which type of intervention will be helpful in each case. Moreover, considering that the cause of some regrets may be due to “excessive and hasty medicalization”, it is possible that this may also help in the prevention of detransition.
From: Age of first experience of gender incongruence among transgender and non-binary individuals. Jeong Won Oh et al. 2023. Obstetrics and Gynaecology Science.
Gender identity is an individual’s intrinsic sense of being male, female, or an alternative gender and is usually expressed in their gender role behaviour. Most people identify with the gender assigned to them and exhibit behaviours typical of their natal gender. However, very early in life, some people experience incongruence between their experiences and their assigned gender. The development of gender identity and expression is a multidimensional process that involves interactions among numerous factors, such as psychological, social, and biological factors. Although prenatal androgen exposure and specific genetic loci related to transmasculine identity and neuroanatomical regions, including the bed nucleus of the stria terminalis, have been identified as biological factors that influence sex development, their mechanisms remain unclear.
Knowledge of cognitive gender development in individuals with gender-variant identities at an early stage is limited. Children as young as 2 years may indicate that they are of another gender, expressing dislike for the gender associated with their natal sex and behave accordingly. Zaliznyak et al. reported that most transgender people first experience gender dysphoria at ≤7 years of age, persisting unaddressed for more than 20 years before commencing gender transition. Recently, 1.4% of youths aged 13–17 years in the USA were identified as transgender. Unaddressed gender dysphoria in childhood and adolescence may have adverse mental and physical health effects, as it does in adulthood.
Many transgender and non-binary individuals undergo the important process of social gender affirmation to pursue legal gender affirmation by changing the legal gender markers in their identification documents. Possessing a valid government identity document (ID) is necessary to access healthcare, open a bank account, and secure employment resources from which transgender individuals are excluded and marginalized. Legal gender affirmation protects transgender individuals from negative emotional responses, such as depression, anxiety, somatization, and global psychiatric distress.
Gender incongruence can develop early in life, given that gender learning begins early, with most children identifying their own and others’ genders within 18 and 24 months. One study found that 66.0% of transgender individuals had early onset in childhood compared to 34.0% with late onset after childhood in four countries that participated in the European network to investigate Gender Incongruence. Similar to previous surveys, we found that most transgender individuals experienced gender incongruence early in their lives. Although the mean age was 3–5 years older than that of Zaliznyak et al., the conceptualization of gender-related experiences is likely to be influenced by various factors such as age, race, culture, socioeconomic status, variations in language, and country, and was reported differently by the study, participants, and questionnaire.
Non-binary refers to gender-diverse people who experience and identify their gender as being outside the traditional gender binary of male or female. Many researchers either did not consider non-binary individuals as an independent group in the study population or excluded them from the sub-analysis of sex development owing to the small sample size. Most studies on transgender individuals have focused on transgender men and women, whereas non-binary individuals have largely gone unnoticed in health research. However, non-binary individuals comprise approximately 24.0% to over 50.0% of the gender-diverse individuals in recent studies.
In extensive population-based surveys in Brazil, non-binary identities were more common than binary transgender identities (1.2% vs. 0.7%). Given that gender-related experiences, intrapersonal progression, and expressions can differ between non-binary and transgender individuals, applying a binary-oriented identity narrative to understand the development of non-binary individuals may marginalize the unique experiences of this gender-diverse population.
A multidimensional gender spectrum should be included rather than a dichotomous categorization of gender identity. To the best of our knowledge, this study is the first to quantify the age of the first experience of gender incongruence in non-binary individuals and compare them with other transgender men and women. Non-binary individuals comprised 10.4% (35/337) of the transgender population in this study, and the mean age at which they first experienced gender incongruence was significantly older than that of transgender men and women (13.9 [non-binary] vs. 9.3 [transgender men] and 11.1 [transgender women], P=0.000).
While 5.3% of transgender men and 12.4% of transgender women first experienced gender incongruence after 16 years or older (after high school age), over 30.0% of non-binary individuals experienced incongruence first after 16 years or older. Non-binary individuals who do not belong to the binary transgender group may have limited resources and language to explore and articulate their gender identities in the community and in interpersonal relationships. Previous studies have found that invalidation experiences, such as non-binary identity is not “real” or is the result of a “phase,” with self-doubt, confusion, and rumination prevalent among non-binary adolescents, and some are unsure or ambivalent about their transgender identity.
In contrast, in another study, non-binary individuals reported significantly higher levels of gender and body satisfaction than binary transgender individuals. This intersectional complexity may contribute to the delayed identification of sex among non-binary individuals. Otherwise, 88.6% (31/35) of non-binary individuals in our study reported taking hormone therapy. Even though some non-binary individuals do not have an interest in medical treatment or feel unsure about their needs, others seek gender-affirming care to alleviate gender dysphoria or incongruence and increase body satisfaction through medically necessary interventions. The specific goals of care for non-binary individuals remain unclear. Still, the World Professional Association for Transgender Health recommends health care professionals provide information and gender-affirming medical interventions (GAHT or GAS) for non-binary individuals that affirm their experience of gender in their clinical guidelines.
Unaddressed gender dysphoria in childhood and adolescence may have adverse mental and physical health effects, as it does in adulthood. In contrast, non-binary children who were accepted for their identities by others and in their communities were generally well adjusted. Timely and appropriate interventions with or without medical support improved mental health outcomes and prevented the harmful effects of growing up with a body that was incongruent with one’s gender identity. Moreover, many studies have found that gender-affirming care, such as puberty suppression, GAHT, or GAS, appears to contribute significantly to the well-being of both binary and non-binary adolescents as well as adults. Almost none of the youths in adulthood regretted the decisions they had taken in adolescence.
One of the barriers to accessing GAHT for transgender adolescents is a lack of family approval. Some parents claim that their children’s gender dysphoria is simply an identity crisis common during growth that resolves over time. Other parents or caregivers found it difficult to accept the physical changes, and their reluctance stemmed from concerns about long-term side effects or the fear that their child would regret it later. Therefore, they did not allow their child to access medical care for GAHT. The lack of provider training and knowledge of transgender youths is an additional barrier. Health-care barriers may also lead to self-medication.
The findings of this study highlight the need for a change in social attitudes toward people with gender dysphoria. Social transition to match an individual’s affirmed gender has also improved psychosocial adjustment and well-being in transgender and non-binary individuals. This process can include actions such as changing names, providing appropriate bathroom/locker rooms or allowing them to use their suitable bathroom/locker rooms for them, communicating affirmed gender to others (on social media, school, or social contacts), and changing sex/gender markers in identification documents. The possession of government ID can be essential to general social life, and transgender individuals are at risk of harassment, assault, and other forms of adverse treatment if they present with an ID that does not match their gender.
From: Gender incongruence and gender dysphoria in childhood and adolescence—current insights in diagnostics, management, and follow-up. Claahsen-van der Grinten H et al. 2020. European Journal of Paediatrics.
Gender incongruence (GI) is defined as a condition in which the gender identity of a person does not align with the gender assigned at birth. Awareness and more social acceptance have paved the way for early medical intervention about two decades ago and are now part of good clinical practice although much robust data is lacking. Medical and mental treatment in adolescents with GI is complex and is recommended to take place within a team of mental health professionals, psychiatrists, endocrinologists, and other healthcare providers.
Gender identity and gender variation are frequently discussed in today’s modern society. Less than 50 years ago, the traditional roles of men and women were clearly defined. There was a taboo around topics such as homosexuality and gender incongruence. Nowadays, most Western societies are more open to variations in sexuality and gender identity. Gender identity refers to the identification of a person of being male, female, or neither/both [1]. Gender incongruence (GI) is defined as a condition in which the gender identity of a person does not align with the gender assigned at birth.
Persons with GI who experience significant burdens are in the DSM classification described as gender dysphoria (GD). Opposite to the binary approach of being male or female, the concept of gender becomes nowadays accepted as a continuum. The prevalence of GD in children and adolescence is reported to be 0.6–1.7% and depends on the selection of the study cohort, age, and method of investigation. In recent years, the number of children and adolescents seeking help with GI and GD has increased sharply and especially in children not all persons with GI represent with symptoms of GD. A remarkable change concomitant with the increase in referrals is a shift in the sex ratio of clinically referred adolescents, with more birth assigned girls now referred than birth assigned boys.
To date, the etiology of GI is still largely unidentified. Current research suggests that psychosocial and biological factors play a role in the development of GI. Indeed, there are findings that suggest there is a biological/anatomical base for GI: postmortem brain studies have shown that specific brain structures that are found to be different between men and women without GI show strong resemblance in volume and the number of neurons in people with GI to the gender one identifies. Recent studies have focused on brain connectivity between people with and without GI, showing differences in brain networks related to body image.
Research on the role of biological factors involved in the development of GI has mainly focused on genetic factors the role of (prenatal) sex hormones and differences in the brain. Genetic contribution in the development of GI has been demonstrated in twin studies, showing a high concordance of GI in monozygotic twin pairs and discordance of GI in dizygotic twin pairs, but true candidate genes have not yet been identified. Brain imaging studies have found support for the role of prenatal hormone (androgen) exposure in the development of GI. Various studies, in which various measures have been used, have shown that the brains of people with GI show resemblance to the brains of the gender they identify with and differences to the brains of the gender they were assigned with; the variations in findings are however large between studies,
See:
- Heylens G, De Cuypere G, Zucker KJ, Schelfaut C, Elaut E, Vanden Bossche H, De Baere E, T’Sjoen G (2012) Gender identity disorder in twins: a review of the case report literature. J Sex Med 9:751–757
- Klink DdHM (2013) Genetic aspects of gender identity development and gender dysphoria Springer US, New York
Psychiatric problems, such as internalizing problems, i.e., anxiety and depression, increased incidence of suicidal behaviours, and autism spectrum disorders are more prevalent in children and adolescents with GI. Therefore, the diagnostic sessions are also aimed to address these possible coexisting problems. Internalizing problems are thought to be reactive to feelings of GI and/or in response to social stigma. Many report being bullied.
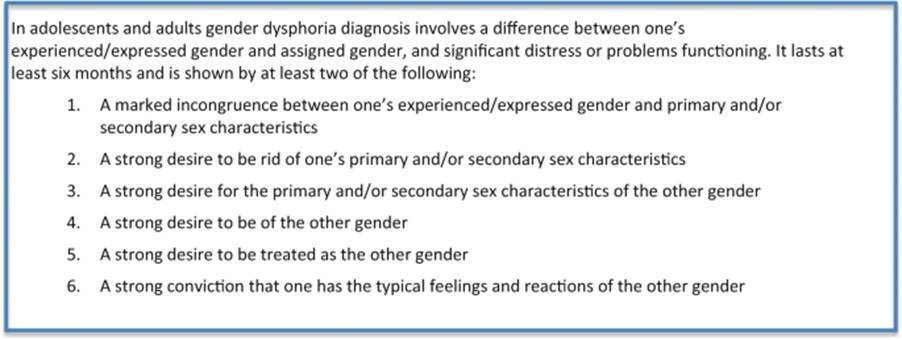
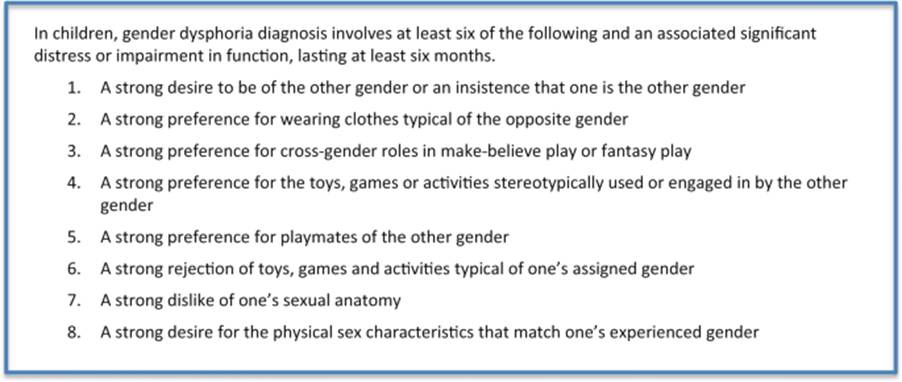
The development of their biological secondary sex characteristics is generally a highly distressful experience for adolescents with GI/GD that may lead to serious complaints of psychological functioning and behaviour. Therefore, pubertal suppression (PS) has been introduced in several expert centres to prevent or stop pubertal development [21] . It is well known that the use of long-acting GnRH analogous (GnRHa) to suppress gonadotropins can effectively prevent the progression of puberty.
See: Cohen-Kettenis PT, Delemarre-van de Waal HA, Gooren LJG (2008) The treatment of adolescent transsexuals: changing insights. J Sex Med 5:1892–1897.
Subsequent to GnRHa treatment, synthetic sex steroids are added to induce the development of sexual characteristics of the identified gender. There are generally two treatment regimes. When GnRHa treatment had started in an early Tanner stage, the “new” puberty is induced with a dosage scheme that is also common in prepubertal hypogonadal adolescents. Alternatively, when GnRHa treatment had started in physically matured persons and the duration of the hypogonadal state was limited, hormones can be started at a higher dose and more rapidly increased. An additional advantage of GnRHa treatment is that hormones do not have to be administered in supraphysiological dosages, which would otherwise be needed to suppress endogenous sex steroid production.
Surgery can address the primary or secondary sex characteristics with the aim to establish greater congruence with the experienced gender. Not every transgender or gender-incongruent individual seeks surgical interventions to change sex characteristics. The desire for an operation is for every transgender individual different.
To meet the needs of youth with GI, a multidisciplinary team is required and therefore we recommend that children and adolescents are to be followed by an experienced multidisciplinary team with access to a well-trained team of mental health professionals, psychiatrists, endocrinologists, gynecologists, surgeons, and other healthcare providers. A phased trajectory is generally preferred and starts with psychological assessment, followed by medical interventions. Endocrine treatment consists of two phases: first the start of GnRHa to prevent the development of pubertal development (a fully reversible intervention) followed by the addition of with gender-affirming hormones, which leads to irreversible changes. Although many details and aspects of this approach are still unknown, it is of great importance that youth with GI are provided with care that improves their well-being. While taking steps in this process, the benefits and possible harms of each intervention should be carefully balanced.
From: Gender Dysphoria and Gender Incongruence: An evolving inter-disciplinary field. Bourman W P, De Vries A, T’Sjoen G. 2016. International Reeview of Psychiatry.
The number of people with gender dysphoria and gender incongruence who seek assessment, support and treatment at gender identity clinic services has increased substantially over the years in Europe and North-America (Aitken et al. de Vries et al). There is also a significant increase in people who self-diagnose as having gender dysphoria and gender incongruence. Two recent population studies have aimed to estimate the prevalence of people who identify as such. Kuyper & Wijsen examined self-reported gender identity and dysphoria in a large Dutch population sample (N = 8064, aged 15–70 years old), and found that 4.6% of people assigned male at birth and 3.2% of people assigned female at birth reported an ‘ambivalent gender identity’ (defined as equal identification with other sex as with sex assigned at birth) and 1.1% of people assigned male at birth and 0.8% of people assigned female at birth reported an ‘incongruent gender identity’ (defined as stronger identification with other sex as with sex assigned at birth). Similarly, Van Caenegem et al. reported results based on two population-based surveys, one of 1,832 Flemish persons and one of 2,472 sexual minority individuals in Flanders, Belgium examining the prevalence of ‘gender ambivalence’ and ‘gender incongruence’. In the general population, gender ambivalence was present in 2.2% of male and 1.9% of female participants, whereas gender incongruence was found in 0.7% of men and 0.6% of women. In sexual minority individuals, the prevalence of gender ambivalence and gender incongruence was 1.8% and 0.9% in men and 4.1% and 2.1% in women, respectively.
The increase in prevalence of gender dysphoria and gender incongruence in the last decade is likely due to a number of interactively linked factors: the increased visibility of trans people on television and in cinema, such as for instance Caitlyn Jenner, Transparent, and The Danish Girl. Their screening make trans societal conscience as an increasingly mainstream phenomenon and is likely to contribute to at least a partial de-stigmatization of being trans; the wide availability of information on the Internet and other communication channels about gender dysphoria and gender incongruence, which also likely contributes to de-stigmatization; the increased awareness of the availability of biomedical treatment (Coleman et al. Wylie et al. and the development of societal tolerance towards trans individuals.
The significance of the increase in prevalence of gender dysphoria and gender incongruence should not be underestimated, which is likely to indicate the level of further future demand for clinical services. Governments, health insurance companies, national commissioning bodies of health services should work closely with gender identity clinic services, patient groups and other relevant stakeholders to ensure that adequate resources are allocated, that service planning is developed, and that training of high quality clinical and other staff is initiated.
International Organizations, such as the World Professional Association of Transgender Health (WPATH) and the European Professional Association of Transgender Health (EPATH), TransGender Europe (TGEU), Global Action for Trans* Equality (GATE) and the like, could play a vital role in setting minimum standards of care within a legal equality framework at national and supra-national political level.
In their review of mental health and gender dysphoria Dhejne et al. show that, although the levels of psychopathology and psychiatric disorders in trans people attending clinical services at the time of assessment are higher than in the cisgender population, they do improve following gender-confirming medical intervention, in many cases reaching normative values. They emphasise the need for a more robust measurement tool for gender and body dysphoria. Marshall et al. systematically review non-suicidal self-injury (NSSI) and suicidality in trans* people and conclude that they are at a greater risk of NSSI behaviour and suicidality than the cisgender population, and discuss the need to develop effective preventative interventions. V
an der Miesen et al. in their narrative review describe a frequent co-occurrence of Gender Dysphoria and Autism Spectrum Disorder, but also state that this co-occurrence does not necessarily preclude gender affirming treatment interventions. Jones et al. systematically review body dissatisfaction and disordered eating in trans* people and show that body dissatisfaction is core to the distress trans people experience and that this dissatisfaction may increase the risk of disordered eating in some individuals. These four papers thus confirm the vulnerability to mental health problems of this population. Future research must concern itself with the prevention of mental health problems, which predominantly include anxiety, depression and self-harming behaviour. Research must move beyond the narrative that trans people are a psychologically vulnerable group and focus on design and implementation of treatment programs, which tackle minority stress, discrimination and enhance legal protection and social support. Interventions aiming at improving the life of trans people, by involving significant others, in order to increase support for this population needs to be developed and evaluated.
Kreukels & Guillamon conclude with an exceptional and scholarly review of neuroimaging studies in people with gender incongruence. They describe studies into the etiology of feelings of gender incongruence, and studies that evaluate the effects of cross-sex hormone treatment on the brain. The growing body of research suggests evidence for the role of prenatal organization of the brain in the development of gender incongruence. Most importantly, their findings validate the feelings people with gender incongruence have and experience.
Key Literature References
*** Do hormones and surgery improve the health of adults with gender incongruence? A systematic review of patient reported outcomes (2025), by Kelsey Ireland, et al., published in ANZ Journal of Surgery
*** Gender Incongruence (2024), by Jack Drescher & Eric Yarbrough, published in Tasman’s Psychiatry
(Notable) *** Gender Dysphoria and Gender Incongruence (2024), by Diana Schellenberg & Michael Bombardier, textbook chapter in Psychopathology 6th Edition (eds. James E Maddux, Barbara A Winstead)
*** Depathologization of trans* experience in ICD-11: Suggestions for context-sensitive psychotherapeutic work (2024), by Kirsten Teren, published in Behavioral Sciences & The Law
(Notable) *** Etiology of gender incongruence and its levels of evidence: A scoping review protocol (2023), by Juan Pablo Rojas Saffie, published in PLOS One
(Notable) *** Age of first experience of gender incongruence among transgender and non-binary individuals (2023), by Jeong-Won Oh, et al., published in the journal Obstetrics & Gynecological Science
*** Gender incongruence and timing of puberty: a population-based cohort study (2022), by Anne H. Thomsen, et al., published in Fertility and Sterility
*** What is the most anticipated change induced by treatment using gender-affirming hormones in individuals with gender incongruence? (2021), by Naoya Masumori, et al., published in International Journal of Urology
*** Gender incongruence and gender dysphoria in childhood and adolescence—current insights in diagnostics, management, and follow-up (2020), by Hedi Claahsen – van der Grinten, et al., published in the European journal of Pediatrics
*** Gender Dysphoria and Gender Incongruence: An evolving inter-disciplinary field (2016), by Walter Pierre Bouman, et al., published in the International Review of Psychiatry
>> (Chapter 4) What research on nonbinary identity has been published in recent years, and why has the prevalence of people identifying as nonbinary dramatically increased over the past 10 years ?
Overview: (Under Development) by Scott Kerlin
Increasingly, there is a sizeable proportion of the population that identifies as nonbinary and has their own unique, specific treatment needs within transgender health.
Non-binary Identity
Bouman et al. (2023) recognize individuals who identify outside of the binary of male and female, but who may not have a physical intersex condition, generally termed ‘nonbinary’–as “individuals who may either embrace both male and female identities, feel more inclined towards one identity than the other, or do not identify with any of the binary gender identities. Generally termed ‘nonbinary’, these individuals may either embrace both male and female identities, feel more inclined towards one identity than the other, or do not identify with any of the binary gender identities. Others challenge the very notion of the existence of gender or do not experience gender identity at all (agender people). Terminology in this area is constantly changing as new identities are been described.”
Yu-Chi Wang, et al. (2025), in their study “Nonbinary Can Mean Different Things to Different People”, observe that “Nonbinary identities exist in direct opposition to the gender binarist pressure to adhere to strictly defined binary notions of gender, pressures reflected by the historical pathologization of gender diversity. by psychological and medical institutions (Galupo et al., 2017). There is no universal nonbinary experience.”
Salinas-Quiroz, et al. (2024) summarize, “The concept of cisnormativity (the societal assumption that everyone is cisgender, meaning their gender identity aligns with the sex they were assigned at birth) assumes that being cisgender is the default, universal gender modality. This perspective reinforces a narrow and exclusive understanding of gender diversity, systematically oppressing and overlooking the lived experiences of individuals whose gender identities do not match the gender that they were assigned at birth. Additionally, it reinforces the idea that trans and nonbinary identities are abnormal or deviant. This contributes to discrimination and prejudice against those who do not conform to cisnormative expectations. However, in the contemporary era, a more fluid and inclusive understanding of gender has emerged, acknowledging the diverse spectrum of gender identities beyond the confines of the binary. This more nuanced understanding of gender is already prevalent in gender nonconforming children aged 3–10. Further, they propose,
“We are using nonbinary as an umbrella term for someone who self-identifies as a gender outside the gender binary, and/or does not identify as always and completely being just a man or a woman, recognizing gender as existing along a spectrum. Some examples of nonbinary identities include being both a woman and a man, genderqueer or genderfluid identities that fluctuate, demigender identities that relate more to one gender than another without completely aligning with that gender, having two or three gender identities, two-spirit gender identities that are rooted in the spiritual and cultural beliefs of Indigenous communities in North America going beyond the traditional Western understanding of gender.”
Scandurra, et al. (2019) observe, “Transgender is an umbrella term referring to individuals who have a gender that differs from that normatively expected of their assigned sex [American Psychological Association (APA), 2015]. Not all transgender individuals have a binary identity, namely self-identifying as woman if they were male assigned at birth (MAAB) or man if they were female assigned at birth (FAAB). Indeed, the term non-binary and genderqueer (NBGQ) refers to individuals who have a gender identity that does not fall exclusively in man/male or woman/female normative categories. NBGQ individuals identify themselves with a neither exclusively masculine nor feminine gender, and their gender identity is situated beyond the gender binary, fluctuates between genders, or rejects the gender binary.
Prevalence of Nonbinary Individuals
Wilson & Meyer (2021) provide a major overview of nonbinary LGBTQ adults in the United States. They note that “about 11% of the LGBTQ adults (age 18-60 years) identify as nonbinary in terms of their gender. While non binary identified people are among both cisgender and transgender LGBTQ populations, they make up a larger proportion of the transgender population than of the cisgender LGBQ adult population.” They report from their surveys that that “the majority of nonbinary LGBTQ adults are young, urban, and born in the U.S. In terms of race/ethnicity identity respondents identified as White (58%) multiracial (16%), Latinx (15%), and Black (9%), and that most nonbinary LGBTQ adults did not identify as transgender. When asked about sexual identities, nonbinary respondents reported that they use a broad range of sexual identity terms—a majority reported queer (31%), bisexual (17%), pansexual (17%), or asexual (14%) identities.”
Bouman et al. (2023) in their UK study of nonbinary gender identities in the United Kingdom, report that the Census 2021 of the Office of National Statistics included a question on gender identity asked of those aged 16 years and over to provide the first official data on the size of the transgender population in England and Wales. The question asked ‘Is the gender you identify with the same as your sex registered at birth?‘. In total, 45.4 million (93.5%) answered ‘Yes’ and 262,000 (0.5%) answered ‘No’. Within the latter group, 118,000 (0.24%) answered ‘No’ but did not provide a write-in response; 48,000 (0.10%) identified as a trans man; 48,000 (0.10%) identified as a trans woman; 30,000 (0.06%) identified as nonbinary; 18,000 (0.04%) wrote in a different gender identity. The remaining 2.9 million (6.0%) did not answer the question on gender identity. It would seem that a careful estimate suggests that at least 0.1% of the population in England and Wales identifies as nonbinary according to our definition of non-binary, which amounts to 48,000 people of 16 years and over. Our findings and observations affirm that the concept of gender identity as a binary entity does not reflect reality and without this affirmation these important realities remain invisible.”
Research with Nonbinary Individuals
Di Giannantonio, et al. (2024) observe that “research with nonbinary people has been growing steadily and studies examining identity milestones in nonbinary individuals reveal a great diversity in the paths to self-awareness of one’s gender identity.” Research indicates a continuous increase in the numbers of nonbinary people, with rates among transgender or gender diverse populations ranging from 20% to 52%, and in the general population, with higher prevalence among individuals assigned female at birth (AFAB) who identify as nonbinary, ranging from 2% to 9%.
“Unlike transgender woman and men who typically become aware of their gender identity in the early stages of puberty or younger, many nonbinary individuals tend to gain awareness of their nonbinary identity in later
adolescence or early adulthood. This delayed discovery is attributed to a lack of social references to nonbinary identities, resulting in highly individualized developmental trajectories and significant variability in outcomes.
“For individuals with nonbinary identities, processes of identity awareness involve a complex relationship with defining one’s identity in relation to their own body. While experiences of gender dysphoria in transgender men and women often arise from bodily perceptions of incongruence, nonbinary individuals usually trace their genderdysphoria back to social aspects—namely invisibility and a lack of recognition.”
Schudson & Morgenroth (2023) have conducted substantial psychological research on non-binary identities. They point out: “Non-binary identities are gender and/or sex identities (gender/sex) that are not exclusively female or male. They can be comprised of elements of femaleness and/or maleness or exist outside of female and male. Some non-binary identities (e.g., agender) might involve not having a gender identity at all or rejecting aspects of gender/sex as a social category more broadly. Non-binary identities are sometimes conceptualized as falling under a broader transgender umbrella, which encompasses gender/sex identities that diverge from the gender associated with a person’s assigned sex at birth. However, non-binary people’s ways of conceptualizing their own identities are highly diverse, and some non-binary people do not identify as transgender, identify as cisgender to some degree, and/or describe themselves as neither transgender nor cisgender. In addition, not all people who locate their identity outside of the gender/sex binary use the term non-binary specifically to describe themselves, and might use other terms (e.g., genderqueer or gender diverse).
Research on non-binary people’s self-concepts
(per Schudson & Morgenroth (2023)) “Psychological research has historically excluded non-binary people’s self-understandings, and has often failed to identify non-binary participants in a sample due to binary-focused gender/sex measurement practices (e.g., survey items assessing gender/sex with “female” and “male” as the only response options). The dominance of these binary-focused practices has been a common impediment to the effective study of non-binary people’s identities and lives. Recent research has explored non-binary people’s self-concepts through their identity narratives, including how they describe their own gender/sex identities and how they understand gender/sex more broadly. Some research has examined similarities and differences between the experiences, identities, and perspectives of non-binary people and binary-identified trans people (i.e., trans women and trans men who do not identify as non-binary).
Non-binary people’s wellbeing
(per Schudson & Morgenroth (2023)) Much recent research on non-binary people’s mental health has used the minority stress model to examine how the broader contexts of systemic cissexism and binarism, along with intersecting forms of power (e.g., racism and misogyny), explain mental health disparities between non-binary people and binary-identified cisgender people. Some of this work has suggested that non-binary trans people might experience more minority stressors than binary-identified trans people, who are very commonly subjected to minority stressors.
Significant research has been conducted on mental health and well-being of nonbinary individuals in recent years. Wickham, et al. (2023) in their research with nonbinary individuals found a strong positive relationship between gender non-conformity and social well-being.
References Used: (Under Development)
Key Literature References
*** Understanding differences in types of social support and their effects on mental health over time for trans and nonbinary adults (2025), by Elioot Tebbe, et al., published in the journal Psychology of Sexual Orientation and Gender Diversity
*** “Nonbinary can mean different things to different people”: Nonbinary individuals’ internal gender conceptualizations and external navigation and negotiation of gender binarism (2025), by Wang, Y.-C, et al., published in the journal Psychology of Sexual Orientation and Gender Diversity
*** Nonbinary people in the family context: a systematic review and meta-analysis (2025), by Chiara Commone, published in International Journal of Transgender Health
*** Doing and undoing gender: examining nonbinary and cisgender expression at work in the U.S. (2025), by Theresa R. Hernandez, et al., published in The International Journal of Human Resource Management
*** Barriers reported by nonbinary adults when accessing gender-affirming medical treatments: A systematic scoping literature review. (2024), by Christienne Javier, et al., published in the journal Psychology of Sexual Orientation and Gender Diversity
(Notable) *** “You’re free from just a girl or a boy”: Nonbinary children’s understanding of their gender (2024), by Fernando Salinas-Quiroz, et al., published in the International Journal of Transgender Health
(Notable) *** “The third table where I would sit comfortably”: Narratives of nonbinary identity routes (2024), by B. Di Giannantonio, et al., published in the International Journal of Transgender Health
*** Being Not Binary: Experiences and Functions of Gender and Gender Communities (2024), by Heidi M. Levitt, et al., published in the journal Sex Roles
*** “It’s like a happy little affirmation circle”: a grounded theory study of nonbinary peoples’ internal processes for navigating binary gender norms (2024), by Katelyn O Coburn, et al., published in the International Journal of Transgender Health
(Notable) *** Nonbinary Gender Identities (2023), by Walter Pierre Bouman, et al., published in the journal Best Practice & Research Clinical Obstetrics & Gynecology
*** Gender-affirming endocrine care for youth with a nonbinary gender identity (2023), by Juanita K. Hodax, et al., published in Therapeutic Advances in Endocrinology and Metabolism
*** Invalidation and Mental Health Among Nonbinary Individuals (2023), by Kelly C. Johnson, et. al, published in the journal Psychology of Sexual Orientation and Gender Diversity
(Notable) *** Non-binary Gender/sex Identities (2023), by Zach C. Schudson & Thekla Morgenroth, published in the journal Current Opinion in Psychology
*** Non-binary Experiences in the Context of Gender Dichotomization: A Qualitative Systematic Review (2023), by Chyna (C.J.) Parker, unpublished doctoral dissertation, Pepperdine University
(Notable) *** Gender Identification Beyond the Binary and Its Consequences for Social Well-Being (2023), by Miriam Ines Wickham, et al., published in Archives of Sexual Behavior
*** Non-Binary Clients’ Experiences of Psychotherapy: Uncomfortable and Affirmative Approaches (2022), by Fau Rosati, et al., published in the International Journal of Environmental Research and Public Health
*** Non-Binary Gender Identity Development: A Qualitative Study (2022), by Trevor Waagen, unpublished PhD dissertation, University of North Dakota
*** ‘The Default is Just Going to be Getting Misgendered’: Minority Stress Experiences Among Nonbinary Adults (2022), by Em Matsuno, et. al, published in the journal Psychology of Sexual Orientation and Gender Diversity
*** Interactions Between Blending and Identity Concealment: Effects of Non-binary People’s Distress and Experiences of Victimization (2021), by Sana Flynn and Nathan Grant Smith, published in the Public Library of Science (PLOS)
*** “There is Nothing to Do About It”: Nonbinary Individuals’ Experience of Gender Dysphoria (2021), by M. Paz Galupo, Lex Pulice-Farrow, and Emerson Pehl, published in the journal Transgender Health
*** Psychological Functioning in Non-binary Identifying Adolescents and Adults (2021), by Nastasja M. de Graaf, et al., published in Journal of Sex & Marital Therapy
(Notable) *** Nonbinary LGBTQ Adults in the United States (2021), by Wilson, Bianca D.M., & Meyer, Ilan H., published by UCLA: The Williams Institute
(Notable) *** Health of Non-binary and Genderqueer People: A Systematic Review (2019), by Cristiano Scandurra, et al., published in Frontiers in Psychology
*** Non-binary/Genderqueer Identities: a Critical Review of the Literature (2017), by Emmie Matsuno & Stephanie L. Budge, published in Current Sexual Health Reports
>> (Chapter 5) How have overall measures of gender identity evolved over time? What is the concept of “diversity in gender identity development”?
Overview: As the study of gender identity itself has evolved for many years, so have the variety of measures themselves. Below is a variety of reports which shed light on the most essential areas of investigation. Of particular emphasis is Ellena Fisher’s 2024 study, “What do measures of gender identity tell us about gender identity over time?“.
From “Development and validation of novel measures of gender minority stress for transgender and nonbinary people.” Puckett et al. [2025] International Journal of Transgender Health
Transgender and nonbinary (TNB) people experience a myriad of minority stressors that drive health disparities. Minority stress refers to the additional stress that marginalized groups experience, above and beyond the general stressors that anyone may encounter. The minority stress model was originally proposed to help explain the mental health disparities experienced by cisgender lesbian women and gay men. This model was later adapted to better include the experiences of TNB people with two primary changes. One notable change was the addition of gender non-affirmation as a distal stressor (which includes experiences of misgendering). This refers to when a person’s gender is invalidated by others, such as when referred to with the wrong pronouns, gendered terms, and other dynamics that incorrectly gender a TNB person.
A plethora of research shows that these minority stressors are associated with worse mental health outcomes. Given the importance of the minority stress model to framing future research on the drivers of health disparities experienced by TNB people, there is a clear need to continue advancing our understanding of TNB-specific forms of minority stress.
There are various stressors that can arise at the interpersonal level, in response to cultural norms around gender and the broader sociopolitical context. For example, TNB people may experience body/gender policing. This stressor refers to when others try to enforce gender norms, behaviours, or other expectations onto TNB people in attempts to force them into a particular gender expression or experience. In addition, felt stigma may be experienced as perceiving uneasiness from others and bodily vigilance.
From: “What do measures of gender identity tell us about gender identity over time?” Fisher E, Wright S, Sargeant C. [2025] British Journal of Developmental Psychology.
Gender-diverse individuals have been present throughout history and experiences outside of the gender binary are found in cultures around the world. However, contrasting assumptions about the nature of ‘gender’ have led to the pathologisation of gendered expressions that do not align with Westernized cultural stereotypes. Over time, there has been a move towards an affirmative model of care for gender-diverse individuals (American Psychological Association and practitioners have been encouraged to recognize and accept varied gender expressions as a part of human diversity.
Conceptual understandings of gender fall into 3 categories: (1) evolutionary understandings based on biological sex, (2) social structural approaches based on societal norms and structures, and (3) social identity approaches based on gender as a social category with which an individual identifies. Across the research literature, ‘sex’ is often used to refer to the biological characteristics of an individual (e.g., chromosomes), while ‘gender’ typically refers to the societal and cultural meanings associated with femininity and masculinity. The term ‘transgender’ is operationalized by Lindqvist et al. as ‘individuals whose assigned gender at birth does not correspond to their self-defined gender identity’. These ‘assigned genders’, given to infants at birth, are often based on a dichotomous binary categorization of gender and sex.
With rising numbers of individuals whose experience cannot be defined using these binary categories, theories of gender identity have broadened, reflecting ideas of gender as a spectrum. Viewing gender as a societal construct rather than a characteristic determined by biological sex has led to an affirmative model of care being used internationally with gender-diverse individuals, supporting an individual to consolidate their expressed gender.
Measures of gender identity
In line with broadening theories and models of gender, a diverse range of measures have been developed to attempt to understand the multifaceted nature of gender identity. Bates et al. note that these measures often focus on a person’s internal understanding of their own gender, as well as their gender expression and how this is perceived by others. A biosocial model of gender in which an individual’s gendered psychological attributes ‘emerge flexibly from a dynamic interaction among biological and social factors’.
Self-identification
Self-identification measures of gender identity are based on the descriptive categorization of self rather than interpretative accounts of personality or behavioural traits. Many researchers have attempted to explore the age at which a child is able to recognize their own gender and notice the gender of others in order to make this ‘summary judgement’, suggesting that children generally are able to label their own gender by the age of 2.
Intergroup bias
Another means of understanding a child’s gendered experience is to explore sex segregation or intergroup bias. This is referred to by Kornienko as a ‘between-gender’ measure. Social identity theory suggests that members of any group see their group as distinct from outgroups and the sense of belonging felt by a group member will automatically lead to in-group bias.
Gender stereotyped preferences
With some children not developmentally able to self-identify at an early age, many researchers also use observational methods or parental reports of children’s stereotyped preferences. Modern models of gender identity are based on early research suggesting that separate dimensions of masculinity and femininity are useful tools in understanding overall gender identity. The personality traits and preferences associated with each of these dimensions are universally accessible and used frequently by social perceivers.
Comparison of trajectories in transgender and cisgender children and young people.
When exploring the experiences of transgender children and young people, many researchers have found evidence to suggest that transgender children show very similar patterns of development to control groups of children of their expressed gender. Across a variety of measures, Rae et al. found that this similarity was present regardless of whether a transgender child had been able to socially transition. Although stronger cross-sex identification was found to be predictive of later social transition and persistence of gender dysphoria, the scores that children obtained using these measures prior to transitioning did not differ significantly from those who had transitioned already or to a control group of their expressed gender. These preferences may be influenced by a combination of biological factors and a child’s early experiences and interactions with adults.
With so many children demonstrating gender identities incongruent with biological sex, it appears that neither nature nor nurture can fully explain this essentialist quality. As children develop and learn about the societal expectations and stereotypes attached to gender, an individual’s gendered experience seems to remain stable over time, even when this does not match cultural and societal expectations. Attempts to inhibit gender identity to fit within the prominent binary systems and structures can have a negative impact on psychological outcomes.
From: “A critical discussion of paediatric gender measures to clarify the utility and purpose of ‘measuring’ gender. Strauss P. et al. [2024]. International Journal of Transgender Health.
Why do gender clinics and researchers continue to use gender measures? Is it truly meaningful or useful to attempt to quantify, categorize, or systematically clarify gender identity or gender dysphoria, using standardized measures, at any age? Do gender measures serve to perpetuate the pathologization of diverse gender identity? Which measures are most useful and least harmful? Are any current measures ideal for use? What would be the ideal properties of a pediatric gender measure, and how would it best be developed? These are questions that we suggest clinicians and researchers reflect on when choosing whether to use a gender measure, which measure to use, and in the development of gender measures.
Considering inclusivity
Trans people are often aware that dominant narratives of binary gender identity may more readily result in access to gender-affirming medical care, which may have implications for how young people respond to measures. Many measures are founded on outdated cisnormative and heteronormative conceptualizations of male and female gender: for example, many do not accommodate the possibility of trans male/masculine people having feminine gender expression. An increasing number of young people who identify as non-binary are presenting to paediatric gender clinics, so there is a clear requirement for inclusive gender measures. Thus, all measures separated into male/female versions should now be used with caution. Some newer measures aim to be inclusive of diverse gender identities. It is likely that the more a measure reflects the diverse reality of gender experience, the more likely the young person is to feel understood and express their thoughts and feelings openly, creating a good foundation for a clinical relationship as well as more accurate data.
Conclusion
Gender diversity is increasingly recognized as part of a spectrum of human variation, and many people do not believe it is appropriate to classify gender difference. Throughout this paper, evaluating the purpose and utility of each measure has remained central. There is a need for broader clinical and cultural investigation: are gender measures necessary in the gender-affirming care of trans young people? Trans researcher and community involvement in the development and validation of newer, more ideal measures would enable gender clinics to reduce reliance on older measures. It would be informative to explore clinicians’ perceived utility of measures, over and above asking the young person to self-identify and describe their experience of gender in a structured way. We encourage clinical teams and researchers to actively reflect upon, and periodically review, the measures they administer. Most pertinently, any current clinical or research use of measures that frame trans people as abnormal, use discriminatory language, or measure only distress without measuring wellbeing and euphoria, needs urgent reevaluation.
From: “The Gender Self-Report: A Multidimensional Gender Characterization Tool for Gender-Diverse and Cisgender Youth and Adults.” Strang J. et al. [2023]. The American Psychologist.
Gender identity is a core component of human experience, critical to account for in broad health, development, psychosocial research, and clinical practice. Yet, the psychometric characterization of gender has been impeded due to challenges in modelling the myriad gender self-descriptors, statistical power limitations related to multigroup analyses, and equity-related concerns regarding the accessibility of complex gender terminology. Therefore, this initiative employed an iterative multi-community-driven process to develop the Gender Self-Report (GSR), a multidimensional gender characterization tool, accessible to youth and adults, nonautistic and autistic people, and gender diverse and cisgender individuals. Two stable factors emerged: Nonbinary Gender Diversity and Female–Male Continuum (FMC). FMC was transformed to Binary Gender Diversity based on designated sex at birth to reduce collinearity with designated sex at birth. Differential item functioning by age and autism status was employed to reduce item–response bias.
From: “Between a boy and a girl: Measuring gender identity on a continuum.” Gülgöz S, et al. [2022] Social Development.
Studies of gender development typically use binary, discrete measures of identity. However, growing literature indicates that some children might not identify with a binary gender. We tested a continuous measure of felt gender identity with gender-nonconforming children, socially-transitioned transgender children, cisgender siblings, and unrelated cisgender children. In two studies, we found that transgender and cisgender children did not differ in their degree of identifying as their current gender, that they showed more binary identities compared to gender-nonconforming children, and that the continuum was a valid predictor of other measures of gender development
Consistent with prior research using categorical measures of gender identity, the current work shows that transgender children, cisgender siblings and unrelated cisgender children do not differ in the extent to which they identify as their current gender on a spectrum measure of gender identity. Moreover, neither cisgender nor transgender children identified exclusively as their current gender, which suggests that continuous measures might provide more nuanced representations of children‘s gender identities. These results lend support to the growing recognition that binary gender categories might not fully reflect how individuals identify.
Finally, questions remain on whether different gender identity measures used in the field tap into the same or similar constructs. Related to this issue of how gender should be conceptualized and measured by researchers, some have theorized that gender identity is better conceptualized not as a stable trait but as a fluid construct that varies contextually.
From: “Under-Representation of Transgender Identities in Research: The Limitations of Traditional Quantitative Survey Data.” Ghorbanian A et al. [2022]. Transgender Health.
Research indicates that the portrayal and representation of transgender individuals within society, or lack thereof, impact the way in which they are able to reconcile their gender identity. Quantitative research methodology often requires that participants select one identity label from a limited list for each identity characteristic (e.g., race, sexual orientation, and relationship status). The process of choosing from limited items that do not represent one’s identities limits our understanding of the nuances of identity and may create minority stress for the participant.
The nuance of transgender identities may not be adequately captured by standard demographic research methodologies and research would benefit from ongoing revision of demographic response options informed by the literature. Through the process of acknowledging and validating less visible identities, transgender individuals will be better represented and understood by researchers. Psychological research and its methodologies have the power to either reinforce societal oppression or propel us forward by prioritizing inclusivity and representation of diverse identities.
From: “Measuring Satisfaction and Comfort with Gender Identity and Gender Expression among Transgender Women: Development and Validation of the Psychological Gender Affirmation Scale.” Sevelius J, et al., [2021] International Journal of Environmental Research and Public Health.
Among transgender and gender diverse people, psychological gender affirmation is an internal sense of valuing oneself as a transgender or gender diverse person, being comfortable with one’s gender identity, and feeling satisfied with one’s body and gender expression. Gender affirmation can reduce gender dysphoria and mitigate deleterious health effects of marginalization.
Gender identity is an internal felt sense of one’s gender, while gender expression is how a person presents their gender to the external world. Transgender and gender diverse people have a gender identity and/or expression that differs from the sex they were assigned at birth, whereas cisgender (i.e., non-transgender) people’s gender identity and expression align with their assigned birth sex. Further, some transgender people experience gender dysphoria, defined as psychological distress associated with a sense of incongruence between their gender identity and gender expression and/or body and physical appearance. Gender dysphoria is compounded by transphobia—the systemic stigma and discrimination faced by transgender people—which often results in social and economic marginalization as well as violence. Experiences of transphobia are also significantly associated with poorer mental health and substance use among transgender and gender diverse people. Social gender affirmation is interpersonal recognition and respect for one’s gender identity, while medical gender affirmation entails the utilization of gender-affirming medical treatments, such as hormone therapy and/or surgeries.
Psychological gender affirmation is also a distinct concept from gender congruence, in that gender congruence indicates whether a person feels that their external appearance, or gender expression, is aligned with their gender identity, whereas psychological gender affirmation represents a felt sense of comfort and satisfaction with one’s identity and appearance, regardless of perceived alignment of one with the other.
From: “What is gender, anyway: a review of the options for operationalising gender.” Lindqvist A, et al.[ (2021) Psychology and Sexuality.
In the social sciences, many quantitative research findings as well as presentations of demographics are related to participants’ gender. Most often, gender is represented by a dichotomous variable with the possible responses of woman/man or female/male, although gender is not a binary variable. It is, however, rarely defined what is meant by gender
Gender as consisting of several aspects, which can be divided into the four main facets of: (a) physiological/bodily aspects (sex); (b) gender identity or self-defined gender; (c) legal gender; and (d) social gender in terms of norm-related behaviours and gender expressions (the American Psychological Association refers to this aspect as ‘sex role’;. These aspects may change over a life-time, due to external impact, such as from society. A simple way is to ask the participants about how feminine and masculine they see themselves, and how feminine and masculine they believe others see them.
From: “The Transgender Identity Survey: A Measure of Internalized Transphobia.” Bockting W, et. al, [2020] LGBT Health.
Gender norms are deeply embedded in society, and perceived transgressions of these norms are generally met with resistance. This is seen in the ridicule, bullying, and rejection experienced by gender nonconforming children and adolescents, and it is reflected in the enacted stigma (actual experiences of discrimination) and felt stigma (perceived rejection and expectations of being stereotyped or discriminated against) reported by transgender people. Transgender and gender nonconforming (TGNC) people are a diverse group of individuals whose gender identity and/or expression differs from the sex they were assigned at birth. Transgender individuals may internalize gender norms and expectations, and they may develop shame and self-hatred because of their lack of conformity to culturally established definitions of maleness and femaleness, manhood and womanhood, or masculinity and femininity.
The TIS reliably measures internalized transphobia and its four dimensions of Pride, Passing, Alienation, and Shame. We found positive associations between the TIS and measures of gender identity, role, and ideology, consistent with the definition of internalized transphobia as stemming from the internalization of prevailing binary conceptualizations of gender, which for many transgender individuals fails to account adequately for their lived experience. Confronting internalized transphobia often involves working toward acceptance of ambiguity in gender identity and role, challenging traditional ideology. Future research should explore the causes and correlates of each of the four dimensions of internalized transphobia, furthering our understanding of minority stress and its impact on identity development and health.
Key Literature References
*** The Case for “Other”: Measuring Gender and Sexual Identity in Survey Research (2025), by Christina Pao, et al., published in Sociology Compass
(Notable) *** Development and validation of novel measures of gender minority stress for transgender and nonbinary people (2025), by Jay A. Puckett, et al., published in the International Journal of Transgender Health
(Notable) *** What do measures of gender identity tell us about gender identity over time? (2025) by Ellena Fisher, et al., published in the British Journal of Developmental Psychology
*** Gender identity and mental health inequalities 2001–2022 population-level evidence from an Australian cohort study (2025), by Karinna Saxby, et al., published in BMJ Mental Health
*** Diverse Gender Identity Development: A Qualitative Synthesis and Development of a New Contemporary Framework (2024), by Molly Speechley, et al., published in the journal Sex Roles
(Notable) *** A critical discussion of pediatric gender measures to clarify the utility and purpose of “measuring” gender (2024), by Penelope Strauss, et al., published in the International Journal of Transgender Health
*** Measurement opportunities for studying sexual and gender diverse partnerships in population-based surveys (2024), by Christopher A. Julian, et al., published in Journal of Marriage and Family
*** Beyond Wokeness: Why We Should All Be Using a More “Sensitive” Measure of Self-Reported Gender Identity (2023), by Melissa Marcotte, et al., published in Psychological Reports
(Notable) *** The Gender Self-Report: A Multidimensional Gender Characterization Tool for Gender-Diverse and Cisgender Youth and Adults (2023), by John F. Strang, et al., published in The American Psychologist
*** The Measurement of Gender Expression in Survey Research (2023), by Dana Garbarski, published in the journal Social Science Research
(Notable) *** Exploring Current Gender Meanings: Creating a New Gender Identity Scale (2023), by Jan E. Stets, et al., published in Advancing Identity Theory, Measurement, and Research
*** Demographics and gender‑related measures in younger and older
adolescents presenting to a gender service (2023), by Marijn Arnoldussen, et al., published in European Child & Adolescent Psychiatry
(Notable) *** Between a boy and a girl: Measuring gender identity on a continuum (2022), by Selin Gülgöz, et al., published in the journal Social Development
*** Measuring Sex, Gender Identity, and Sexual Orientation (2022), by Becker T, Chin M, Bates N, from the textbook Measuring Sex, Gender Identity, and Sexual Orientation
(Notable) *** Under-Representation of Transgender Identities in Research: The Limitations of Traditional Quantitative Survey Data (2022), by Ariann Ghorbanian, et al., published in Transgender Health
(Notable) *** Measuring Satisfaction and Comfort with Gender Identity and Gender Expression among Transgender Women: Development and Validation of the Psychological Gender Affirmation Scale (2021), by Jae M. Sevelius, et al., published in International Journal of Environmental Research and Public Health
(Notable) *** What is gender, anyway: a review of the options for operationalising gender (2021), by Anna Lindqvist, et al., published in Psychology & Sexuality
*** Evaluating the Use of a Two-Step Gender Identity Measure in the 2018 General Social Survey (2021), by Danya Lagos & D’Lane Compton, published in Demography
(Notable) *** The Transgender Identity Survey: A Measure of Internalized Transphobia (2020), by Walter O. Bockting, et. al, published in LGBT Health
*** The Gender Identity Scale: Adapting the Gender Unicorn to Measure Gender Identity (2019), by Felicity Ho & Alexander Mussap, published in the Psychology of Sexual Orientation and Gender Diversity
*** Gender Congruence and Body Satisfaction in Nonbinary Transgender People: A Case Control Study (2019), by Bethany A. Jones, Walter Pierre Bouman, Emma Haycraft, and Jon Arcelus, published in the International Journal of Transgenderism
*** The Terminology of Identities Between, Outside and Beyond the Gender Binary–A Systematic Review (2019), by Nat Thorne, et. al, published in the International Journal of Transgenderism
*** Transforming the Paradigm of Nonbinary Transgender Health: A Field in Transition (2019), by Joz Motmans, Timo O. Niedler, & Walter Pierre Bouman, published in the International Journal of Transgenderism
>> (Chapter 6) What is the current status of gender identity research with children and youths?
Author: Robert L.P. Klaehn, MD, DFAACAP
Part 1: Introduction
The current research on gender development indicates that gender identity begins to form around two years of age, when many children begin to notice the physical differences between boys and girls. In “Embracing Diversity: Developing a Gender Identity,” the infant and toddler mental health organization, Zero-to-Three (Now, Zero-to-Five) discusses the basics of gender development:
“At first, their definitions of their definitions of ‘boys and girls’ are hazy at best. Just as they might claim that any animal with four legs is a doggie, they may believe that any person who wears a blue shirt and has short hair is a boy…
Most kids begin to strongly identify with a gender around age 3, whether they are cisgender (when their biological sex matches their identity), transgender (when there biological sex does not match their identity), or somewhere in between. It’s very common for young children to try on different roles, pretending to be a princess one day and a prince the next.
What is different for transgender children? Trans kids are likely to be ‘persistent, consistent, and insistent” – clear and certain that they’re not the gender those around them think they are. Recent research suggests that about 1 in every 100 adults in the US identify as transgender….”
What advice do these infant and toddler mental health specialists have in supporting young children developing their gender identity?
“Make sure that your child knows that they have your support.”
“Be aware that gender stereotypes may even start before your baby is born.”
“Offer children a range of toys and experiences, including toys that some may think cross gender lines.”
“Be clear about your family’s values: “In our family, anyone can play with any toy. It doesn’t matter what your gender is” and “Jason has two parents who love him very much, just like you. He has two dads. You have a mom and a dad.”
“As children grow, apply a gender-neutral approach to daily chores and family
responsibilities.”
“Read stories that feature all kinds of families, as well as stories that include
transgender, non-binary, and gender expansive characters. Shared reading is a
powerful way for all families to nurture an inclusive worldview and challenge
stereotypes from the start.”
“Build an inclusive community. This is important for all kids, and it’s especially
important for kids who may later identify as LGBTQ. In the past, one of the
toughest things for kids discovering that their sexual orientation or gender
identity was different than those around them was a feeling of being alone…
Make it clear that all people are welcome in your community and in your
household. Living your values in this way shows your child that they will be
loved however they show up and whoever they become.” (Zero-to-Three, 2021)
Gulgoz and their colleagues (2019) looked at the similarities in gender development between transgender and cisgender children in a cohort of 317 children (including 208 transgender girls) between 3 and 12 years old, “who, in early childhood, are identifying and living as a gender different than their assigned sex.” Like the gender development in cisgender children, they found that:
“…Transgender children strongly identify as members of their current gender group and show gender-typed preferences and behaviors that are strongly associated with their current gender, not the gender typically associated with their sex assigned at birth.”
“…Children develop a sense of identity at an early age, that this identity is not
necessarily determined by sex assigned at birth, and that children my hold onto
this identity even when it conflicts with others’ expectations.
“…Our findings also demonstrate that once a child is living in line with an identity different from the one they were assumed to have at birth and were initially socialized to have, they are likely to show the same patterns of gender development as a child who develops a gender aligning with their assigned sex and socialization.”
Lisa Diamond (2020) reports that that an increasing number of children and youth have gender identities that are different from their assigned sex at birth:
“A growing number of children and adolescents describe themselves as transgender, gender fluid, or nonbinary, meaning that their gender identities or expressions differ from their birth-assigned gender. In a recent population-based study of more than 80,000 ninth and eleventh graders in Minnesota, 3% of youth viewed themselves as transgender, genderqueer, gender fluid, or unsure of their gender identity (Rider, et al (2018) cited in Diamond).
Part 2: Assessment
There is a lack of clarity regarding the purpose of the initial psychiatric evaluation of gender diverse children and youth. Levine (2024) states:
“A fundamental question is emerging within the arena of trans health care. What is the purpose of the comprehensive psychiatric evaluation (CPE) for trans-gender identified children and adolescents?” There are two opposing answers, both of which have the same goal of improving the patients’ mental health and social function. The gender affirmative one, favored by the many desperate young patients and many for the sequence of social transition,
hormones, and surgery based on patients’ desires (Coleman et al., 2022, cited in
Levine, 2024). The more recent answer, favored by many parents, anxious minors, and a growing number of mental health professionals is to clarify what is occurring to create an efficient focus for a psychotherapy.” (Genspect, 2023, cited in Levine, 2024).
In 2024, the European Academy of Pediatrics (EAP) published a statement on clinical management of children and adolescents with gender dysphoria and made the following recommendations:
- EAP recognizes that in different countries, there will be a variety of approaches to this complex issue.
- EAP recommends an individual rights-based analytical approach to caring for young people with gender dysphoria.
- This is a rare condition, referral to fully funded expert pediatric centers is necessary to develop the specialist services we recognize deliver the optimal care for young people and their families.
- EAP urges urgent research into the optimal approach to supporting young people with gender dysphoria and their families.
- Pediatricians or other physicians (i.e., GP/family doctors) who care for children and adolescents should support those with gender dysphoria, which includes directing them to a multidisciplinary team of experts and providing ongoing primary and tertiary care support.
- Thus, pediatricians and all healthcare professionals treating children and adolescents should be well-trained on gender issues.
- EAP suggests there should be further understanding, not controversy, in gender dysphoria.
However, there is not a consensus on the adequacy of current clinical guidelines. Jo Taylor and their colleagues (2024) conclude that:
“Most clinical guidance for managing children/adolescents experiencing gender dysphoria/incongruence lacks an independent and evidence-based approach and information about how recommendations were developed. This should be considered when using these to inform service development and clinical practice.”
Clearly, continued research and consensus building is needed.
Part 3: Co-occurring conditions in children and youth with gender dysphoria/incongruence
A recent study by Nicolas Suarez and others at the Centers for Disease Control (2023) shows that there are multiple disparities between the mental health status of Transgender and Gender Diverse (TGD) high school students and ess than their cisgender peers. From the abstract:
“…Until recently, population-based data describing the experiences of transgender students and students questioning whether they are transgender (questioning) have been limited. In 2023, the national Youth Risk Behavior Survey assessed transgender identity, providing the first nationally representative data about transgender students. This report describes the demographic characteristics of transgender and questioning high school students and examines differences in the prevalence of experiences of
violence, poor mental health, suicidal thoughts and behaviors, school connectedness, and unstable housing among transgender, questioning, and cisgender high school students nationwide.
In 2023, 3.3% of U.S. high school students identified as transgender, and 2.2% identified as questioning. Transgender and questioning students experienced a higher prevalence of violence, poor mental health, suicidal thoughts and behaviors, and unstable housing, and a lower prevalence of school connectedness than their cisgender peers. Compared with 8.5% of cisgender male students, 25.3% of transgender students and 26.4% of questioning students skipped school because they felt unsafe. An estimated 40% of
transgender and questioning students were bullied at school, and 69% of questioning students and 72% of transgender students experienced persistent feelings of sadness or hopelessness, a marker for experiencing depressive symptoms. Approximately 26% of transgender and questioning students attempted suicide in the past year compared with 5% of cisgender male and 11% of cisgender female students.”
At the 2024 Annual Meeting of the American Academy of Child and Adolescent Psychiatry, (AACAP) Dr. Mehmet Kucuker and their colleagues presented a poster on the “Clinical Characteristics of Transgender and Gender-Diverse (TGD) Youth Presenting to a Psychiatric Emergency Department.” For their poster, they reviewed data from the medical records of 5- to 17-year-olds present to a pediatric psychiatric emergency room from March 2019 to November 2021. Their results and conclusions:
“TGD youth exhibited higher rates of psychiatric ED revisits, elevated suicidal risk at admission, longer ED stays, and higher numbers of co-occurring diagnoses at discharge. Moreover, TGD individuals were more prone to receiving diagnoses of disorders related to trauma, mood, anxiety, or adjustment disorders, as well as suicidal thoughts and behaviors (STBs). Interaction analyses showed that the risk of trauma-related disorders and STBs was unaffected by sex assigned at birth among TGD youth.
TGD youth showed more severe clinical presentations at the psychiatric ED compared to their cisgender peers. Sex assigned at birth did not influence the risk for STBs or trauma-related disorders. Further research is essential to understand the nuanced dynamics of psychiatric presentations among TGD patients in ED settings.”
In a very recent study, O’Shea and their colleagues (2025) assessed the risk factor that are associated with the higher prevalence of mental health disorders in sexual minority (those who do not identify as heterosexual, SM) and gender minority (who do not exclusively identify with the sex they are assigned at birth, GM) young people in ”a systematic review of systematic reviews and meta-analysis.” They found both proximal and distal risk factors for both the SM and GM groups.
Proximal risk factors for sexual minority (SM) young people include: “Maladaptive coping mechanisms/emotion regulation, Internalized homophobia/discomfort with sexual identity, Lack of openness about sexual orientation/stress associated with ‘coming out,’ Early frequent sexual activity, Internal religious conflicts [and] unmet medical needs.
Distal factors for SM youth include a: “Lack of closeness with and hostility from family members, Lack of support from friends/schools, Bullying, Victimization, Discrimination, Harassment, Micro- aggressions, Hostility from religious groups, Stressful life events, [and] Traumas experienced in childhood and adolescence.”
Proximal risk factors for gender minority (GM) young people include: “Negative coping mechanisms, Internalized transphobia, Low appearance congruence, Detectable HIV viral load, Drug use [and] Trading sex.” Distal factors for GM youth include: “Lack of acceptance/rejection from family, Lack of support from peers/schools, Victimization, Discrimination [and] Living in suburban area.”
Hull and their colleagues (2025) also found an increased incidence of non-suicidal self-injury (NSSI), suicidal ideation (SI) and suicide attempts (SA) in gender diverse youth. From the abstract:
“Data were drawn from the Adolescent Brain Cognitive Development Study, a longitudinal study of youth across the United States. Youth (n = 7909) were aged 10–11 during initial assessment, and follow-up was conducted one year later. Two dimensions of experienced gender, felt-gender incongruence (not feeling aligned with the gender associated with one’s sex assigned at birth) and gender non-contentedness (feeling dissatisfaction with the gender associated with one’s sex assigned at birth), were assessed.
For youth assigned female at birth, felt-gender incongruence was prospectively
associated with first-onset NSSI and SI and gender non-contentedness was
prospectively associated with first onset of NSSI. For youth assigned male at birth, gender non-contentedness was prospectively associated with first-onset SI. Diverse experienced gender did not prospectively predict suicide attempts.
They concluded that “Dimensions of experienced gender may be associated with subsequent first-onset self-injurious thoughts and behavior among preadolescents. These findings support the need for future research on risk and protective factors that may mediate or moderate this relationship.”
Several recent studies have looked at the possible contributors to depressive symptoms in sexual minority (SM) and/or gender minority (GM) youths. Andre Gonzales Real, MD and their colleagues studied 366 SM and GM youth, aged 15-21. They found:
“1 in 5 (18.2%) reported a different gender identity over time. Youths transitioning to a transgender or gender diverse identity reported higher levels of depressive symptoms at baseline: depressive symptoms disparities were explained by exposure to lesbian, gay, bisexual, and transgender violence, but frequency of gender identity variability was not associated with the level or changes in depressive symptoms.”
Gonzales Real and his group concluded that “…Changes in gender identity were not associated with depressive symptoms, suggesting that gender identity exploration is a normal part of adolescent development for some youth.”
Two other studies showed a relationship between depressive symptoms and bullying by their peers. Gower and their colleagues (2022) reviewed data from the Minnesota Student Survey, with 124,778 students in grades 8, 9 and 11 to determine the prevalence of sexual and gender identities. Their results and conclusions:
“Among 9th and 11th graders, 9.4% identified as lesbian, gay, bisexual, queer, or pansexual (1.7% pansexual, 0.4% queer). Among 8th, 9th, and 11th graders, 1.4% were transgender, genderqueer, or genderfluid, with almost half of those identifying as nonbinary; 2.1% were unsure of their gender identity. Rates of depressive symptoms were highest among pansexual students compared to other sexual orientations and among nonbinary and transmasculine youth who identified their sex as female. Rates of depression and bias-based bullying for youth who did not identify their sexual orientation as 1 of the response options were comparable to straight youth or those who did not understand the question.
Findings provide strong support for the inclusion of a broader set of sexual and
gender identity response options in epidemiological surveys and patient forms.
Pansexual and queer youth and transmasculine and nonbinary youth whose sex is female carry a particularly high burden of bias and discrimination, and clinicians should screen for additional services and supports these youth may need to thrive.”
Watson and their colleagues (2024) looked at data from a US national survey of sexual and gender diverse youth, aged 13-18 years with data collected in 2022. The sample size was 12,822 individuals. Their findings:
“Transgender boys were among those at the highest prevalence for compromised mental health and peer based in-person victimization. Although the primary distinguishing factor was transgender identity for depression and anxiety; there were no racial/ethnic distinctions, corroborating some previous scholarship. Asian cisgender and transgender [females] shared the lowest burden of peer-based in-person victimization in school.”
They concluded: “Our findings suggest a need for scholars, health professionals, and other stakeholders to better understand the mechanisms that drive negative health experiences and in-person victimization experiences at the intersections of sexual, gender, racial, and ethnic identities.”
Section 4: Treatment methods for Childhood and Adolescent Gender Dysphoria
A 2025 systematic review for treatment interventions for dysphoria completed by Dopp and their colleagues for Transgender and Gender-Expansive youth identifies seven different areas of potential treatment interventions. [Author’s note: The Human Rights Campaign’s Glossary of Terms (2023) defines a gender-expansive individual as: “A person with a wider, more flexible range of gender identity and/or expression than typically associated with the binary gender system. Often used as an umbrella term when referring to young people still exploring the possibilities of their gender expression and/or gender identity.”]
In their review, seven types of potential interventions were identified, potential outcomes were reviewed and the certainty of evidence for each intervention was assessed:
- Psychosocial interventions (e.g., social transition, professional psychological
support; k = 22 studies) were associated with decreases in suicidality and
depression (very low certainty). - Puberty-suppressing hormones (e.g., gonadotropin-releasing hormone analogues; k = 49 studies) were associated with decreases in pubertal changes, and hormone replacement therapy (e.g., testosterone, estrogen; k = 56 studies) was associated with increases in pubertal changes associated with the youth’s gender identity (both with low certainty). Both interventions were associated with reductions in youth-reported gender dysphoria in some studies; that outcome was measured infrequently, and evidence was rated very low certainty.
- Gender-affirming surgeries (k = 18 studies) were associated with reductions in gender dysphoria for mastectomy (low certainty) and other surgery types (very low certainty).
- Across these first four intervention categories, findings indicated low regret, low dissatisfaction levels, and low side effects and complications (all with very low certainty). For example, bone health metrics decreased relative to age-based reference values during puberty suppression; this outcome showed improvement after starting hormone replacement therapy (both very low certainty).
- Some studies found mental health improvements following hormones and surgeries, but others found no effects (very low certainty for all instances of the outcome, because of inconsistent study findings).
- Reproductive health interventions (k = 9 studies) were found to result in successful fertility preservation of viable oocytes, embryos, or semen (very low certainty).
- We did not identify relevant evidence for outcomes in youth for two intervention categories that are part of the standards of care: voice therapy and support for detransition.
- Treatment of co-occurring mental health or developmental disorders (k = 7 case reports) was not associated with improved mental health for interventions targeting eating disorders or depression and anxiety; for interventions targeting autism spectrum disorder, there was some evidence for improved autism symptoms but not gender dysphoria (all very low certainty).
- Gender identity and expression change efforts (sometimes referred to as conversion therapy or reparative therapy; k = 4 studies) were associated with increases in suicidality (low certainty) and increases or no change in mental health symptoms (very low certainty).”
Doop and their colleagues concluded:
“Despite the low certainty of the available evidence, practitioners and policymakers can use evidence-informed approaches that account for uncertainty in their decisions about health care for TGE youth, such as routinely updating the standards of care or developing relevant legislation. Researchers can use our findings to inform efforts to strengthen the evidence base by producing higher-certainty evidence with greater practice and policy relevance.”
Another important intervention is the use of the “chosen name” of the transgender and gender non-confirming youth across settings in their daily life. Russell and their colleagues (2018) collected data from “a community cohort sample of 129 transgender and gender nonconforming youth from three U.S. cities.” Their results and conclusion:
“After adjusting for personal characteristics and social support, chosen name use in more contexts was associated with lower depression, suicidal ideation, and suicidal behavior Depression, suicidal ideation, and suicidal behavior were lowest when chosen names could be used in all four contexts.
For transgender youth who choose a name different than the one given at birth, use of their chosen name in multiple contexts affirms their gender identity and reduces mental health risks known to be high in this group.”
Another systematic review by Heathcote and their colleagues (2023) looked at the psychosocial support interventions for children and adolescents with gender dysphoria or incongruence. Ten studies were reviewed, with five studies completed in the US and five international studies. Their findings include:
- “There is limited evidence on the outcomes of psychosocial interventions for children and adolescents experiencing gender dysphoria/incongruence.
- The evidence base for outcomes of psychosocial interventions for children and adolescents experiencing gender dysphoria/incongruence is of low quality.
- Most analyses of mental health, psychological and/or psychosocial outcomes showed either benefit or no change, with none indicating negative or adverse effects.
Heathcote and their colleagues recommend: “Identification of the core approach and outcomes for psychosocial interventions would ensure they are addressing key clinical goals, attending to the needs of children/adolescents and families as well as supporting future aggregation of evidence. More robust methodology and reporting is required.”
Medico and their group (2020) interviewed 10 transgender youth and their caregivers/ parents in Switzerland and found that “At least three developmental pathways seem to emerge:
- The affirmed children who affirm themselves very early,
- The silent children are the most common in our sample. These youth relate having had a feeling of not being cisgender since a long time but only revealing their gender identity around the onset of puberty. As a child they recalled a sense of not belonging, a felt, embodied sense of something being wrong. But this feeling was difficult to label or express for some youth, so they tried to repress and hide this feeling from others and from themselves during childhood. From a developmental perspective we can conclude that they experienced internal conflict regarding gender for many years.
- The neutral children who become aware of their gender difference at puberty following a childhood in which gender was not problematic.
In all cases puberty is a crossroads, lived painfully with significant manifestations of both social and body dysphoria. A better understanding of the process of gender development in trans children and youth will help improve our interventions to better serve young people and their families, and help them overcome the different levels of oppressions they face.
Sequeira and their colleagues (2025) surveyed 230 transgender and non-binary young adults who were between 18 and 20 years old when they presented for gender-affirming care. The results of their study include:
- Nearly all (94.3%) indicated they desired Gender Affirming Medical Care (GAMC) before age 18. Half (55.7%) of the respondents reported being out about their gender identity to a parent before age 18.
- Outness, discussing desire for GAMC, and asking for consent to receive GAMC from a parent were significantly more common among participants who identified as men compared to those who identified as women and among those assigned female at birth compared to those assigned male at birth. No such differences emerged when comparing nonbinary individuals to those who identified as men or women.
- Lack of parental willingness to consent for GAMC was cited as the primary contributor of not having received care in adolescence.
Kearns and their colleagues (2021) identified five potential barriers to receiving gender-affirming care:
- Disclosure of gender identity. Three studies flagged reluctance to disclose gender identity as a major systematic barrier to accessing gender care. For most young people, parental/guardian consent is a prerequisite to accessing care, and thus “coming out” is an imperative step.
- The pursuit of care: After coming out and progressing to the steps of finding a healthcare provider, youth face major structural barriers. This is evidenced in the literature as finding a suitable health care provider, geographical burdens and onerous waiting lists.
- The cost of care: Cost and insurance coverage are repeatedly identified as major systematic barriers to care. This is evidenced in the literature by young people who worry about how much it will cost and if their insurance will cover the cost. Some young people felt guilt and worry that their parents were burdened.
- Patient-provider relationships: Throughout the studies included in this review, variance exists on how youth access gender-affirming care. In some instances, young people present to a specialized gender clinic and all gender-affirming assessments are carried out in this service by a specialized multidisciplinary team (MDT). Others find a general physician who will provide gender-affirming care without MDT support. Five of the studies included in our synthesis enrolled patients who all accessed their gender affirming healthcare from different sources…Reports of healthcare providers (HCPs) being ill-equipped on gender related care were common throughout the studies.
Arnoldussen and their co-researchers (2023) looked at the demographics of the children and youth seeking gender-affirming care from a clinic in Amsterdam with a sample size of 506 birth-assigned males and 981 birth-assigned females referred between 2000 and 2018.
They found that:
“The distribution of the age of clinic referred transgender adolescents was not evenly distributed, but was distributed in a younger group presenting around the age of 11/12 years (median age 11.95 years) and an older group presenting around the age of 16/17 years (median age 16.25 years). Relatively more adolescents belonged to the older presenting group…
A larger part of the younger presenters lived with both biological parents, whereas the older presenters more often came from divorced families or other living circumstances. Of notice, younger adolescents more frequently were diagnosed with gender dysphoria and started with Gender-Affirming Medical Treatment (GAMT). Further, younger presenters showed higher levels of gender nonconformity in childhood. Finally, older presenters were more dissatisfied with most aspects of their bodies.”
Arnoldussen and their colleagues conclude:
“Our study showed that age distribution of adolescents who present at the Amsterdam gender service shows two peaks with a younger median age of 11.95 years and an older median age of 16.25 years. The differences exist between the younger and older presenters in terms of demographic, diagnostic, and treatment characteristics, gender nonconformity in childhood, and body image, suggesting that there may be different developmental pathways in adolescents that lead to seeking gender-affirming medical care. The fact that gender incongruent adolescents present at different ages with different characteristics calls for more research to understand the differences within the population and an individualized approach in the care and treatment of transgender
adolescents.”
Current guidelines from the World Professional Association for Transgender Health (WPATH) recommend a “comprehensive biopsychosocial assessment” before initiating pubertal suppression (Coleman et al, 2022). Turban and his associates (2024), describe the elements of the psychosocial assessment needed before initiating pubertal suppression:
- Introduce that the goal is not to determine whether patient “is really transgender.”
- Explain that the goal is to provide adolescent and family with all information
needed to make an informed decision about pubertal suppression. - Highlight that a clinician should work to identify all necessary domains of gender- related support (medical, social, legal educational).
- Collect a history and timeline of gender identity development. Under current
guidelines, one must establish a diagnosis of gender dysphoria and/or
gender incongruence prior to initiating pubertal suppression, depending on
the diagnosis in use in the clinician’s country of practice. - Obtain a history of past steps toward social transition (name, pronouns,
dress, etc). - Explore past and expected future reactions of family, peers, and community
members related to patient’s gender identity and expression to assess for
mental health risks and/or protective factors. - Elicit any issues at school related to gender (bullying, bathroom access
locker room access, sports participation). - Discuss a framework for conceptualizing gender identity (relationship to
gender roles and expectations, relationship to physical sex characteristics,
and transcendent “hard-to-put-into-words” feelings of gender), while being
flexible to developmental stage and the ways in which the adolescent and
their family conceptualize gender identity (eg, binary, non-binary, gender
fluid, etc). - Discuss concepts of sexual/romantic orientation, gender identity, and
gender expression. - Discuss unvalidated theories of TGD identities being related to trauma or
internalized misogyny, emphasizing that there are no data to establish
these etiologies but wanting patients to be exposed to these ideas in a safe
and supportive environment, given the likelihood of encountering them on
social or legacy media. - Collect a past medical history and family medical history to assess for
conditions that could be relevant to starting pubertal suppression (eg,
history of low bone density). - Discuss the reversible nature of pubertal blockers (endogenous puberty will
continue, if stopped) and encourage patient and family to be in close contact
with team about any evolving desires related to pubertal suppression. - Discuss that there will be a need in the future to either stop pubertal
suppression or initiate gender-affirming hormones. - Discuss fertility implications of pubertal suppression.
- Explain the impact of pubertal suppression on bone health, importance of
monitoring, and ways to mitigate risk (eg, increasing physical activity). - Discuss implications of blockers on possible future gender-affirming
surgeries. - Discuss experience of being delayed in puberty relative to peers.
- Emphasize the many diverse pathways that people experience (being TGD
with or without pursuing pubertal suppression, being cisgender with
diverse gender expression, being TGD with diverse gender expression, etc).
What do the systematic reviews and meta-analyses tell us about the current research on the use of puberty blockers for gender dysphoria in adolescents? Jo Taylor and their co-researchers (2023) found that: - There is a lack of high-quality research assessing the outcomes of hormones for masculinization or feminization in adolescents experiencing gender dysphoria/incongruence.
- There is limited or inconsistent evidence regarding gender dysphoria, body satisfaction, psychosocial and cognitive outcomes, fertility, height/growth, bone health and cardiometabolic effects.
- There is moderate-quality evidence from mainly pre–post studies that hormone treatment may in the short-term improve psychological health.
They conclude that: “There is a lack of high-quality evidence to support the initiation of hormones for masculinization or feminization in adolescents experiencing gender dysphoria/incongruence. Agreement on core outcomes and high-quality research are needed.”
A 2025 study by Miroshnychenko and their colleagues came to similar results and conclusions:
“We included 10 studies. Comparative observational studies (n=3), comparing puberty blockers versus no puberty blockers, provided very low certainty of evidence on the outcomes of global function and depression. Before–after studies (n=7) provided very low certainty of evidence addressing gender dysphoria, global function, depression, and there remains considerable uncertainty regarding the effects of puberty blockers in individuals experiencing GD. Methodologically rigorous prospective studies are needed
to understand the effects of this intervention.”
There have been several studies looking at the effectiveness of Gender-Affirming Hormone Treatment in improving mental health for transgender adolescents. Tordoff and their co-researchers (2022) found:
“In this prospective cohort of 104 Transgender and Non-binary (TNB) youths aged 13 to 20 years, receipt of gender-affirming care, including puberty blockers and gender-affirming hormones, was associated with 60% lower odds of moderate or severe depression and 73% lower odds of suicidality over a 12-month follow-up.”
They concluded: “This study found that access to gender-affirming care was associated with mitigation of mental health disparities among TNB youths over 1 year; given this population’s high rates of adverse mental health outcomes, these data suggest that access to pharmacological interventions may be associated with improved mental health among TNB youths over a short period.”
Olson-Kennedy and their group (2025) looked at emotional health outcomes for transgender youth after 24 months of gender-affirming hormone therapy. The objectives of their study were: - Investigate and verify the factor structure of the National Institutes of Health Toolbox Emotional Battery (NIHTB-EB) among trans and non-binary (TNB) youth
- Examine changes in emotional health over 24 months of GAH treatment
- Examine the extent to which changes in emotional health were associated
with improved appearance congruence (AC).
Olson-Kennedy’s study participants were:
“…From Trans Youth Care – United States (TYCUS) study, an observational, prospective, longitudinal study of adolescents initiating gender-affirming hormone (GAH) treatment enrolled between 2016 and 2019. Data was obtained at baseline, 6, 12, 18 and 24 months following initiation of GAH treatment….Eligible participants were those with gender dysphoria, aged 12-20 years, naïve to GAH, and initiating GAH for the purpose of phenotypic gender transition…315 youth were predominantly White (58.7%) and transmasculine (65%).”
They report the following implications and contribution of their research:
“Among adolescents with gender dysphoria, emotional health improves over 24 months of gender-affirming hormone treatment and is related to improvement in transgender appearance congruence. This manuscript expands on existing data examining the positive effect of medical treatment on mental health among youth experiencing gender dysphoria.”
A 2021 study by Green and their associates focused on the effects of gender-affirming hormone therapy on depression and thoughts of suicide. It was a very large survey of 34,759 lesbian, gay, bisexual, transgender, queer and questioning youth between the ages of 13 and 24, including 11,914 transgender or binary youth. They were recruited through “targeted ads on Facebook, Instagram, and Snapchat.”
They found that:
- Half of transgender and nonbinary youth said they were not using gender-affirming hormone treatment (GAHT) but would like to, 36% were not interested in receiving GAHT, and 14% were receiving GAHT.
- Parent support for their child’s gender identity had a strong relationship with receipt of GAHT, with nearly 80% of those who received GAHT reporting they had at least one parent who supported their gender identity.
- Use of GAHT was associated with lower odds of recent depression and seriously considering suicide compared to those who wanted GAHT but did not receive it.
- For youth under age 18, GAHT was associated with lower odds of recent depression and of a past-year suicide attempt.
Green and their associates conclude:
“Transgender and nonbinary youth have high risk of depression and suicide.
Gender-affirming healthcare is associated with lower risk using adult samples. This large-scale study examines GAHT among transgender and nonbinary youth. Findings demonstrate that GAHT is significantly related to lower rates of depression and suicidality among transgender and nonbinary youth.”
Chen and their colleagues (2023) looked at the psychosocial functioning of transgender adolescent after 2 years of gender-affirming hormone (GAH) treatment. 315 transgender and non-binary individuals between the ages of 12 and 10 years of age participated in the study. 60.3% were transmasculine (designated female at birth). 58.7% were non-Latinx white. They found:
“During the study period, appearance congruence, positive affect, and life satisfaction increased, and depression and anxiety symptoms decreased. Increases in appearance congruence were associated with concurrent increases in positive affect and life satisfaction and decreases in depression and anxiety symptoms. The most common adverse event was suicidal ideation (in 11 participants [3.5%]); death by suicide occurred in two participants…our findings showed improvements in psychosocial functioning across 2 years of GAH treatment, which supports the use of GAH as effective treatment for transgender and nonbinary youth.”
A 2022 study by Turban and their associates found that improved mental health outcomes from the use of gender-affirming hormone (GAH) treatment extended into adulthood. Conducting a secondary analysis of data from the 2015 Transgender Survey and found:
“21,598 participants (77.9%) reported ever desiring GAH. Of these, 8,860 (41%) never accessed GAH. 119 (0.6%) accessed GAH in early adolescents, 362 (1.7%) accessed GAH in late adolescence and 12,257 (56.8%) accessed GAH as adults. Adjusting for potential confounders, accessing GAH during early adolescence, late adolescence or adulthood was associated with lower odds of past year suicidal ideation when compared to desiring but never accessing GAH. In post hoc analysis, GAH during adolescence (ages 14-17) was associated with lower odds of past-year suicidal ideation when compared to accessing GAH during adulthood.”
Though the outcome studies regarding gender-affirming care show positive results, more research in the treatment of gender dysphoria/incongruence in childhood and adolescence is needed.
[Author’s note: Since January 2025, there has been a sharp decrease in federal funding and support for continued research and access to needed gender-affirming treatment for transgender children and adolescents in the United States. A trusted colleague recently told me, “Gender diverse people have always and will always exist, and how disheartening to see someone use their power to dehumanize and delegitimize the very existence of some of our most special kids.” Access to the research on evidence-based practice is one way to counter this alarming change in US federal policy.]
References Cited in Chapter Six
Arnoldussen, M., de Rooy, F.B.B., de Vries, A.L.C., van der Miesen, A.I.R., Popma, A, & Steensma, T.D. (2023) Demographics and gender-related measures in younger and older adolescents presenting to a gender service. European Child & Adolescent Psychiatry (2023) 32:2537–2546. https://doi.org/10.1007/s00787-022-02082-8
Brierley, J., Larcher, V., Hadjipanayis, A.A. and Grossman Z (2024) European Academy of Paediatrics statement on the clinical management of children and adolescents with gender dysphoria. Front. Pediatr. 12:1298884. doi: 10.3389/fped.2024.1298884
Chen, D., et. al. (2023) Psychosocial Functioning in Transgender Youth after 2 years of hormones. NEJM 388:240-250. DOI: 10.1056/NEJMoa2206297. LINK: Psychosocial Functioning in Transgender Youth after 2 Years of Hormones (2023)
Coleman, E., Radix, A. E., Bouman, W. P., Brown, G. R., de Vries, A. L. C., Deutsch, M. B., Ettner, R., Fraser, L., Goodman, M., Green, J., Hancock, A. B., Johnson, T. W., Karasic, D. H., Knudson, G. A., Leibowitz, S. F., Meyer-Bahlburg, H. F. L., Monstrey, S. J., Motmans, J., Nahata, L., Nieder, T. O., … Arcelus, J. (2022). Standards of care for the health of transgender and gender diverse people, version 8. International journal of transgender health, 23(Suppl 1), S1–S259. doi:10.1080/26895269.2022.2100644
Diamond, L.M. (2020) Gender Fluidity and Non-binary Gender Identities Among Children and Adolescents. Child Development Perspectives, 0:0, pages 1-6. LINK: Gender Fluidity and Nonbinary Gender Identities Among Children and Adolescents (2020)
Dopp, A. R., Peipert, A., Buss, J., De Jesús-Romero, R., Palmer, K., & Lorenzo-Luaces, L. (2025). Interventions for Gender Dysphoria and Related Health Problems in Transgender and Gender-Expansive Youth: A Systematic Review of Benefits and Risks to Inform Practice, Policy, and Research. Rand health quarterly, 1. LINK: Interventions for Gender Dysphoria and Related Health Problems in Transgender and Gender-Expansive Youth: A Systematic Review of Benefits and Risks to Inform Practice, Policy, and Research (2025).
Genspect (2023). The Gender Framework, Draft 1. Theories of Gender 1.21 to 1.9. (prepublication).
Gonzales Real, A., Rodrigues Lobato, M.I. & Russell, S.T. (2024) Trajectories of Gender Identity and Depressive Symptoms in Youths. JAMA Network Open. 2024;7(5):e2411322. doi:10.1001/jamanetworkopen.2024.11322 Downloaded from jamanetwork.com on 07/29/2025. LIST: Trajectories of Gender Identity and Depressive Symptoms in Youths (2024)
Gower, A.L., Rider, G.N., Brown, C. & Eisenberg, M.E. (2022) Diverse Sexual andGender Identity, Bullying, and Depression Among Adolescents. Pediatrics; 149(4):e2021053000. doi/10.1542/peds.2021-053000. LINK: Diverse Sexual and Gender Identity, Bullying, and Depression Among Adolescents (2022)
Green, A.E., DeChants, J.P., Price, M.N., & Davis, C.M. (2022) Association of Gender-Affirming Hormone Therapy With Depression, Thoughts of Suicide, and Attempted Suicide Among Transgender and Nonbinary Youth. Journal of Adolescent Health 70:643-649. https://doi.org/10.1016/j.jadohealth.2021.10.036 LINK: Association of Gender-Affirming Hormone Therapy with Depression, Thoughts of Suicide, and Attempted Suicide Among Transgender and Nonbinary Youth (2022)
Gulgoz, S., Glazier, J.J., Enright, E.A., Alonso, D.J., Durwood, L.J., Fast, A.A., Lowe, R., Ji, C., Heer, J., Martin, C.L. & Olson, K.R., (2019) Similarity in Transgender and cisgender children’s gender development. PNAS, 116(49), www.pnas.org/cgi/doi/10.1073/pnas.1909367116
Heathcote, C., Taylor, J., Hall, R., Jarvis, S.W., Langston, T., Hewitt, C.E. & Fraser, L. (2024) Psychosocial support interventions for children and adolescents experiencing gender dysphoria or incongruence: a systematic review. Arch Dis Child;109:s19–s32. (https:// doi. org/10. 1136/ archdischild- 2023-326347).
Hull, S., Origlio, J., Noyola, N., Henin, A., & Liu R.T. (2025) Dimensions of experienced gender and prospective self-injurious thoughts and behaviors in preadolescent children: A national study, Journal of Affective Disorders, Volume 369, 2025, Pages 467-474, ISSN 0165-0327, https://doi.org/10.1016/j.jad.2024.10.033
Human Rights Campaign (2023) Glossary of Terms. Accessed on 09/03/2025 from https://www.hrc.org/resources/glossary-of-terms? utm_source=ads_ms_HRC_20240306-HRC-AW-GS-Natl-GlossaryRP_GlossaryKeywords_a001-dynamic-rst_b:gender%20expansive&gad_source=1&gad_campaignid=21083351170&gbraid=0AAAAAD6IzShDCZUBIFgbv9rIGenyh0MFb&gclid=Cj0KCQjwzt_FBhCEARIsAJGFWVnueaXNUvDgd_QChgs_WtHVcU8L2C96nQ88TKMQ0j9jvlbfMmmSQeMaAkZJEALw_wcB
Joel, D., Berman, Z., Tavor, I., Wexler, N., Gaber, O., Stein, Y., Assaf, Y. (2015). Sex beyond the genitalia: The human brain mosaic. Proceedings of the National Academy of Sciences of the United States of America, 112, 15468–15473. https://doi.org/10.1073/pnas.1509654112
Kearns, S., Kroll, T., O‘Shea, D. & Neff, K. (2021) Experiences of transgender and non-binary youth accessing gender-affirming care: A systematic review and meta-ethnography. PLoS ONE 16(9): e0257194. doi.org/10.1371/journal.pone.0257194. LINK: Experiences of transgender and non-binary youth accessing gender-affirming care: A systematic review and meta-ethnography (2021)
Kucuker, M.U., Martinez Agulleiro, L.M., Guo, F., Stein, Baroni, A., and Janssen, A. (2024) Clinical Abstract for the Poster “Clinical Characteristics of Transgender and Gender-Diverse Youth Presenting to a Psychiatric Emergency Department” Presented at the 2024 Annual Meeting of the American Academy of Child and Adolescent Psychiatry in Seattle, Washington. https://doi.org/10.1016/j.jaac.2024.08.224
Levine, S.B. (2024) What is the Purpose of the Initial Psychiatric Evaluation of Minors with Gender Dysphoria, Journal of Sex & Marital Therapy, 50:6, 773-786, DOI: 10.1080/0092623X.2024.2362774.
Medico, D., Pullen Sansfaçon, A., Zufferey, A., Galantino, G., Bosom, M. & Suerich-Gulick F. (2020) Pathways to gender affirmation in trans youth: A qualitative and participative study with youth and their parents. Clinical Child Psychology and Psychiatry;25(4):1002-1014. doi:10.1177/1359104520938427. LINK: Pathways to gender affirmation in trans youth: A qualitative and participative study with youth and their parents (2020)
Miroshnychenko, A., Roldan, Y., Ibrahim, S., Kulatunga-Moruzi, C., Montante, S., Couban, R., Guyatt, G. & Brignardello-Peterson, R. (2025) Puberty blockers for gender dysphoria in youth: A systematic review and meta-analysis. Arch Dis Child 110:429–436. (https:// doi. org/10. 1136/ archdischild- 2024-327909).
O’Shea, J., Jenkins, R., Nicholls, D., Downs, J. & Hudson, L.D. (2025) Prevalence, severity and risk factors for mental disorders among sexual and gender minority young people: a systematic review of systematic reviews and meta-analyses. European Child & Adolescent Psychiatry (2025) 34:959–982. https://doi.org/10.1007/s00787-024-02552-1
Olson-Kennedy, J., Wang, L., Wong, C.F., Chen, D., Ehrensaft, D., Hidalgo, M.A., Tishelman, A.C., Chan, Y.-M., Garofalo, R., Radix, A.E., & Rosenthal, S.M. (2025) Emotional Health of Transgender Youth 24 Months After Initiating Gender-Affirming Hormone Therapy. Journal of Adolescent Health 77: 41-50. https://doi.org/10.1016/j.jadohealth.2024.11.014
Rider, G. N., McMorris, B. J., Gower, A. L., Coleman, E., & Eisenberg, M. E. (2018). Health and care utilization of transgender and gender nonconforming youth: A population-based study. Pediatrics, 141, 1–8. https://doi.org/10.1542/peds.2017-1683
Russell, S. T., Pollitt, A. M., Li, G., & Grossman, A. H. (2018). Chosen Name Use Is Linked to Reduced Depressive Symptoms, Suicidal Ideation, and Suicidal Behavior Among Transgender Youth. The Journal of adolescent health : official publication of the Society for Adolescent Medicine, 63(4), 503–505. https://doi.org/10.1016/j.jadohealth.2018.02.003
Sequeira, G.M., Kahn, N.F., Kyweluk, Kidd, K.M., Asante, P.G., Karrington, B., Bocek, K., Lucas, R., Christakis, D., Pratt, W. & Richardson, L.P. (2025) Desire for Gender-Affirming Medical Care Before Age 18 in Transgender and Nonbinary Young Adults. LGBT Health 12(1): 30-36 Link: Desire for Gender-Affirming Medical Care Before Age 18 in Transgender and Nonbinary Young Adults (2025), by Gina M. Sequeira
Suarez NA, Trujillo L, McKinnon II, et al. Disparities in School Connectedness, Unstable Housing, Experiences of Violence, Mental Health, and Suicidal Thoughts and Behaviors Among Transgender and Cisgender High School Students — Youth Risk Behavior Survey, United States, 2023. MMWR Suppl 2024;73(Suppl-4):50–58. LINK: Disparities in School Connectedness, Unstable Housing, Experiences of Violence, Mental Health, and Suicidal Thoughts and Behaviors Among Transgender and Cisgender High School Students — Youth Risk Behavior Survey, United States, 2023 (2024) DOI: hgttp://dx.doi.org/10.15585/mmwr.su7304a6.LINK:
Taylor J, Hall R, Heathcote C, et al. (2024) Clinical Guidelines for children and adolescents experiencing gender dysphoria or incongruence: a systematic review of guideline quality (part 1) Arch Dis Child, 109: s65–s72. https://doi.org/10.1136/ archdischild- 2023-326499).
Tordoff, D.M., Wanta, J.W., Collin, C., Stepney, C., Inwards-Breland, D.J. & Ahrens, K. (2022) Mental Health Outcomes in Transgender and Nonbinary Youths Receiving Gender-Affirming Care. JAMA Network Open. 2022;5(2):e220978. doi:10.1001/jamanetworkopen.2022.0978. LINK: Mental Health Outcomes in Transgender and Nonbinary Youths Receiving Gender-Affirming Care (2022)
Turban J.L, King, D., Kobe J., Reisner S.L. & Keuroghlian, A.S. (2022) Access to gender-affirming hormones during adolescence and mental health outcomes among transgender adults. PLoS ONE 17(1): e0261039. https://doi.org/10.1371/journal.pone.0261039
Turban, J.L., Thornton, A.B. & Ehrensaft, D. (2025) Biopsychosocial Assessments for Pubertal Suppression to Treat Adolescent Gender Dysphoria. JAACAP 64(1):12-16. LINK: Biopsychosocial Assessments for Pubertal Suppression to Treat Adolescent Gender Dysphoria (2025)
Watson, R.J. et. al. (2024) Examining Mental Health and Bullying Concerns at the Intersection of Sexuality, Gender, Race and Ethnicity Among a Sample of Sexual and Gender Diverse Youth. LGBT Health 11(1): https://doi.org/10.1089/lgbt.2023.0072. LINK: Examining Mental Health and Bullying Concerns at the Intersection of Sexuality, Gender, Race, and Ethnicity Among a National Sample of Sexual and Gender Diverse Youth (2024)
zerotothree.org (2021) Embracing Diversity: Developing a Gender Identity. Accessed from the Internet 07/31/2025 at https://www.zerotothree.org/resource/embracing-diversity-developing-a-gender-identity
Notable References not cited in Chapter Six
Bindman, J., Ngo., A, Zamudio-Haas, S. & Sevelius, J. (2021) Health care experiences of patients with nonbinary gender identities, Transgender Health X:X, 1–7, DOI: 10.1089/trgh.2021.0029.
Bloom, T., et. al. Measurement tools for gender identity, gender expression, and gender dysphoria in transgender and gender-diverse children and adolescents: a systematic review. The Lancet Child & Adolescent Health, Volume 5, Issue 8, 582 – 588. LINK: Measurement tools for gender identity, gender expression, and gender dysphoria in transgender and gender-diverse children and adolescents: a systematic review (2021)
Kahn, N.F., Asante, P.G., Coker, T.R., Kidd, K.M., Christakis, D.A., Richardson, L.P., & Sequeira, G.M. (2024). Demographic Differences in Gender Dysphoria Diagnosis and Access to Gender-Affirming Care Among Adolescents LGBT Health 11(5) 348-358. LINK: Demographic Differences in Gender Dysphoria Diagnosis and Access to Gender-Affirming Care Among Adolescents (2024)
Martin, C.L. & Ruble, D.N., (2010) Patterns of Gender Development. Annual Review of Psychology, 61: 353-381. https://doi.org/10.1146/annurev.psych.093008.100511
Miller-Perusse, M., Horvath, K.J., Kahle, E. & Stephenson, R. (2024) Gender Minority Stress, Resilience, and Psychological Distress: The Role of Resilience Among Transgender and Gender Diverse Youth. Transgender Health, 9(4) 307-3. DOI: 10.1089/trgh.2022.0117 [doi]. LINK: Gender Minority Stress, Resilience, and Psychological Distress: The Role of Resilience Among Transgender and Gender Diverse Youth (2024)
National Academies of Sciences, Engineering, and Medicine; Health and Medicine Division; Board on Health Care Services; Committee on Sex and Gender Identification and Implications for Disability Evaluation; Malcarney MB, Amaro HdlA, editors. Sex and Gender Identification and Implications for Disability Evaluation. Washington (DC): National Academies Press (US); 2024 Nov 18. Available from: https://www.ncbi.nlm.nih.gov/books/NBK610239/ doi: 10.17226/27775
Olson-Kennedy, J., Cohen-Kettenis, P., Kreukels-Baudewijntje, P.C., Meyer-Bahlburg, H., Garofalo, R., Meyer, W., & Rosenthal, S.M. (2016) Research priorities for gender nonconforming/transgender youth gender identity development and biopsychosocial outcomes. Current Opinion in Endocrinology & Diabetes and Obesity 23(2):172-179. DOI: 10.1097/MED.0000000000000236. LINK: Research priorities for gender nonconforming/transgender youth gender identity development and biopsychosocial outcomes (2016)
Parchem, B., Berona, J., Coyne, C.A., Moskowitz, J.T., Chan, Y-M., Ehrensaft, D., Garofalo, R., Hidalgo, M.E., Olson-Kennedy, J., Stephen M Rood, S. M., Reisner, S. L., Surace, F. I., Puckett, J. A., Maroney, M. R., & Pantalone, D. W. (2016). Expecting rejection: Understanding the minority stress experiences of transgender and gender-nonconforming individuals. Transgender health, 1(1), 151-164. DOI: 10.1089/trgh.2016.0012.
Rosenthal, A.C. et. al. (2025) Minority stress, mental health, and substance use in transgender youth: the moderating role of positive affect, Journal of Pediatric Psychology, Volume 50, Issue 5, May 2025, Pages 412–419, https://doi.org/10.1093/jpepsy/jsaf018
Suto, D., Turban, J. Belfort, E. (2024). Social Media and Development of Sexual and Gender Identity in Adolescents. Pediatric clinics of North America. 72. 279-289. 10.1016/j.pcl.2024.08.004.
Tankersley, A.P., Grafsky, E.L., Dike, J. et al. Risk and Resilience Factors for Mental Health among Transgender and Gender Nonconforming (TGNC) Youth: A Systematic Review. Clin Child Fam Psychol Rev 24, 183–206 (2021). https://doi.org/10.1007/s10567-021-00344-6. LINK: Risk and Resilience Factors for Mental Health among Transgender and Gender Nonconforming (TGNC) Youth: A Systematic Review (2021)
Turban, J.L., Brady, C. & Olson-Kennedy, J. (2022) Understanding and Supporting Patients with Dynamic Desires for Gender-Affirming Medical Interventions. JAMA Network Open. 2022;5(7):e2224722. doi:10.1001/jamanetworkopen.2022.24722. Downloaded from jamanetwork.com on 07/31/2025.
Turban, J., Dolotina, B., Freitag, T., King, D. & Keuroghlian, A. (2023). Age of Realization and Disclosure of Gender Identity Among Transgender Adults. Journal of Adolescent Health. 10.1016/j.jadohealth.2023.01.023.
Turban, J., Anderson, C. & Spetz, J. (2024). Gender Identity and Ethnoracial Disparities in Conversion Effort Exposure. American journal of public health. 114. 455-457. 10.2105/AJPH.2024.307630.
Wickham, M.I., van Nunspeet, F. & Ellemers, N. (2023) Gender Identification Beyond the Binary and Its Consequences for Social Well-being. Archives of Sexual Behavior 52: 1073-1093. https://doi.org/10.1007/s10508-022-02453-x
Additional References
*** The Myth of “Reliable Research” in Pediatric Gender Medicine: A critical evaluation of the Dutch Studies—and research that has followed (2023), by E. Abbruzzese, et al., published in the Journal of Sex & Marital Therapy
(Notable) *** Longitudinal impact of gender-affirming endocrine intervention on the mental health and well-being of transgender youths: preliminary results (2020), by Christal Achille, et al., published in the International Journal of Pediatric Endocrinology
*** Supporting and understanding non-binary & gender diverse youth: a physician’s view (2024), by Jamie Agapoff, published in Child and Adolescent Psychiatry and Mental Health
*** Negotiating Care: The Biographical Narratives of Young Adults Who Questioned Their Gender When Younger (2025), by Karl Atkin & Christine Jackson-Taylor, published in Sociology of Health & Illness
(Notable) *** Sexually and Gender Diverse Adolescents: Critical Perspectives on Risk and Resilience (2025), Eds. Laura Baams and Tessa M. L. Kaufman
*** Sexual Orientation and Gender Identity/Expression in Adolescent Research: Two Decades in Review (2023), by Laura Baams, et al., published in The Journal of Sex Research
*** A European Network for the Investigation of Gender Incongruence in adolescents (2024), by Lidewij S Boogers, et al., published in the Journal of Sexual Medicine
*** Disparities in School Connectedness, Unstable Housing, Experiences of Violence, Mental Health, and Suicidal Thoughts and Behaviors Among Transgender and Cisgender High School Students — Youth Risk Behavior Survey, United States, 2023 (2024)
*** Onset Age and Internalizing Problems in Adolescents with Gender Dysphoria: Is There an Association? (2025), by Saskia Fahrenkrug, et al., published in Archives of Sexual Behavior
*** Supporting Gender Identity in Early Childhood: Understanding the Lived Experiences of Parenting a Gender Variant Child Under Age 6 Years (2024), by Deborah L. Hahn, unpublished PhD dissertation, Walden University
(Notable) *** Evolving national guidelines for the treatment of children and adolescents with gender dysphoria: International perspectives (2025), by Kasia Kozlowska, et al., published in Human Systems: Therapy, Culture and Attachments
(Information Reference) *** National Health Service (NHS) England: Referral pathway for Children and Young People’s Gender Services Guidance for NHS Community and Hospital Paediatric Services (2025)
*** A nuanced look into youth journeys of gender transition and detransition (2023), by Annie Pullen Sansfaçon, et al.,published in Infant & Child Development
*** Masculinising and feminising hormone interventions for adolescents experiencing gender dysphoria or incongruence: a systematic review (2024), by Jo Taylor, et al., Archives of Disease in Childhood
(Notable) *** Perceived Gender Transition Progress, Gender Congruence, and Mental Health Symptoms Among Transgender Adolescents (2023), by Brian C. Thoma, et al., published in Journal of Adolescent Health
(Notable) *** A Systematic Review and Qualitative Research Synthesis of the Lived Experiences and Coping of Transgender and Gender Diverse Youth 18 Years or Younger (2024), by Krystiina Tyni, et al., published in the International Journal of Transgender Health
(Notable) *** How Transgender Adolescents Experience Expressing Their Gender Identity Around New People: An Interpretative Phenomenological Analysis (2021), by Hannah Wilson, et al., published in Journal of Adolescent Research
(Notable) *** Mental Health of Transgender and Gender Diverse Youth (2023), by Natalie M. Wittlin, et al., published in Annual Review of Clinical Psychology
**************************
>> (Chapter 7) What research has emphasized social and emotional support for individuals who identify as transgender/nonbinary and who are exploring questions regarding gender identity?
By Laura Henton, DNP, APRN, FNP-C
Overview:
For many individuals (adults and youths) who are experiencing serious emotional distress with respect to their gender identity and sexuality, a major positive difference is when individuals have solid and reliable support systems from friends and family. Below is a review of a vast range of studies in this area.
The 4-item Multidimensional Scale of Perceived Support and the 21-item Beck Depression Inventory were administered to 66 transgender youth aged 12-24 on the west coast (USA) who desired to start cross-sex hormone treatment (Simons et al., 2013). Parental support was found to be associated with higher life satisfaction, and protective against depressive symptoms and perceived burden of being transgender.
Seventy-five adolescent patients (aged 11-18) at a gender-affirming multidisciplinary clinic were surveyed regarding anxiety and depressive symptoms, suicidal ideations, and social support from friends and family. More than half of these participants (52%) were receiving hormonal interventions. Hormonal interventions were correlated with fewer anxiety symptoms. Fewer depressive symptoms were linked to family support, while friend support was associated with fewer anxiety symptomology and less suicidality (Olsavsky et al., 2023).
Selkie and colleagues (2020) interviewed 25 transgender adolescents (aged 15-18) from a pediatric gender clinic in the Midwest (USA) to determine how these patients use social media to access transgender-related support. Although the participants mentioned negative experiences (such as harassment), they did indicate that social media platforms provide emotional and informational support for transgender youth.
The concepts of self-compassion and perceived family support were the focus of researchers Samrock and colleagues (2021). These researchers interviewed 148 individuals (ages 18-64) who identified as transgender or non-binary and experienced gender dysphoria, and administered the 12-item Self-Compassion Scale-Short Form and the 20-item Center for Epidemiological Studies Depression Scale. Family support was measured by the 4-item Multidimensional Scale of Social Support. Negative associations were seen between depressive symptoms, family support, and self-compassion. This suggests that higher scores in self-compassion and perceived family support correlate to lower scores in depressive symptomology. These researchers found that “younger participants (aged 18-24) with lower family support reported the highest levels depressive symptoms” (Samrock et al., 2021, para. 1).
Pletta et al. (2024) followed a subset (n=495) of adult transgender and gender diverse individuals in New England (USA) for 12 months; these individuals (n=830) were part of a larger study. The study group was largely white (70%) transmen (40%) with bachelor’s degrees (53%) and private insurance (67%). The researchers were interested in the connection between social support and suicide attempts in this population. Social support was measured by the 12-item Multidimensional Scale of Perceived Social Support; psychological distress was measured with the 6-item Kessler Psychological Distress Scale; levels of community connectedness was measured with the Gender Minority Stress and Resilience Measure; and suicidality was measured with the US Army’s Study to Assess Risk and Resilience in Service Members Instrument. At the 12-month mark, a total of 26 participants reported having a suicide attempt. These researchers found that the following traits predicted a future suicide attempt: transfeminine gender identity, having a prior suicide attempt, and having moderate (versus high) perceived social support. The authors stress the importance of screening for future suicide risk, and interventions addressing facilitation of support from family and friends.
Structured peer navigation was the topic studied by Fowler et al. (2025), in a group of 15 participants undergoing feminizing gender-affirming hormone therapy at an Australian clinic. Participants acknowledged that informal peer support is already occurring, and that peer support offers support that healthcare providers cannot.
Lewis and colleagues (2023) used focus groups in their qualitative analysis to look at stigma, identity, and support. The focus groups were comprised of transgender people, relational partners, and service providers, in southwest England. The 26 people interviewed spoke more about their supportive social relationships rather than stigma and rejection.
Researchers Fuller and Riggs (2018) recruited 345 transgender participants for their online questionnaire, which asked about family support. Inclusionary criteria included being at least 18 years old and living in the United States. Resiliency, psychological distress, and perceived social support were scored. The average participant scored moderate to high levels of psychological distress; somewhat emotionally close to family members; and moderate to high levels of gender-related discrimination. The authors found that “emotional closeness to family does indeed mitigate the effects of general discrimination on psychological distress” (Fuller & Riggs, 2018).
Parents of transgender and gender-diverse adolescents (ages 11-17) were recruited by researchers (Belmont et al., 2024) to ascertain whether parental support predicted mental health outcomes in their transgender children. The 63 parents were predominantly white (92%), women (89%), straight (60%), college graduates (71%) who lived with their partner (62%) in Australia. The adolescents’ depressive symptoms were measured by their parents. Parental support for affirmation was found to be a strong predictor of lower depressive symptoms in the transgender children.
An online survey was completed by 695 transgender persons, who ranged in age from 16 to 73. Most of the participants were white (76%) transgender men (30%), with a mean age of 25. They were queried about their friends/family support (using the Multidimensional Scale of Perceived Social Support), community connection (using the Gender Minority Stress and Resilience Scale), depression (using the Patient-Reported Outcomes Measurement Information System, or PROMIS, Depression scale), anxiety (with the PROMIS-Anxiety scale), and resilience (with the Brief Resilience Scale). More than half of the participants reported moderate to severe levels of depressive and anxiety symptoms. More family support was correlated to lower depression/anxiety and more resilience. Support from friends was correlated with lower depression and anxiety symptomology, but not with increased resilience. Community connection did not show a significant influence on anxiety or resilience (Puckett et al., 2019).
Interest in specifically sibling support for transgender youth prompted Klepper et al. (2024) to critically review nine studies which addressed the lived experience with a transgender sibling. These researchers found that the support of siblings was associated with lessened depression and suicidal ideation.
Researchers Day and Brömdal (2024) performed a systematic literature review of 15 peer-reviewed studies, with an emphasis on the mental health of transgender schoolchildren, and the effect of the school environment. These researchers found a high rate of self-harm, suicidal ideations, and suicide in the school-aged transgender population. A limitation of this review is that only three of the 15 studies discussed schools with faith or religious affiliation. Religious institutions are long thought to be unwelcoming to transgender and nonbinary parishioners (Cline & Hampton, 2024); it follows that transgender youth are especially vulnerable in faith-based schools (Taylor & Cuthbert, 2019). Mohr and colleagues (2024) found that one-third of the transgender youth surveyed found acceptance in the religious setting, while the other two-thirds were neutral or had negative experiences. Transgender persons interviewed by Timbers et al. (2023) found acceptance and importance of community as reasons for staying affiliated with a faith-based organization. Day and Brömdal (2024) stress the importance of “fostering supportive environments for transgender and gender diverse youth” (p.12).
A systematic review was conducted by researchers Di Luigi and colleagues (2025). They reviewed 61 studies, looking at social gender affirmation (SGA), with an intent of developing “a new conceptualization of SGA by exploring how [transgender and gender-diverse] people, their social networks, and professionals … interpret and assign value to SGA” (Di Luigi et al., 2025, pp. 2-3). They noted that one aspect of non-affirmation, misgendering, was associated with increased anxiety and poorer mental health. Through their review of 61 studies, they recognized three core dimensions of social gender affirmation: interpersonal affirmation, societal recognition, and collaborative support.
References Used
Belmont, N., Cronin, T. J., & Pepping, C. A. (2024). Affirmation-support, parental conflict, and mental health outcomes of transgender and gender diverse youth. International Journal of Transgender Health, 25(1), 50-62.
https://doi.org/10.1080/26895269.2023.2252418
Cline, C. & Hampton, A. G. (2024). Defining welcome: Lesbian, gay, bisexual, and genderqueer Christian voices. Social Work & Christianity, 51(2), 181-216.
https://doi.org/10.34043/sdvw4p75
Day, M. & Brömdal, A. (2024). Mental health outcomes of transgender and gender diverse students in schools: A systematic literature review. International Journal of Transgender Health, 1-21.
https://doi.org/10.1080/26895269.2024.2359934
Di Luigi, G., Zoppolat, G., Steiglitz, S, & Doyle, D. M. (2025). Systematic review and development of a comprehensive conceptualization of social gender affirmation for trans and gender diverse people. SSM Mental Health, 7, 100453.
https://doi.org/10.1016/j.ssmmh.2025.100453
Fowler, J. A., Crilly, T., Reyment, M., Franks, N., Warzywoda, S., Bisshop, F., Wood, P., & Dean, J. A. (2025). Feasibility of a peer-navigation model of care to support transgender individuals undergoing feminizing gender-affirming hormone therapy: A qualitative study. International Journal of Transgender Health, 1-13.
https://doi.org/10.1080/15532739.2025.2464235
Fuller, K. A. & Riggs, D. W. (2018). Family support and discrimination and their relationship to psychological distress and resilience amongst transgender people. International Journal of Transgenderism, 19(4), 379-388.
https://doi.org/10.1080/15532739.2018.1500966
Klepper, M., Bosse, J., Flores, D. D., & Sanders, R. (2024). Sibling support for transgender and gender-diverse youth: A scoping review. Journal of Adolescent Health, 75(4), 543-552.
https://doi.org/10.1016/j.jadohealth.2024.05.014
Lewis, T. O. G., Barreto, M., & Doyle, D. M. (2023). Stigma, identity and support in social relationships of transgender people throughout transition: A qualitative analysis of multiple perspectives. Journal of Social Issues, 79(1), 108-128. https://doi.org/10.1111/josi.12521
Mohr, O., Chiaramonte, D. & Olezeski, C. L. (2024). Religious and spiritual experiences of transgender and gender nonconforming youth. Clinical Practice in Pediatric Psychology, 12(4), 480-488. https://doi.org/10.1037/cpp0000530
Olsavsky, A. L., Granis, C., Bricker, J., Chelvakumar, G., Indyk, J. A., Leibowitz, S. F., Mattson, W. I., Nelson, E. E., Stanek, C. J., & Nahata, L. (2023). Associations among gender-affirming hormonal interventions, social support, and transgender adolescents’ mental health. Journal of Adolescent Health, 72(6), 860-868. https://doi.org/10.1016/j.jadohealth.2023.01.031
Pletta, D. R., Austin, S. B., Chen, J. T., Radix, A. E., Keuroghlian, A. S., Hughto, J. M. W., & Reisner, S. L. (2024). Lower levels of social support are associated with risk for future suicide attempts in a clinical sample of transgender and gender diverse adults. Social Psychiatry and Psychiatric Epidemiology, 59(8), 1401-1412.
https://doi.org/ 10.1007/s00127-023-02606-w
Puckett, J. A., Matsuno, E., Dyar, C., Mustanski, B., & Newcomb, M. E. (2019). Mental health and resilience in transgender individuals: What type of support makes a difference? Journal of Family Psychology, 33(8), 954-964.
http://dx.doi.org/10.1037/fam0000561
Samrock, S., Kline, K. & Randall, A. K. (2021). Buffering against depressive symptoms: Associations between self-compassion, perceived family support and age for transgender and nonbinary individuals. International Journal of Environmental Research and Public Health, 18(15), 7938.
https://doi.org/10.3390/ijerph18157938
Selkie, E., Adkins, V., Masters, E., Bajpai, A., & Shumer, D. (2020). Transgender adolescents’ uses of social media for social support. Journal of Adolescent Health, 66(3), 275-280. https://doi.org/10.1016/j.jadohealth.2019.08.011
Simons, L., Schrager, S. M., Clark, L. F., Belzer, M., & Olson, J. (2013). Parental support and mental health among transgender adolescents. The Journal of Adolescent Health, 53(6), 791-793. https://doi.org/10.1016/j.jadohealth.2013.07.019
Taylor, Y. & Cuthbert, K. (2019). Queer religious youth in faith and community schools. Educational Review, 71(3), 382-396. https://doi.org/10.1080/00131911.2017.142327
Timbers, V. L., Gandy, M. E., Paciak, R., & Hopwood, R. A. (2023). Faithful foundations: Positive experiences of transgender and gender expansive individuals in faith communities. Mental Health, Religion & Culture, 26(5), 470-486. https://doi.org/10.1080/13674676.2023.2245351
Key Literature References
*** Feasibility of a peer-navigation model of care to support transgender individuals undergoing feminizing gender-affirming hormone therapy: A qualitative study (2025), by James Fowler, et al, published in International Journal of Transgender Health
(Notable) *** Systematic review and development of a comprehensive conceptualization of social gender affirmation for trans and gender diverse people (2025), by Guendalina Di Luigi, et al., published in SSM-Mental Health
*** Lower levels of social support are associated with risk for future suicide attempts in a clinical sample of transgender and gender diverse adults (2024), by David R. Pletta, et al., published in Social Psychiatry and Psychiatric Epidemiology
*** Sibling Support for Transgender and Gender-Diverse Youth: A Scoping Review (2024), by Meredith Klepper, et al., published in Journal of Adolescent Health
(Notable) *** Mental health outcomes of transgender and gender diverse students in schools: a systematic literature review (2024), by Mahaila Day, et al., published in the International Journal of Transgender Health
(Notable) *** Religious and Spiritual Experiences of Transgender
and Gender Nonconforming Youth (2024), by October Mohr, et al., published in Clinical Practice in Pediatric Psychology
*** Defining Welcome: Lesbian, Gay, Bisexual, and Genderqueer Christian Voices (2024), by Craig Cline, published in Social Work & Christianity
(Notable) *** Affirmation-support, parental conflict, and mental health outcomes of transgender and gender diverse youth (2024), by Natasha Belmont, et al., published in International Journal of Transgender Health
*** Associations Among Gender-Affirming Hormonal Interventions, Social Support, and Transgender Adolescents’ Mental Health (2023), by Anna L. Olsavsky, et al., published in Journal of Adolescent Health
(Notable) *** Faithful foundations: positive experiences of transgender and
gender expansive individuals in faith communities (2023), by Veronica L. Timbers, et al., published in Mental Health, Religion & Culture
(Notable) *** Stigma, identity and support in social relationships of transgender people throughout transition: A qualitative analysis of multiple perspectives (2022), by Tom O.G. Lewis, et al., published in The Journal of Social Issues
(Notable) *** Buffering against Depressive Symptoms: Associations between Self-Compassion, Perceived Family Support and Age for Transgender and Nonbinary Individuals (2021), by Steven Samrock, et al., published in International Journal of Environmental Research & Public Health
*** Transgender Adolescents’ Uses of Social Media for Social Support (2020), by Ellen Selkie, et al., published in Journal of Adolescent Health
*** Queer religious youth in faith and community schools (2019), by Yvette Taylor & Karen Cuthbert, published in Educational Review
(Notable) *** Mental Health and Resilience in Transgender Individuals: What Type of Support Makes a Difference? (2019), by Jae. A. Puckett, et. al, published in the Journal of Family Psychology
*** Family support and discrimination and their relationship to psychological distress and resilience amongst transgender people (2018), by Kimberly Fuller, published in the International Journal of Transgenderism
*** Parental Support and Mental Health Among Transgender Adolescents (2013), by Lisa Simons, et al., published in Journal of Adolescent Health
>> (Chapter 8) What are the most common areas of research that emphasize mental health assessment and issues for people who are transgender, nonbinary, or experiencing concerns with gender identity?
Overview by Scott Kerlin & Ian Cameron
Extensive research on mental health issues has been conducted with gender diverse populations over the years, and this collection highlights the leading dimensions of mental health vulnerabilities and trends. I recommend a deep exploration of the major areas of emphasis in the articles below.
>> Assessment of Mental Health in Gender-diverse Individuals
(Under development by Kerlin)
>> Mental Health Disparities in Gender Diverse Populations
Azagba, de Silva, & Ebling (2025) recognize “Gender minorities face unique health challenges. These challenges manifest in numerous physical, mental, and behavioral health disparities, with gender minorities experiencing a disproportionately high prevalence of adverse health outcomes. Compared to the general population or cisgender individuals, gender minorities have higher rates of psychiatric morbidities, including mood disorders, anxiety, depression, self-harm, and suicide.”
Further, the authors note, “Our study provides recent, population-based data showing mental health disparities among transgender individuals, which aligns with studies reporting high rates of depression and anxiety in this population. The higher incidence of poor mental health days among transgender individuals may support the minority stress model. This model suggests that marginalized groups face unique stressors, such as internalized stigma and discrimination, which can lead to adverse mental health outcomes. Prior studies have linked minority stressors to adverse mental health outcomes, including depression and suicidal ideation, among transgender individuals. The chronic stress associated with minority status may lead to heightened anxiety, which, over time, can contribute to the development of more severe mental health conditions. Additionally, the lack of social support and the experience of social rejection can exacerbate feelings of isolation and depression.”
Liu, et al. (2024) published results of a large Behavioral Risk Factor Surveillance System (BRFFS) study conducted under the auspices of the U.S. National Institutes of Health (NIH) that had the goal of assessing changes in mental health status of transgender and gender-diverse (TGD) individuals in the U.S. between 2014 and 2022. The report noted that among the nearly 2 million adults who participated in the study, “Prevalence of frequent mental distress increased from 18.8% in 2014 to 38.9% in 2022 among TGD adults and from 11.2% to 15.5% among cisgender adults. Prevalence of depression more than doubled from 19.7% to 51.3% among TGD adults, whereas smaller increases occurred among cisgender adults. Worsening of mental health outcomes was significantly more pronounced among TGD than cisgender adults.”
Hajek, et al., 2023 sought to determine prevalence and determinants of depressive and anxiety symptoms among transgender people, recognizing “For transgender people, health inequities are multifactorial and include increased risks for systematic social and economic marginalization, stigma, and discrimination. Transgender people are at substantially increased risk for various negative mental health outcomes compared to cisgender people. These poor mental health outcomes include depression and anxiety and are likely due to social rejection, stigma, discrimination, and violence.” Further, the observe that “transgender people face difficulties in receiving the diagnosis and obtaining care due to, for example, barriers to mental health care or/and experiencing stigma and discrimination by healthcare professionals or/and lack of support by their families. For example, transgender people often find in healthcare that providers lack skills in the area and are confronted with discrimination. Consequently, providers are often seen as unsupportive to transgender people’s healthcare needs.”
Pinna, et al. produced a substantial overview of published studies measuring mental health issues among transgender individuals for the International Review of Psychiatry in 2022 (see Cameron-Fleming in this report below).
Barr, et al., 2021 report “findings that document meaningful relationships between anti-transgender bias, non-affirmation, internalized transphobia, and posttraumatic stress. They provide initial support for conceptualizing anti-transgender bias and non-affirmation experiences as potentially traumatic themselves and/or as trauma response triggers and highlight a potential role of internalized transphobia in PTSD symptoms.” Their study documents “high rates of diagnosis of PTSD and trauma exposure based on DSM-5 symptom criteria.”
>> Contributing Factors for Adverse Mental Health in Transgender Populations
Significant research has recognized a strong positive association between adverse life experiences among transgender, nonbinary (TNB) and gender-diverse individuals and negative mental health effects. One valuable study in particular is by Tebbe & Budge (2022), who have developed an integrated theoretical framework of the predictive factors associated with TNB mental health disparities. They recognize that stigma-based stressors are associated directly and indirectly with mental health disparities in depression, anxiety, post-traumatic stress disorder (PTSD), self-harm, disordered eating, substance use in TNB individuals. They also observe that “rates of self-harm and suicidality in TNB populations create a public health crisis.”
Of particular note is recent research on adverse childhood experiences among sexual and gender minoritized adults. Schnarrs, et al. (2025), point out that “adverse childhood experiences (ACEs) are potentially traumatic events that occur before adulthood and include witnessing or experiencing various forms of abuse or neglect and other household challenges, such as substance abuse in the home or domestic violence. Research has consistently found that sexual and gender minoritized (SGM) people are at increased risk for ACEs exposure compared with heterosexual individuals.” They conclude that their findings “support the notion that early life adversity may lead to perceptions of a lack of social safety resulting from alterations in neurodevelopment. These alterations lead to greater awareness of discrimination in adulthood, and this contributes to worse mental health for SGM adults. Early prevention is needed to buffer against the effects of ACEs.”
Fasel, et al., 2025 observe that “Transgender individuals as gender minorities have a high prevalence of depressive symptoms (52%) and anxiety symptoms (38%), which is significantly higher compared with non-gender minorities Among LGBT people, transgender individuals were at greatest risk with a lifetime prevalence for non-suicidal self-jury. Across 42 studies, 55% of transgender individuals ideated about and 29% attempted suicide in their lifespan.”
Their research emphasized attention to specific Early Maladaptive Schemas (EMSs) that develop during childhood as adaptive responses to one’s aversive environment, form a template that guides the interpretation of later experience and may elicit significant impairment. EMSs are theorized to be a result of unmet core emotional needs in childhood, primarily due to the interaction between adverse childhood experiences and emotional temperament are defined as “dysfunctional and pervasive patterns of memories, thoughts, and physical sensations regarding the self, relationships, and world that develop in childhood and adolescent years and elaborate throughout the life”, and are particularly observed in transgender and gender-diverse adults.
Mezza, et al., 2024 conducted a systematic review of quantitative studies of minority stress and mental health in European transgender and gender-diverse people, concluding “minority stress factors are significantly related to various mental health problems, including depression, anxiety, and suicidal tendencies among European TGD population, and that resilience factors might buffer these harmful effects, contributing to the person’s psychological well-being. Although the life conditions of TGD people living in Europe have been increasingly improving over the last few decades, the TGD population continues to face pervasive stigma, which dramatically impacts mental health by limiting the access to resources and generating cumulative, chronic stress.”
Kidd, et al., 2023 utilized minority stress theory (a public health framework that is widely used to explain gender-identity-related health disparities) to investigate a “consistent link between minority stress and poor mental health among transgender people.” They conclude that “results provide clear evidence of poorer mental health (serious psychological distress, suicidality, non-suicidal self-injury) among transgender adults, compared to cisgender adults.”
>> Self-Compassion and Mental Health in Gender Minority Populations
Researchers Emily C. Helminen, et al., 2022 point out, sexual and gender minority (SGM) populations report numerous mental health disparities relative to heterosexual and cisgender populations, due in part to the effects of minority stress. They conducted a meta-analysis of self-compassion literature focusing on SGM populations. In overview, they recognize that self-compassion encompasses three main components: (1) self-kindness, (2) common humanity, and (3) mindfulness. Self-kindness refers to “the ability to treat oneself with kindness during moments of suffering or failure. Common humanity refers to the understanding that one shares the experience of suffering with other humans. Mindfulness, in the context of self-compassion, is the ability to attend to one’s feelings of suffering without being
overwhelmed by them. Scholars have begun to conceptualize self-compassion as a coping resource that may buffer against the negative health effects of general stress.” In conclusion, the authors state that self-compassion represents a promising coping resource to promote positive mental health among SGM populations. This review proposes self-compassion as a coping resource to protect against the deleterious health effects of minority stress among SGM populations. Through a meta-analysis and synthesis of the literature, we found preliminary evidence for self-compassion as a coping resource among SGM populations. Specifically, self-compassion seems to have robust direct associations with minority stress and mental health, and there is cross-sectional evidence that self-compassion may act as a mediator within minority stress and psychological mediation frameworks, though more research is needed to clarify these effects.
Carvalho & Guiomar (2022) examined twenty-one studies in their meta-analysis, corresponding to a total of 6573 nonheterosexual and/or noncisgender participants. All meta-analytic models were significant: higher levels of self-compassion were associated with less depression, anxiety, psychological distress, suicidal ideation, internalized homophobia/transphobia, and stigma, and with more well-being, outness, and social support. Their summary:
Conclusion: This meta-analysis suggests that self-compassion is significantly associated with mental health indicators in SGM people, and this relationship is especially strong with internalized homophobia/transphobia in older SGM adults, and with suicidal ideation in younger SGM individuals. Results suggest that affirmative mental health care may benefit from promoting self-compassion.
In a recent PhD dissertation completed at the University of Alberta, Canada, author Britany N. Budzan (2023) summarized, “The purpose of this study was to explore the experiences of self-compassion in non-binary young adults. To this end, I utilized an interpretative phenomenological analysis approach, engaging in in-depth interviews with seven participants. Transcripts for each interview were coded and grouped into higher order themes. After analyzing individual cases, I conducted a cross-case analysis, from which emerged five super-ordinate themes: (a) intentional self-care; (b) developing a positive sense of self; (c) living with authenticity; (d) improved coping through perspective taking, and (e) self-compassion as an interpersonal process. The findings from this study suggest that self-compassion may be a positive strategy for promoting mental health and well-being in non-binary young adults. Implications for clinical practice are discussed, in addition to limitations and future research directions.”
Rosenthal, et al. (2023) examined the role of self-compassion in mediating against harmful effects of everyday discrimination in sexual and gender minorities (SGM)–particularly depression and suicidality. They concluded, “among gender minority individuals, there was a significant interaction between everyday discrimination and self-compassion for probable depression and having considered suicide. For all SGM individuals, perceived discrimination was associated with poor mental health. Among gender minority adults, self-compassion was protective and attenuated this relationship. It is crucial to address discrimination using a multilevel approach to ensure reduction of harm for SGM individuals across the United States.”
By Ian Cameron
From: Anxiety and Depression Across Gender and Sexual Minorities: Implications for Transgender, Gender Nonconforming, Pansexual, Demisexual, Asexual, Queer, and Questioning Individuals. Borgogna N. et al. [2019] Psychology of Sexual Orientation and Gender Diversity.
Empirical findings indicate that sexual and gender minorities report notably poorer outcomes on measures of mental health when compared with cisgender/heterosexual individuals. Although several studies have examined these issues, few have taken the time to examine differences between cisgender/ heterosexual and specific lesbian, gay, bisexual, transgender, and queer identities. This is especially important as an increasing number of new gender and sexual identities emerge, yet limitations in statistical power often preclude such analyses. Evidence of an interaction of gender and sexual identity impacting mental health such that those with minority statuses in both identity groups had significantly worse outcomes compared to those with only one minority identity. Individuals in the emerging sexual and gender minority categories (pansexual, demisexual, asexual, queer, questioning, and transgender/gender nonconforming) report significantly higher rates of depression and anxiety when compared with cisgender/heterosexual individuals, and even significantly more than those who identify as gay/lesbian.
These findings support the notion of a synergistic, interactive effect of gender identity and sexual orientation on mental health outcomes whereby participants who had minority status membership for both identities had the highest levels of anxiety and depression. This provides evidence of the additive effects of multiple sexual and gender minority statuses in a person’s demography on mental health.
Future studies should examine the relationship across gender identity, sexual orientation, and mental health outcomes using alternative and more comprehensive measures such as personality inventories and instruments designed to assess stress related to each identity. Comparisons of mental health outcomes and associated factors across these gender and sexual identities using longitudinal designs would also likely yield beneficial information for scientists and clinicians alike, especially studies that track the fluidity/stability of these identities through adolescence into adult hood.
From: Mental health in transgender individuals: a systematic review. Pinna F. et al. [2022] International Review of Psychiatry.
Several lines of evidence indicate the prevalence of mental health disorders in Transgender (TG) individuals is higher than that of cisgender individuals or the general population. In this systematic review, we aim to propose a summary of some of the most significant research investigating mental health disorders’ prevalence among this population. We performed a double-blind systematic review using the Preferred Reporting Items for Systematic Reviews and Meta-analyses reporting (PRISMA) on PUBMED/MEDLINE and SCOPUS, specifically using peer-reviewed articles examining the mental health status of transgender (TG) individuals. This review did not exclude any research based on publication date.
The last search was performed in February 2022. The employed search strategy led to the selection of 165 peer-reviewed articles. The majority of these papers presented a cross-sectional design with self-reported diagnoses and symptoms, signalling a significant prevalence of mental health disorders amongst TG Individuals.
Of the reviewed articles, 72 examined the prevalence of mood and anxiety disorders; 8 examined eating disorders; 43 examined the prevalence of suicidal or self-harm ideation or behaviours; 5 papers examined the prevalence of trauma and stress-related disorders; 10 examined the frequency of personality disorders; 44 examined substance use disorders; and 9 papers examined the prevalence of autism spectrum disorder. Finally, 22 studies reported on the prevalence of TG individuals diagnosed with co-morbid mental health disorders or unspecified mental disorders. Our findings coincide with existing research, which indicates TG individuals do experience a higher prevalence of mental health disorders than that of the general population or cisgender individuals. However, further research is needed to address the existing gaps in knowledge.
Many psychologists and other mental healthcare professionals still report limited experience and training in providing care to TG individuals, often resorting to generalising their competence from sexual minorities, versus gender minorities, such as lesbian, gay, or bisexual persons. Transgender and gender-diverse youth experience a high degree of discrimination, such as bullying and peer rejection. Consequently, approximately one out of four transgender or gender-diverse youth experience a high degree of anxiety and symptoms of major depressive disorder, with one out of two of these youth making attempts to complete suicide.
Given the preponderance of evidence to suggest the mental health of TG individuals suffers from societal discrimination, researchers must also consider how discrimination impacts available data. Specifically, as the available research is largely based on self-report, we must recognise that there is a phenomena of identity concealment within the TG community. Several lines of evidence point to a higher prevalence of mental health disorders among TG Individuals in comparison to the general population or cisgender individuals.
Even though increasing efforts in studying the prevalence of mental health disorders within the TG community resulted in significant advancements in this field, much remains to be done. More research is needed in addressing the existing gaps in knowledge and how to promote the well-being of this underserved population.
Key Literature References
(Notable) *** US State Policies and Mental Health Symptoms Among Sexual and Gender Minority Adults (2025), by Briana S. Last, et al., published in JAMA Network Open
*** Mental Health Disparities Among LGBTQ People in the US—Time to End the Stigma (2025), by Mandi L. Pratt-Chapman, published in JAMA Network Open
(Notable) *** Examining general, physical, and mental health disparities between transgender and cisgender adults in the U.S. (2025), by Sunday Azagba, et al., published in International Journal for Equity in Health
*** It is time for gender-affirming care: Trans+ experiences and perspectives on presurgical mental health assessment prior to transition-related surgery referral (2025), by Dupasquier, Jessica R., et al., published in Canadian Psychology
(Notable) *** Adverse Childhood Experiences, Perceived Discrimination, and Mental Health in Sexual and Gender Minoritized Adults: Comparing Stress Accumulation and Stress Sensitization Models (2025), by Phillip W. Schnarrs, et al., published in the journal LGBT Health
*** Internalized Transnegativity, Self-Warmth, Self-Coldness, and Eating Disorder Symptomatology Among Transgender and Nonbinary Adults (2025), by Sarah McArthur, et al., published in Journal of Clinical Psychology
*** Increased vulnerability to psychological distress and suicidal ideation among transgender women with self-reported disabilities in San Francisco, California (2025), by Abtin Shafie, et al., published in Preventative Medicine Reports
(Notable) *** Relationship between early maladaptive schemas (EMSs), adverse childhood experiences and mental health in adulthood among transgender individuals (2025), by Mirko Fasel, et al., published in the European Journal of Psychotraumatology
(Notable) *** Minority stress and mental health in European transgender and gender diverse people: A systematic review of quantitative studies (2024), by Fabrizio Mezza, et al., published in Clinical Psychology Review
*** Bans on Evidence-Based Care for Transgender and Gender Diverse People Present Risks for Clients and Dilemmas for Mental Health Providers (2024), by Debra A. Hope & Jae A. Puckett, published in Cognitive and Behavioral Research
*** Transgender and Gender Diverse Individuals in their Faith Communities: The Impact of Religious Abuse on Mental Health Outcomes by Meghan Elizabeth Wood, PhD Dissertation, Texas Woman’s University
(Notable) *** Health Status and Mental Health of Transgender and Gender-Diverse Adults (2024), by Michael Liu, et al., published in JAMA Internal Medicine
*** Temporal Trends in Mental Health in the United States by Gender Identity, 2014–2021 (2024), by Donn Feir, et al., published in The American Journal of Public Health
*** Everyday Discrimination and Mental Health among Sexual and Gender Minority Adults: The Moderating Role of Self-compassion (2023), by Samantha R. Rosenthal, et al., published in the journal Psychology of Sexual Orientation and Gender Diversity
(Notable) *** Prevalence and Determinants of Depressive and Anxiety Symptoms among Transgender People: Results of a Survey (2023), by André Hajek , et al., published in the journal Healthcare
*** Structural transphobia is associated with psychological distress and suicidality in a large national sample of transgender adults (2023), by Maggi A. Price, et al., published in Social Psychiatry and Psychiatric Epidemiology
(Notable) *** Prevalence of substance use and mental health problems among transgender and cisgender U.S. adults: Results from a national probability sample (2023), by Jeremy D. Kidd, et al., published in Psychiatry Research
(Notable) *** Self-compassion, minority stress, and mental health in sexual and gender minority populations: A meta-analysis and systematic review (2023), by Helminen, et al., published in Clinical Psychology: Science and Practice
*** Everyday discrimination and mental health among sexual and gender minority adults: The moderating role of self-compassion (2023), by S.R. Rosenthal, et al., published in the journal Psychology of Sexual Orientation and Gender Diversity
*** Mental Health in Transgender Individuals: A Systematic Review (2022), by Federica Pinna, et al., published in International Review of Psychiatry
(Notable) *** Factors that drive mental health disparities and promote well-being in transgender and nonbinary people (2022), by Elliot A. Tebbe & Stephanie L. Budge, published in Nature Reviews: Psychology
(Notable) *** Experiences of Self-Compassion in Young Adults with Non-Binary Gender Identities (2022), by Brittany N. Budzan, unpublished PhD dissertation, University of Alberta, Canada
*** Self-Compassion and Mental Health in Sexual and Gender Minority People: A Systematic Review and Meta-Analysis (2022), by Sergio A. Carvalho & Raquel Guiomar, published in the journal LGBT Health
(Notable) *** Understanding factors that affect wellbeing in trans people “later” in transition: a qualitative study (2022), by Z. Aldridge, et al., published in the journal Quality of Life Research
(Notable) *** Posttraumatic Stress in the Trans Community: The Roles of Anti-transgender Bias, non-Affirmation, and Internalized Transphobia (2021), by Sebastian M. Barr, et. al, published in the journal Psychology of Sexual Orientation and Gender Diversity
(Notable) *** Mental Health in Transgender Adults: The Role of Proximal Minority Stress, Community Connectedness, and Gender Nonconformity (2021), by Valerie Helsen, Paul Enzlin, & Luk Gijs, published in the Psychology of Sexual Orientation and Gender Diversity
(Notable) *** Mental Health Issues and Complex Experiences of Abuse Among Trans and Gender Diverse Young People: Findings from Trans Pathways (2020), by Penelope Strauss, et al., published in LGBT Health
(Notable) *** Mental Health and Quality of Life in non-binary transgender adults: A Case Control Study (2019), by Bethany A. Jones, Walter Pierre Bouman, Emma Haycraft, & Jon Arcelus, published in the International Journal of Transgenderism
*** Anxiety and Depression Across Gender and Sexual Minorities: Implications for Transgender, Gender Nonconforming, Pansexual, Demisexual, Asexual, Queer, and Questioning Individuals (2019), by Nicholas C. Borgogna, et. al, published in the Psychology of Sexual Orientation and Gender Diversity
(Notable) *** Generational Differences in Internalized Transnegativity and Psychological Distress Among Feminine Spectrum Transgender People (2018), by Kasey B Jackman, et al., published in LGBT Health
>> (Chapter 9) What are the principal areas of mental health treatment and outcomes for persons experiencing gender dysphoria?
By Scott Kerlin and Ian Cameron
Overview: This section will grow considerably when the June issue of this report is completed. One area that especially interests me, from my own personal experience, is a focus on evaluating the relative effectiveness and value of psychotherapy. One recommended article is by Katie Schofield (2025), “Let me be me: Investigating transgender clients’ experiences of their therapeutic relationship with their counsellor.”
(Note: Five sections of current focus by Kerlin & Cameron are currently under development)
I. Mental Health Benefits of Treatment and Outcomes for Gender Dysphoria
(Under development by Kerlin)
Much research has been published that seeks to measure the definitive positive outcomes of treatments and interventions designed to accomplish improvements in mental health among transgender and gender-diverse people.
Shelemy et al. (2024) state that there are four theorized contributors to distress
and mental health difficulties in TGD (transgender and gender-diverse) people: 1) gender dysphoria, 2) minority stressors, 3) reduced social support and 4) reduced access to healthcare services. Gender dysphoria describes the sense of feeling unhappy, uncomfortable and unaligned with one’s sex assigned at birth. This sensation is persistent for many TGD people and is often present from early childhood. Further, they observed that “A number of interventions exist that aim to directly reduce gender dysphoria experienced by individuals. These interventions introduce physical, psychological, social and behavioral changes to reduce the individual’s experienced discrepancy between their sex assigned at birth (or biological sex) and their gender identity. These include medical interventions that alter the biological and/or physical appearance of an individual, psychological/psychosocial interventions (e.g. therapeutic peer-led group spaces) and adaptive methods to address physical appearance and internal congruity (e.g. breast binding, genital tucking, body sculpting). The theory behind these interventions is that alleviating the gender dysphoria-related distress may improve an individual’s discomfort, self-identity, self-esteem and interaction with minority stressors which may in turn lead to mental health benefits.
The authors identified 29 major published studies that measured effectiveness of significant interventions for treating gender dysphoria, especially hormone and psychological treatments, and “tentatively” concluded that they were of particular benefit for reducing depression.
Mezzalira et al., (2025) assessed effectiveness of psychotherapy with transgender/nonbinary patients and reported highly varied patient experiences, based on diverse components of the patient/therapist working relationship.
(to be continued)
II. Mental Health Symptoms Most Frequently Treated in Transgender, Gender-diverse, and Nonbinary Individuals
(Under development by Kerlin)
III. Models of Mental Health Treatment and Care for Transgender and Gender-diverse Individuals
(Under development by Kerlin & Cameron)
(Notable) *** Mental Health Care for Transgender and Non-binary Adults: An Investigation of Affirmative Practice, Therapy Experiences and Outcomes, and Reasons for Treatment Termination (2025), by Christopher A. Pepping, et al., published in Sexuality Research and Social Policy
(Notable) *** A patient-centered model of mental health care for trauma and minority stress in transgender and gender diverse people: A bottom-up network analysis (2024), by Anna Salomaa, et al., published in the journal Psychology of Sexual Orientation and Gender Diversity
*** Care of Transgender Patients: A General Practice Quality Improvement Approach (2022), by Isabel Boyd, et al., published in the journal Healthcare
(Notable) *** One Size Does not Fit All: In Support of Psychotherapy for Gender Dysphoria (2021), by Roberto D’Angelo et. al, published in the Archives of Sexual Behavior
Review of Selected Study, by Ian Cameron
From: A thematic analysis of approaches to practice with people who are transgender and gender nonconforming. Leitch J. [2021] Department of Social Work, University of North Carolina, Greensboro, NC, USA. Wiley
People who are transgender and gender nonconforming (TGNC) have substantial disparities in mental health and thus rely on mental health practitioners like therapists to help address these disparities. However, little is known about therapist practices with TGNC people, and what research exists is often generalised from broader research on practice with people who are gay and lesbian. Because this research uses broad models to describe practitioner behaviour, it assumes all therapists approach practice with TGNC clients in the same way.
The current study explores therapists’ self- reported practices with TGNC people through a structured, qualitative, web- based survey of 95 practising social workers. From a thematic analysis of responses, five approaches to practice with TGNC people emerged: 1) A Low- Impact Approach, 2) A Fairness First Approach, 3) A Responsive Approach, 4) A Therapist Responsibility Approach and 5) A Pathological Approach. These approaches vary on three key dimensions: whose responsibility it is to broach client gender identity in treatment (therapist or client), the importance of gender identity (from low to high), and whether a TGNC identity is a disorder (yes, no or not addressed). The breadth of practice behaviours and undergirding assumptions participants described indicates that a single model may not fit practice behaviour with TGNC people.
A discussion of the relationship between each approach and existing practice models suggests that the Low- Impact Approach, Responsive Approach and Therapist Responsibility Approach may be effective with TGNC people and that the Pathological Approach likely represents poor practice.
People who identify as transgender and/or gender nonconforming (TGNC) are at risk of substantial mental health disparities and their related effects. They are six times more likely to have a mood or anxiety disorder than the general population and have lifetime prevalence rates of depression at around 60%. Close to half of all transgender people have attempted suicide, with attempt rates eight times higher than the general population. Rates of mental health disorders for the broader population of sexual and gender minority (SGM) people have been increasing since they were first measured. These disparities may be why TGNC people have such high use of counselling professionals such as psychologists and social workers, underscoring the need for competent and effective practices with this population.
Although it is important to relate practice approaches to clinical outcomes, the relative effectiveness of these approaches has not been studied. However, we can relate these approaches to existing practices with TGNC people and the related clinical outcomes.
Five approaches emerged from participants’ self- described behaviour: a Low- Impact Approach, a Responsive Approach, a Fairness First Approach, a Therapist Responsibility Approach and a Pathological Approach. These vary on dimensions of the importance of gender identity, the role of the client and therapist in discussing gender identity and whether a TGNC identity is a disorder. While effects of the use of these approaches have not been studied, relationships with existing practice models suggest that the Low- Impact Approach, Responsive Approach and Therapist Responsibility Approach might be effective with TGNC clients, whereas the Pathological Approach may hinder therapeutic progress.
This study suggests that there may be some relationship between including the classification of Gender Dysphoria in the DSM 5 and the belief that a TGNC identity is a disorder. It may be valuable to consider this as the field negotiates the ongoing inclusion of this category diagnosis.
IV. Experiences of Psychotherapy Among People who Identify as Transgender, Gender-diverse, and Non-binary
(Under development by Kerlin)
V. Factors Affecting Access to Mental Health Care for Transgender, Gender-diverse, and Non-binary Individuals
(Under development by Kerlin & Cameron)
Review of Selected Study, by Ian Cameron
From: A thematic analysis of approaches to practice with people who are transgender and gender nonconforming. Leitch J. [2021] Department of Social Work, University of North Carolina, Greensboro, NC, USA. Wiley
People who are transgender and gender nonconforming (TGNC) have substantial disparities in mental health and thus rely on mental health practitioners like therapists to help address these disparities. However, little is known about therapist practices with TGNC people, and what research exists is often generalised from broader research on practice with people who are gay and lesbian. Because this research uses broad models to describe practitioner behaviour, it assumes all therapists approach practice with TGNC clients in the same way.
The current study explores therapists’ self- reported practices with TGNC people through a structured, qualitative, web- based survey of 95 practising social workers. From a thematic analysis of responses, five approaches to practice with TGNC people emerged: 1) A Low- Impact Approach, 2) A Fairness First Approach, 3) A Responsive Approach, 4) A Therapist Responsibility Approach and 5) A Pathological Approach. These approaches vary on three key dimensions: whose responsibility it is to broach client gender identity in treatment (therapist or client), the importance of gender identity (from low to high), and whether a TGNC identity is a disorder (yes, no or not addressed). The breadth of practice behaviours and undergirding assumptions participants described indicates that a single model may not fit practice behaviour with TGNC people.
A discussion of the relationship between each approach and existing practice models suggests that the Low- Impact Approach, Responsive Approach and Therapist Responsibility Approach may be effective with TGNC people and that the Pathological Approach likely represents poor practice.
People who identify as transgender and/or gender nonconforming (TGNC) are at risk of substantial mental health disparities and their related effects. They are six times more likely to have a mood or anxiety disorder than the general population and have lifetime prevalence rates of depression at around 60%. Close to half of all transgender people have attempted suicide, with attempt rates eight times higher than the general population. Rates of mental health disorders for the broader population of sexual and gender minority (SGM) people have been increasing since they were first measured. These disparities may be why TGNC people have such high use of counselling professionals such as psychologists and social workers, underscoring the need for competent and effective practices with this population.
Although it is important to relate practice approaches to clinical outcomes, the relative effectiveness of these approaches has not been studied. However, we can relate these approaches to existing practices with TGNC people and the related clinical outcomes.
Five approaches emerged from participants’ self- described behaviour: a Low- Impact Approach, a Responsive Approach, a Fairness First Approach, a Therapist Responsibility Approach and a Pathological Approach. These vary on dimensions of the importance of gender identity, the role of the client and therapist in discussing gender identity and whether a TGNC identity is a disorder. While effects of the use of these approaches have not been studied, relationships with existing practice models suggest that the Low- Impact Approach, Responsive Approach and Therapist Responsibility Approach might be effective with TGNC clients, whereas the Pathological Approach may hinder therapeutic progress.
This study suggests that there may be some relationship between including the classification of Gender Dysphoria in the DSM 5 and the belief that a TGNC identity is a disorder. It may be valuable to consider this as the field negotiates the ongoing inclusion of this category diagnosis.
Key Literature References
*** Gender affirming hormone therapy for individuals with gender dysphoria aged <26 years: a systematic review and meta-analysis (2025), by Anna Miroshnychenko, et al., published in Archives of Disease in Childhood
(Notable) *** Let me be me: Investigating transgender clients’ experiences of their therapeutic relationship with their counsellor (2025), by Katie Schofield, et al., published in Counseling and Psychotherapy Research
(Notable) *** Mental Health Care for Transgender and Non-binary Adults: An Investigation of Affirmative Practice, Therapy Experiences and Outcomes, and Reasons for Treatment Termination (2025), by Christopher A. Pepping, et al., published in Sexuality Research and Social Policy
(Notable) *** Supporting autonomy in young people with gender dysphoria: Psychotherapy is not conversion therapy (2025), by Roberto D’Angelo, published in BMJ Journal of Medical Ethics
(Notable) *** Trans in treatment: a mixed-method systematic review on the psychotherapeutic experiences of transgender and gender diverse people (2025), by Selene Mezzalira, et al., published in Research in Psychotherapy: Psychopathology, Process and Outcome (RIPPPO)
(Notable) *** Systematic review of prospective adult mental health outcomes following affirmative interventions for gender dysphoria (2024), by Lucas Shelemy, et al., published in International Journal of Transgender Health
(Notable) *** Changes in depression symptom profile with gender-affirming hormone use in transgender persons (2024), by Margot W.L. Morssinkhof, et al., published in Journal of Affective Disorders
*** Required Mental Health Evaluation Before Initiating Gender-Affirming Hormones: Trans and Nonbinary Perspectives (2024), by Daphna Stroumsa, et al., published in Transgender Health
(Notable) *** A patient-centered model of mental health care for trauma and minority stress in transgender and gender diverse people: A bottom-up network analysis (2024), by Anna Salomaa, et al., published in the journal Psychology of Sexual Orientation and Gender Diversity
*** Factors Associated with Experiences of Gender-Affirming Health Care: A Systematic Review (2023), by Jamie D. Howell* and Rebecca Maguire, published in the journal Transgender Health
*** Care of Transgender Patients: A General Practice Quality Improvement Approach (2022), by Isabel Boyd, et al., published in the journal Healthcare
(Notable) *** The Experiences of Psychological Therapy Amongst People Who Identify as Transgender or Gender Non-conforming: A Systematic Review of Qualitative Research (2022), by Emily Compton, published in Journal of Feminist Family Therapy
(Notable) *** Differences in mental health symptom severity and care engagement among transgender and gender diverse individuals: Findings from a large community health center (2021), by Amelia M. Stanton, et al., published in the journal PLOSOne
(Notable) *** One Size Does not Fit All: In Support of Psychotherapy for Gender Dysphoria (2021), by Roberto D’Angelo et. al, published in the Archives of Sexual Behavior
*** A thematic analysis of approaches to practice with people who are transgender and gender nonconforming (2021), by Judith Leitch, published in Counselling and Psychotherapy Research
(Notable) *** Mental Health Treatment Utilization in Transgender Persons: What We Know and What We Don’t Know (2020), by Sven C. Mueller, published in The American Journal of Psychiatry
(Notable) *** Barriers to Mental Health Care for Trangender and Gender-Nonconforming Adults: A Systematic Literature Review (2019), by Annie Snow, et. al, published in the journal Health & Social Work
(Notable) *** Reduction in Mental Health Treatment Utilization Among Transgender Individuals After Gender-Affirming Surgeries: A Total Population Study (2019), by Richard Bränström, et al., published in The American Journal of Psychiatry
*** Association Between Gender Confirmation Treatments and Perceived Gender Congruence, Body Image Satisfaction, and Mental Health in a Cohort of Transgender Individuals (2018), by Ashli A. Owen-Smith, et al., published in The Journal of Sexual Medicine
(Notable) *** Transgender Clients: Identifying and Minimizing Barriers to Mental Health Treatment (2018), by Jillian C. Shipherd, et al., published in Journal of Gay & Lesbian Mental Health
>> (Chapter 10) What are the leading issues associated with gender-affirming healthcare?
Overview by Ian-Cameron Fleming and Scott Kerlin (References)
From: Patients’ Perceived Level of Clinician Knowledge of Transgender Health Care, Self-rated Health, and Psychological Distress Among Transgender Adults. Miller G H, et al, (2023) JAMA Network Open.
Transgender, gender nonbinary, and genderqueer people are at increased risk for negative health outcomes, and medical school education is currently lacking on inclusion of these topics. However, there is little evidence of an association of clinician knowledge with the health of transgender people. The findings of this cross-sectional study suggest that there is an association between perceived clinician knowledge about transgender people and self-rated health and psychological distress among transgender people. These results highlight the importance of integration and enhancement of transgender health in medical education curriculum as a necessary intervention to improve the health of transgender people.
Long-term stressors, including restrictive policy environments, structural and interpersonal experiences of transphobia, discrimination, stigmatization, and gender minority stress (“the social stressors specific to transgender and other gender minority people that result from gender-related discrimination, … nonaffirmation of gender identity, internalized transphobia, … community connectedness, and pride”), are important factors contributing to these adverse health outcomes. Medical education is an important step in addressing these adverse health outcomes and poor clinical experiences of transgender people.
This perceived lack of knowledge about transgender people and health care for transgender people among clinicians was negatively associated with SRH (Self Related Health) and SPD (Severe Psychological Distress) Although this association remained after controlling for a host of covariates, we stop short at suggesting the education of clinicians alone will improve the mental and overall health of transgender people. Importantly, other factors contribute to the adverse health outcomes of transgender patients. Restrictive state policy environments are associated with poor health and less access to care for transgender people. Experiences of discrimination, stigmatization, and gender minority stress outside the health care context are also associated with negative health outcomes.
Nevertheless, the integration of education surrounding transgender people and transgender health disparities is an important step to address ongoing health disparities transgender populations face. Patients benefit from clinicians trained to understand the health disparities experienced by transgender people and to use best communication practices for these patients. Kattari et alexplored the association of transgender individuals seeking inclusive clinicians with changes in mental health outcomes. Their results indicate that transgender individuals who saw a gender-inclusive clinician and had preexisting mood disorders showed almost a 50% decrease in suicidality, defined as having suicidal thoughts within the past year.30 Ultimately, incorporating more LGBTQAI health topics and considerations on social determinants of health into the medical curriculum provides positive outcomes for learners and future patients.
In this cross-sectional study of transgender, nonbinary, and genderqueer adults, we found that patients’ perceived levels of knowledge clinicians had about transgender people and providing transgender health care was associated with health outcomes of transgender people. Our results demonstrate that transgender people who had to teach their clinicians about transgender people and who reported their clinicians had lower levels of knowledge about transgender health care were at significantly higher odds of reporting fair or poor SRH and were at significantly higher odds of meeting the criteria for SPD. These findings provide empirical evidence to support the integration and enhancement of transgender health care and the impacts of gender identity in the medical education curriculum as a necessary intervention to improve the health of transgender, gender nonbinary, and genderqueer people.
From: Care of Transgender Patients: A General Practice Quality Improvement Approach. Boyd I, et al. (2022) The journal Healthcare.
Primary care must ensure high quality lifelong care is offered to trans and gender minority patients who are known to have poor health and adverse healthcare experiences. This quality improvement project aimed to interrogate and audit the data of trans and gender minority patients in one primary care population in England. A new data collection instrument was created examining pathways of care, assessments and interventions undertaken, monitoring, and complications. General practitioners identified a sample from the patient population and then performed an audit to examine against an established standard of care. No appropriate primary care audit standard was found. There was inconsistency between multiple UK gender identity clinics’ (GIC) individual recommended schedules of care and between specialty guidelines. Using an international, secondary care, evidence-informed guideline, it appeared that up to two-thirds of patients did not receive all recommended monitoring standards, largely due to inconsistencies between GIC and international guidance. It is imperative that an evidence-based primary care guideline is devised alongside measurable standards. Given the findings of long waits, high rates of medical complexity, and some undesired treatment outcomes (including a fifth of patients stopping hormones of whom more than half cited regret or detransition experiences), this small but population-based quality improvement approach should be replicated and expanded upon at scale.
Transgender (trans) people experience adverse health outcomes and increased mortality. Poor healthcare has been identified as one of many factors that lower quality of life for trans people. A 2016 Lancet series examined in detail the conditions in which transgender people live and experience healthcare and provided a framework on which to make improvements to social and legal conditions as well as clinical care considerations and service delivery models. Transgender people report that when they access healthcare regarding gender dysphoria, providers often lack relevant skills and appear unsupportive or hostile to their healthcare needs. They feel uncomfortable discussing their needs with new health care providers and have a fear of mistreatment.
International specialist guidelines exist for the treatment of gender dysphoria. These include the World Professional Association of Transgender Health (WPATH) guidelines and the Endocrine Society guidelines, both of which are widely cited. In 2019 NHS England (the NHS commissioning board) published Service Specifications for Gender Identity Services for adults. NHS England service specifications are written to define standards of care expected from specialist services. They are developed by specialized clinicians, commissioners, expert patients, and public health representatives. These guidelines recommend either self-referral or GP referral to Gender Identity Clinics (GICs), followed by a minimum of two assessments in the clinic where neither endocrinology nor psychology input is considered mandatory, and support should be “affirmative”. The clinics are then permitted to ask the patient’s GP to prescribe hormones and/or gonadotrophin-releasing hormone agonists (GNRHa) under a “Shared Care Agreement” where the clinic provides ongoing follow-up of the patient until they are discharged.
This first published UK quality improvement project of transgender healthcare in primary care generated useful, practice-level data. No UK-wide evidence-based treatment or monitoring guidelines for gender dysphoria in primary care were found. Existing international, national, and GIC guidelines were found to contain contradictions. This problem constrained the audit cycle but is an important finding in itself. The practice audit found that 62% of patients received at least one measure of substandard monitoring when set against the Endocrine Society guidance, largely due to conflicts with the patients’ individual GIC Schedule of Care. By contrast, the practice services for trans patients overall had been noted as “outstanding” in 2018 following an inspection by the independent UK health and social care monitor and regulator, the Care Quality Commission, maybe demonstrating the inadequacy of using the blunt tools of a conflicting international guideline, idiosyncratic UK GIC Schedules of Care or the CQC process.
As practice patients are being treated by multiple NHS and private clinics, provision of safe monitoring by GPs is likely to be more difficult when no national standard exists and GICs’ guidance conflict with one another. Thus, it is difficult for any primary health caregiver to know whether their care really is objectively “substandard” or not. How does a GP know which is the optimal guideline to follow? There is no mechanism for them to question whether guidance recommended by the Endocrine Society such as annual “sub and periareolar breast examinations” in transmen post-mastectomy, is evidence-based, and in patients’ interests, rather than unnecessary and invasive. A further example of conflicting guidance is demonstrated with pelvic ultrasound monitoring of transmen on testosterone. Guidance varies from no advice given, no monitoring advised, biannual ultrasound, or two-yearly ultrasound. Guidance around polycythaemia is also variable, the consequent complication of which could be a stroke or heart attack.
Aside from long waiting times, the routes to hormone therapy and surgery aligned with NHS service specifications. There were many self-referrals to GICs (bypassing traditional primary care triage or gatekeeping), few assessment appointments, and high levels of GP-initiated prescribing. Self-referral was only found in the private clinics, and private clinics provided fewer assessment appointments than the NHS clinics. No international, national, or GIC guideline that we reviewed provided information regarding detransition or regret, or services for these patients.
These findings complement secondary care-generated knowledge and suggest room for improvement. Gender minority/trans people will be better served by evidence-based primary care guidance, including monitoring and communication standards. Existing guidance is contradictory. Given the findings of long waits for GIC assessment, and some unwanted outcomes and complications (including detransition), this small but hypothesis-generating primary care-focused, population-based, quality improvement approach should be replicated and expanded upon at scale.
From: Hormone Therapy, Mental Health, and Quality of Life Among Transgender People: A Systematic Review. Baker K E, et. al, (2021) The Journal of the Endocrine Society
Many transgender people seek medical services to affirm their gender identity. According to the Standards of Care for Transsexual, Transgender, and Gender Non-Conforming People maintained by the World Professional Association for Transgender Health (WPATH), gender-affirming medical care is different for each individual and may include a variety of services and procedures, such as psychological support, hormone therapy, and surgeries. Hormone therapy, which typically involves oestrogens and anti-androgens for transgender women and other trans-feminine people and testosterone for transgender men and other trans-masculine people, is a common component of medical gender affirmation.
Because hormone treatment can have a powerful effect on physical appearance, it is often a priority for transgender people seeking medical gender affirmation. Gender-affirming hormone therapy can be managed for most patients by primary care providers, as it typically involves long-term maintenance on doses similar to those used for cisgender patients with conditions such as hypogonadism. Some clinicians require a minimum period of psychological counseling before hormone therapy can be initiated, while others provide hormone therapy on the basis of informed consent.
The need for gender-affirming care is often characterized using psychiatric diagnoses such as gender dysphoria, which replaced gender identity disorder. Several previous reviews have indicated that gender-affirming hormone therapy is associated with psychological benefits that include reductions in depression and anxiety and improvements in quality of life (QOL) among transgender people.
No study found that hormone therapy decreased QOL scores. We conclude that hormone therapy may improve QOL among transgender people. The strength of evidence for this conclusion is low due to concerns about bias in study designs, imprecision in measurement because of small sample sizes, and confounding by factors such as gender-affirming surgery status.
No study found that hormone therapy increased depression. We conclude that hormone therapy may decrease depression among transgender people. The strength of evidence for this conclusion is low due to concerns about study designs, small sample sizes, and confounding.
No study found that hormone therapy increased anxiety. We conclude that hormone therapy may decrease anxiety among transgender people. The strength of evidence for this conclusion is low due to concerns about study designs, small sample sizes, and confounding.
No conclusions on the basis of this single study about whether hormone therapy affects death by suicide among transgender people.
Uncontrolled confounding was a major limitation in this literature. Many studies simultaneously assessed different types of gender-affirming care and did not control for gender-affirming surgery status, making it difficult to isolate the effects of hormone therapy. Others failed to report complete information about surgery status.
Clinic-based recruitment also overlooks transgender people who cannot access these clinics for financial or other reasons and misses those whose need for gender affirmation does not fit into current medical models. This is a particular concern for nonbinary and other gender-diverse people, for whom a model of gender affirmation as a linear transition from one binary gender to another is inaccurate.
More research is needed to further explore the relationship between gender-affirming hormone therapy and QOL, death by suicide, and other psychological outcomes, especially among adolescents. Future studies should investigate these outcomes in larger groups of diverse participants recruited outside clinical settings. Studies assessing the relationship between gender-affirming hormone therapy and mental health outcomes in transgender populations should be prospective or use strong quasi-experimental designs; consistently report type, dose, and duration of hormone therapy; adjust for possible confounding by gender-affirming surgery status; control for other variables that may independently influence psychological outcomes; and report results separately by gender identity. Despite the limitations of the available evidence, however, our review indicates that gender-affirming hormone therapy is likely associated with improvements in QOL, depression, and anxiety. No studies showed that hormone therapy harms mental health or quality of life among transgender people. These benefits make hormone therapy an essential component of care that promotes the health and well-being of transgender people.
From: How gender theories are used in contemporary public health research. Hammarström A & Hensing G, (2018) International Journal for Equity in Health.
Public health research often focuses on gender differences within certain diagnoses, but so far research has failed to explain these differences in a satisfactory way. Theoretical development could be one prerequisite for moving beyond categorical thinking. The aim of this paper was to analyse how gender theories have been used in public health research in relation to various methodological approaches.
international research shows that substantial gender differences exist within certain major diagnoses, such as hypertension and depression. However, researchers have so far failed to explain these differences in a satisfactory way. This might in part be related to the fact that public health studies often favour empirical research while the researchers lack strong theoretical framework. Thus, much research is devoted to replicating previously known gender differences in health status rather than to explain their origin, which also might contribute to the preservation of gender stereotypes.I n order to find better explanations for gender differences in health status we need to use gender-related concepts, models or theories, yet there is still a lack of development of gender theories in public health research.
The lack of gender theoretical analyses in the final report of the influential Commission of Social Determinants in Health [7] (CSDH) has been highlighted as a major problem. The commission was set up by the WHO in 2005 in order to marshal evidence on what could be done to reach equity in health from a global perspective.
As gender researchers in public health, we recognise the difficulties of moving beyond the statistical quantification of differences between men and women, which is common in epidemiological research. Gender theoretical development is central in the process of moving beyond categorical thinking. In previous research, we have also clarified our use of gender related concepts in order to advance the development of gender theories [6, 12]. Since we are often asked how gender theories can be used in public health research, we believe an important next step towards a comprehensive theory of gender in public health would be to study how gender theories are actually used in contemporary public health research.
The following six special issues contained at least one paper and therefore fulfilled our inclusion criteria (33 papers in total):
I. Current Sociology 2009–7 papers
II. Social Science and Medicine (intersectionality) 2012–16 papers
III. Scandinavian Journal of Work Environment and Health 2005 – 1 paper
IV. International Review of Psychiatry 2011–1 paper
V. Ergonomics 2012-– 1 paper
VI. Social Science and Medicine (masculinities and suicidal behaviour) 2012–7 papers.
The six special issues differed in relation to both their focus and theoretical approach. The health outcomes were specific in three of them; mental health (IV), ergonomics (V) and suicide (VI), while unspecific in the others. The gender theoretical focus was specified in some of the special issues: as relational, intersectional and biosocial (II), to focusing on masculinities (VI). In Current Sociology (I), the theoretical point of departures was specified as the sociological understanding of gender and health (health as gendered, unpacking gender as social category, the health needs of various gender identities, medicalization and the sociology of the body). Gender differences (without references to gender theories) in occupational health as well as in ergonomics were in focus in two special issues (III, V), while special issue IV dealt with more general biological and epidemiological differences in mental health.
The categorical thinking in public health research about gender-related topics should be met with gender theoretical development. With this paper we hope to both inspire and demonstrate to researchers how to develop gender theories in public health research. We do this by providing a set of strategies for using gender theories in relation to various methodological approaches (both qualitative and quantitative, as well as mixed methods approaches) within the broad field of public health.
As a study initiating this approach, we consider our findings to also be useful in education. Public health practitioners have diverse backgrounds. In medical and health science professions, a binary understanding of women and men from a mainly biological point of view is usually predominant in education. However, most public health problems need to be addressed combining bio-psycho-social perspectives. Gender theories open up new perspectives for how to understand women and men in their various contexts, including gendered structures and norms. An important aspect in developing teaching material on gender and health is the inclusion of various gender theories. Our paper has the potential to be an important aid in such training, addressing both the approaches that are currently most used, as well as highlighting how new theoretical perspectives can be applied in research.
A problem within the field of public health research, is that theories are generally underdeveloped. However, there is an increasing theoretical interest in health promotion. Thus, theories are useful in explaining why certain interventions are successful while others are not. Our study identified no gender theoretical paper within the field of health promotion. Through gender theoretical development, the effects of public health interventions can be improved for both men and women with various backgrounds.
Nancy Krieger argues for the need of theories as a way of improving public health research, to avoid errors, spark new ideas, and enable us to be critical of studies. She argues “…by making conscious use of epidemiological theory and having informed debates over the different theoretical perspectives in play we stand a better chance of producing epidemiological knowledge truly useful for preventing disease, promoting health equity and improving people’s health.” And to that we would add: …to move beyond categorical thinking in relation to research on gender and health.
References:
Key Literature References (Kerlin)
*** Transgender adults’ narratives of gender identity and access to care: A timeline study (2025), by Abbey K. Mann & Nadia Manasfi, published in the journal Sexual and Gender Diversity in Social Services
(Notable) *** Providers’ Beliefs and Values: Understanding Their Approach to Gender-Affirming Care (2025), by Ahona Shirin, et al., published in Journal of Primary Care & Community Health
*** The medical institution and transgender health: The role of healthcare barriers and negative healthcare experiences (2025), by Lawrence Stacey, et al., published in Social Science & Medicine
*** The AFFIRM Framework for gender-affirming care: qualitative findings from the Transgender and Gender Diverse Health Equity Study (2025), by Meg Quint, et al., published in BMC Public Health
(Notable) *** Barriers to quality healthcare among transgender and gender nonconforming adults (2025), by Kedryn Berrian, et al., published in Health Services Research
*** Providers’ Beliefs and Values: Understanding Their Approach to Gender-Affirming Care (2025), by Ahona Shirin, et al., published in Journal of Primary Care & Community Health
(Notable) *** Reevaluating gender-affirming care: biological foundations, ethical dilemmas, and the complexities of gender dysphoria (2025), by Marc J. Defant, published in The Journal of Sex & Marital Therapy
*** Gender-Affirming Hormone Therapy Improves Levels of Depression in Transgender Individuals Within the First Year of Treatment (2024), by Cassandra M Godar, et al., published in Journal of The Endocrine Society
(Notable) *** Factors Associated with Experiences of Gender-Affirming Health Care: A Systematic Review (2023), by Jamie D. Howell* and Rebecca Maguire, published in the journal Transgender Health
*** Peer-based interventions to support transgender and gender diverse people’s health and healthcare access: A scoping review (2023), by Ashley Lacombe-Duncan, et al., published in the International Journal of Transgender Health
(Notable) *** Gender Dysphoria and Its Non-Surgical and Surgical Treatments (2023), by Danyon Anderson, et. al, published in the journal Health Psychology Research
*** Patients’ Perceived Level of Clinician Knowledge of Transgender Health Care, Self-rated Health, and Psychological Distress Among Transgender Adults (2023), by Gabe H. Miller, et al., published in JAMA Network Open
*** Care of Transgender Patients: A General Practice Quality Improvement Approach (2022), by Isabel Boyd, et al., published in the journal Healthcare
*** Gender-Affirming Hormone Therapy for the Trans, Gender Diverse, and Nonbinary Community: Coordinating World Professional Association for Transgender Health and Informed Consent Models of Care (2022), by Pravik Solanki, et. al, published in the journal Transgender Health
(Notable) *** Suggestions for Improving Healthcare for Transgender and Gender Diverse People in the United States (2022), by Jae Puckett, et al., published in the International Journal of Transgender Health
(Notable) *** Standards of Care for the Health of Transgender and Gender Diverse People, Version 8 (2022), by Eli Coleman, et al., published in the International Journal of Transgender Health
*** Surgical Satisfaction and Quality of Life Outcomes Reported by Transgender Men and Women at least One Year Post Gender-Affirming Surgery: A Systematic Literature Review (2022), by Christienne Javier, et. al, published in the International Journal of Transgender Health
(Notable) *** The process of transitioning for the transgender individual and the nursing imperative: A narrative review (2021), by Shelley Evans, et al., published in the Journal of Advanced Nursing
(Notable) *** Health and health care access in the US transgender population health (TransPop) survey (2021), by Jamie L. Feldman, et al., published in the journal Andrology
*** Hormone Therapy, Mental Health, and Quality of Life Among Transgender People: A Systematic Review (2021), by Kellan E. Baker, et. al, published in the Journal of the Endocrine Society
*** Care of Transgender Persons (2019), by Joshua D. Safer, M.D., and Vin Tangpricha, M.D., Ph.D., published in the New England Journal of Medicine
>> (Chapter 11) What additional healthcare topics have been emphasized in research with transgender and nonbinary individuals?
Overview by Ian Cameron
From: Fertility in transgender and gender diverse people: systematic review of the effects of gender-affirming hormones on reproductive organs and fertility. De Roo C et al. 2025. Human Reproduction Update.
Transgender and gender diverse (TGD) people seek gender-affirming care at any age to manage gender identities or expressions that differ from their birth gender. Gender-affirming hormone treatment (GAHT) and gender-affirming surgery may alter reproductive function and/or anatomy, limiting future reproductive options to varying degrees, if individuals desire to either give birth or become a biological parent.
TGD people increasingly pursue help for their reproductive questions, including fertility, fertility preservation, active desire for children, and future options. Their specific needs certainly require more insight into the effects of GAHT on gonads, gametes, and fertility. This systematic review aims to provide an overview of the current knowledge on the impact of GAHT on gonads, gametes, fertility, fertility preservation techniques, and outcomes.
In all TGD people using GAHT, histological changes have been reported.
Using testosterone GAHT, ovarian cortical and stromal changes were reported by various studies. In most studies, persistent activity in folliculogenesis can be concluded based on the descriptions of the follicle count, distribution, and oocyte retrieval yield. However, there may be a negative effect on the fertilization rate in the presence of testosterone. Reports of successful ovarian stimulation, fertilization, pregnancies, and live births have been published, describing cases with and without testosterone discontinuation.
After using oestrogen GAHT, testes are reported to be more atrophic, including smaller seminiferous tubules with heavy hyalinization and fibrosis. Spermatogenic levels varied widely from complete spermatogenesis to meiotic arrest with spermatids, to spermatogonial arrest, Sertoli cells only, or even tubular shadows. Oestrogen and anti-androgen treatment causes higher proportions of sperm abnormalities (i.e. low total sperm count, low sperm concentration, poor sperm motility) or azoospermia. However, after cessation, this may be restored.
Although knowledge of the effect of GAHT is growing, blind spots remain to be uncovered. Therefore, additional research in this specific population is needed, preferably comparing outcomes before and after the start of GAHT. This may help to reveal the pure impact of GAHT on reproductive functioning. Research suggestions also include investigations into the reversibility of the GAHT effect, especially for those who start transition at a young age. Looking carefully at the presented data on GAHT effects on gonads and gametes, the correct advice is to assess and reassess reproductive wishes and preferences repeatedly, and also to explore individual fertility preservation needs during gender-affirming treatment, given the expanding knowledge and therapy opportunities. Finally, concerns regarding long-term health outcomes and quality of life of children born by the use of gametes preserved after exposure to GAHT require prospective follow-up studies.
From: The Public Health Crisis State of Transgender Health Care and Policy. Restar A J et al. 2024. American Journal of Public Health.
The rise of antitransgender legislation in the United States has reached unprecedented levels. At the time of writing (October 2023), there were 574 bill proposals explicitly directed at transgender populations in 49 US states, of which 83 have been signed into law. These bills aim to restrict the rights and freedoms of transgender persons, particularly children and adolescents, in areas of health care and society such as employment, education, sports, and public facilities, effectively excluding transgender persons from participating in civic life.
The impact of such antitransgender policies extends far beyond legal and political spheres; it is a critical public health crisis that threatens not only access to care but also the physical and mental well-being and survival of the more than 1.6 million transgender people in the United States.
At the core of this crisis is the deliberate denial of basic human rights and autonomy of a population for a malevolent, politically convenient, and irrational agenda. While the provision of gender affirmation (i.e., services that encompass a range of psychological, behavioural, medical, or legal interventions designed to support one’s gender identity) remains highly politicized, we, as scientific, medical, and legal communities must learn to combat the spread of disinformation and misinformation on this topic as well as policies that purposefully mischaracterize the science. The current wealth of evidence, as supported by multiple established medical organizations like the American Medical Association and the current standards of transgender health care, point to published findings indicating that high-quality, gender-affirming care is an integral protective factor for the mental health and well-being of transgender persons.
The impact of antitransgender legislation on the mental health of transgender individuals cannot be overstated. Transgender people face significant mental health challenges because of discrimination and stigma, and the banning of gender-affirming care, in particular, can lead to trauma and other severe mental health consequences, such as suicide attempts, severe psychological distress, and depression.
This is a crisis for public health and for mental health systems, in particular. Besides gender-affirming care itself, to our team’s knowledge, there are currently no behavioural, social, or structural interventions tailored to transgender populations that have been demonstrated to prevent or reduce adverse mental health symptoms and outcomes. To buffer the impact of antitransgender policies nationwide, greater resources must be invested in scalable interventions to improve family support, promote social connectedness, and build transgender individuals’ and communities’ capacity for empowerment and resistance.
The physical and physiological health consequences of antitransgender legislation are equally devastating. For instance, the denial of gender-affirming care can trigger and lead to myriad adverse physical and physiological health outcomes and consequences, such as hormone imbalances, increased cancer risk, and increased risk of HIV and other sexually transmitted infections. Indeed, some states have reported a chilling effect amid the enforcement of antitransgender policies, leaving providers and mental health professionals concerned that their practices might be penalized and that their patients’ health and safety might be jeopardized. Similar chilling effects have occurred in that transgender patients have hesitated to seek necessary care beyond gender-affirming care such as primary care or routine health checkups for fear of being targeted. In addition, these antitransgender policies may force transgender persons who cannot flee to sanctuary states to conceal their transgender identities and disengage from lifesaving care, thus leading to unmitigated health-harming effects. These antitransgender policies can lead to increased rates of violence and victimization, too, which can result in physical injuries and trauma. As political motivations drive an antitransgender policy landscape, public sentiment follows, emboldening hate groups and dangerous subpopulations in society who wish to eradicate transgender people.
Investing in community-engaged and community-led research, programs, and policy initiatives (e.g., the Trans Legislation Tracker, Centre for Applied Trans Studies) is also crucial to ensure that such responses are community-driven and that they saliently address pressing health and legal needs and directly benefit transgender communities. In addition, it is important to collaborate with other health equity scholars exploring and expanding concepts and strategies on resilience, racial equity, disability rights, Indigenous well-being, and reproductive health, among other topics, given the intertwining impacts of transgender health and policies in these areas, and that health and legal professionals will also encounter transgender people among their target population. Increased investments in rigorous research methodologies are necessary to strengthen evidence, address research and policy gaps, and combat misinformation.
Antitransgender policies reflect malicious attempts by those in power to pit the public against a highly marginalized group and avoid addressing critical economic and social issues that affect everyone (e.g., housing stability, infrastructure maintenance and expansion, climate change). The epidemic of antitransgender policies aims to regress decades of medical, public health, and policy progress, placing our achievements at a perilous crossroads. Where there is legislation that restricts a specific population’s lives and human rights, there are multiple negative and inequitable consequences—as with the case of banning abortion rights, adverse birth outcomes and increased mortality were a consequence. Respect for privacy, bodily autonomy, and the preservation of human rights for transgender people must be core ethical components of current and future health policies, and communities of medical, public health, and policy professionals must proactively oppose legislation that undermines public health responses. These actions are necessary components to achieving health equity for all.
From: Transgender health and the impact of aging and menopause. Cheung A, Nolan B and Zwickl S. 2022. Climacteric.
Gender affirming hormone therapy (GAHT) is used by many transgender people to reduce gender incongruence and improve psychological functioning. As GAHT shares many similarities with menopausal hormone therapy, clinicians supporting people through menopause are ideally placed to manage GAHT. This narrative review provides an overview of transgender health and discusses long-term effects of GAHT to consider when managing transgender individuals across the lifespan. Menopause is less relevant for transgender individuals who take GAHT (often given lifelong) to achieve sex steroid concentrations generally in the range of the affirmed gender.
For people using feminizing hormone therapy, there is an elevated risk of venous thromboembolism, myocardial infarction, stroke and osteoporosis relative to cisgender individuals. For trans people using masculinizing hormone therapy, there is an increased risk of polycythemia, probable higher risk of myocardial infarction and pelvic pain which is poorly understood.
Proactive mitigation of cardiovascular risk factors is important for all transgender people and optimization of bone health is important for those using feminizing hormones. With a lack of research to guide GAHT in older age, a shared decision-making approach is recommended for the provision of GAHT to achieve individual goals whilst minimizing potential adverse effects.
There are many ways in which a trans person may affirm their gender; changing names, pronouns or gender expression, voice therapy, hair removal, using hormone therapy and/or surgery – all of which can significantly improve mental health, gender dysphoria and quality of life.
Research on the effects and adverse effects of GAHT is evolving and in its infancy. Much of our understanding of the effects and adverse effects of GAHT has been gained from well-characterized retrospective analyses and observational cohort studies from North America and Europe, often compared to population samples which will be summarized in this review. Long-term adverse effects are not definitive and become more relevant as individuals age and develop co-occurring medical conditions.
Trans people as a whole face significant marginalization worldwide, including in health care. Difficulty accessing basic medical as well as gender affirming care are frequently reported. Even when being able to access gender affirming care, there remains low-quality evidence to guide the medical treatment of trans people overall and health provider knowledge of trans health remains frequently suboptimal. Healthcare avoidance because of fear of misgendering, discrimination and mistreatment is extremely common, which contributes to poor health. Moreover, the experience of widespread social stressors (social isolation, violence and hate crimes, unemployment) resulting in economic and legal marginalization leads to minority stress, in turn exacerbating poor physical and mental health outcomes.
It is not surprising that trans people have an elevated risk of many chronic health conditions compared to their cisgender counterparts, including chronic obstructive pulmonary disease, depression, hepatitis, HIV, schizophrenia, substance use disorders as well as obesity and other liver conditions. More than 60% report a history of diagnosed depression or anxiety and over 40% have attempted suicide. Rates of death by suicide are more than two-fold greater than for cisgender populations and significant disparities exist for all-cause mortality, especially among trans people presumed male at birth (with feminine or non-binary identities) and trans people of colour. The health inequity faced by trans people globally is a major public health concern.
In 2019, the World Health Organization in its International Classification of Diseases 11th Revision (ICD-11) redefined and reclassified ‘Gender Incongruence’ from the ‘Mental Health’ chapter into a newly established ‘Sexual Health’ chapter, reflecting modern understanding of gender identity. Gender diversity is not a mental health condition, and reclassification sought to reduce stigma and aid access to gender affirming health care.
Aging trans adults have unique challenges. Fear of mistreatment in older care, isolation and loneliness exacerbated by trans identity, increased vulnerability to financial stressors, perceived lack of agency, and healthcare system and provider inclusivity are major concerns. This is compounded by a need for increased healthcare provider interaction with the multiple chronic disease burden exacerbated with aging.
For trans people who take GAHT, whether it be testosterone or estradiol, there remain minimal data on how to manage GAHT with aging, whether there are higher risks with commencement in older age or whether the dose needs to be reduced over time. There is no age at which GAHT is absolutely contraindicated, and in fact, trans people who commence GAHT in older age report higher quality of life scores compared to younger individuals.
Compromised bone density appears inherent even prior to commencement of GAHT. Trans women have lower areal BMD at baseline relative to cisgender men. In addition, lower hand grip strength, lower forearm muscle area and lower 25-hydroxyvitamin D concentrations suggest that lower areal BMD may be related to lifestyle factors such as less physical activity or social isolation.
Estradiol concentrations achieved with GAHT are also important. Trans women with low estradiol (<182 pmol/l) have significant reductions in areal BMD over time and increased bone remodeling markers. In trans men who started GAHT aged <50 years, bone remodeling markers increased, but in those aged >50 years (presumed postmenopausal) bone remodeling markers decreased over the first 12 months of testosterone therapy. Concerns regarding compromised bone microstructure and fracture risk appear to be relevant for trans women only and lifestyle factors may reduce attainment of peak bone mass.
Provision of safe, affirming healthcare environments is essential to reduce health disparity and optimize health outcomes for trans people. GAHT has significant mental health, physical health and quality of life benefits regardless of age at commencement and is often continued lifelong. With aging, the mitigation of cardiovascular risk factors is important for all individuals, and optimization of bone health through ensuring adequate vitamin D levels, dietary calcium intake and regular weight bearing exercise is additionally important for trans people on feminizing hormone therapy. Given a lack of research on the management of GAHT with aging, a shared decision-making approach is recommended to ensure individual goals are attained whilst minimizing potential medical risks.
From: How gender theories are used in contemporary public health research. Hammarstrom A and Hensing G. 2018. International Journal for Equality in Health.
Public health research often focuses on gender differences within certain diagnoses, but so far research has failed to explain these differences in a satisfactory way. Theoretical development could be one prerequisite for moving beyond categorical thinking. The aim of this paper was to analyse how gender theories have been used in public health research in relation to various methodological approaches.
Gender theories were used in eight different ways: 1. to test hypotheses, 2. integrate theories, 3. develop gender concepts and models, 4. interpret findings, 5. understand health problems, 6. illustrate the validity of other theories, 7. integrated into a gender blind theory, as well as to 8. critique of other gender theories. The strategies applied seemed independent of the health aspects of the papers. However, the methodologies were of importance, indicating that both theoretical papers and papers using qualitative methodologies used almost all available strategies, while papers using quantitative empirical research used a limited number of strategies.
International research shows that substantial gender differences exist within certain major diagnoses, such as hypertension and depression. However, researchers have so far failed to explain these differences in a satisfactory way. This might in part be related to the fact that public health studies often favour empirical research while the researchers lack strong theoretical frameworks. Thus, much research is devoted to replicating previously known gender differences in health status rather than to explain their origin, which also might contribute to the preservation of gender stereotypes. In order to find better explanations for gender differences in health status we need to use gender-related concepts, models or theories, yet there is still a lack of development of gender theories in public health research.
Gender theoretical development is central in the process of moving beyond categorical thinking. In gender research, there is a need for questioning the dominating epistemology in medicine as well as for gender theoretical development including power analyses as well as analyses of differences within the group of men/women.
Gender theories were used to:
- test hypotheses
- be integrated in various parts of the paper
- develop gender concept and models
- interpret empirical findings
- understand health problems
- illustrate the validity of theories with health status as an example
- be integrated in traditional gender blind theories
- critique other gender theories
There was a notable lack of focus (apart from one paper about coronary heart disease) on major public health problems like cancer, diabetes, cardiovascular diseases and health behaviours. Furthermore, none of the studies were devoted to better understanding prevention and health promotion from a gender perspective.
interestingly, all of the gender theories featured in the reviewed papers were developed outside the field of public health/medicine, mainly in social science. In addition, the theories mirror the wide range of perspectives that exist in gender research.
A problem within the field of public health research, is that theories are generally underdeveloped. However, there is an increasing theoretical interest in health promotion. This interest has resulted in evidence that public health interventions developed within an explicit theoretical framework are more effective than those performed without a theoretical base. Thus, theories are useful in explaining why certain interventions are successful while others are not. Our study identified no gender theoretical paper within the field of health promotion. Through gender theoretical development, the effects of public health interventions can be improved for both men and women with various backgrounds.
All of the gender theories identified in this review were developed outside the field of public health. In addition, the surprisingly weak theoretical interest in the health outcomes, in combination with the lack of focus on the most common public health diseases, may reflect the lack of public health researchers within our analyses. Among the 33 papers analysed, only four had authors from the field of public health. Consequently, there is an urgent need for public health researchers to engage in gender theoretical research. Our findings provide a stepping stone to further studies within the field.
This is the first study to analyse how gender theories have been used in public health research. Eight ways were identified of using gender theories within the field of gender and health. The methodologies were of importance for the strategies; both theoretical papers and papers using qualitative methodologies used almost all available strategies while papers using quantitative empirical research used a more limited range of strategies. Thus, there is a potential for quantitative studies to improve their use of gender theories.
Nancy Krieger argues for the need of theories as a way of improving public health research, to avoid errors, spark new ideas, and enable us to be critical of studies. She argues “…by making conscious use of epidemiological theory and having informed debates over the different theoretical perspectives in play we stand a better chance of producing epidemiological knowledge truly useful for preventing disease, promoting health equity and improving people’s health.” And to that we would add: …to move beyond categorical thinking in relation to research on gender and health.
Key Literature References
*** Cancer care for transgender and gender-diverse people: Practical, literature-driven recommendations from the Multinational Association of Supportive Care in Cancer (2025), by Elizabeth J. Cathcart-Rake, et al., published in CA: A Cancer Journal for Clinicians
(Notable) *** Fertility in transgender and gender diverse people: systematic review of the effects of gender-affirming hormones on reproductive organs and fertility (2025), by C De Roo, et al., published in Human Reproduction Update
*** Prevalence of Cardiac Arrhythmias in Transgender and Nonbinary Adult Community Health Center Patients (2025), by Ayelet Shapira-Daniels, et al., published in the journal LGBT Health
(Notable) *** The Public Health Crisis State of Transgender Health Care and Policy (2024), by Arjee Javellana Restar, et al., published in the American Journal of Public Health
(Notable) *** Transgender health issues addressed in research on telehealth use: a scoping review (2024), by Susanne Gahbauer & Daniela Haluza, published in Frontiers in Sociology
*** Impact of Gender-Affirming Hormonal Therapy on Cardiovascular Risk Factors in Transgender Health: An Updated Meta-Analysis (2024), by Saad Ur Rahman, et al., published in JACC: Advances
(Notable) *** Transgender health and the impact of aging and menopause (2023), by A. S. Cheung, et al., published in Climacteric
(Notable) *** Suggestions for Improving Healthcare for Transgender and Gender Diverse People in the United States (2022), by Jae Puckett, et al., published in the International Journal of Transgender Health
*** Increasing Access to Care for Transgender/Gender Diverse Youth Using Telehealth: A Quality Improvement Project (2022), by Meredith R. Russell, et al., published in the journal Telemedicine and e-Health
(Notable) *** Health and Health Care Among Transgender Adults in the United States (2022), by Ayden I. Scheim, et al., published in Annual Review of Public Health
*** Viewpoints: Telemedicine in Transgender Care: A Twenty-First–Century Beckoning (2020), by Malke Asaad, et al., published in Plastic & Reconstructive Surgery
(Notable) *** How gender theories are used in contemporary public health research (2018), by Anne Hammarström & Gunnel Hensing, published in International Journal for Equity in Health
*** Determinants of transgender individuals’ well-being, mental health, and suicidality in a rural state (2018), by Adina Smith, et al., published in Journal of Rural Mental Health
>> (Chapter 12) What major issues have been researched with older adults who identify as transgender or non-binary?
by Ian Cameron
Overview: Research in this area is quite extensive and there are are several themes that emerge in the full body of related literature. Here are some key examples:
>>> From: Getting old in the desired gender: a systematic review on aging diseases in transgender people. 2025. Ceolin, Papa, Scale, Sergei, Garolli Journal of endocrinological investigation
Notes the principle conditions are cardiovascular, higher risk of chronic diseases, depression and a reluctance to take part in screening programmes. The prevalence of homophobia, transphobia, rejection, and discrimination experienced by TGD individuals, collectively termed “minority stress,” disproportionately impacts their overall health and carries significant clinical implications.
With the rising number of TGD individuals, there is a growing focus on the long-term impacts of GAHT. The limited existing studies on older TGD individuals indicate that, beyond the inherent risks of chronic diseases, there is a noteworthy cognitive and psychiatric risk that should not be overlooked. Additional research is imperative to elucidate the underlying pathophysiological mechanisms. This, in turn, will enhance awareness among healthcare professionals and contribute to ensuring the successful aging of individuals experiencing gender incongruence.
Findings underscore the importance of addressing the specific or unique needs of TGNC older patients to promote positive or satisfactory experiences in behavioural healthcare. Three themes emerged: (1) engaging with behavioural healthcare practitioners who offer compassionate, patient-centred care; (2) accessing and utilizing culturally tailored peer-support groups; and (3) receiving equitable access to gender-affirming care and social services.
262,000 people in the UK identify as transgender and gender diverse (TGD), and this population is believed to be growing. As the population is aging, an increase in older TGD people accessing health and social care can be anticipated. Despite a recent expansion in research exploring the TGD population, older TGD people are often excluded from the narrative. This review aims to address gaps in the literature by exploring the complex ways older TGD adults access health and social care and how this affects health outcomes with a specific focus on dementia.
Older TGD adults face many barriers when accessing health and social care including experiences of discrimination, gatekeeping by healthcare professionals and limited access to services. These barriers impact on health outcomes in this population and their interactions with the health and social care system. There are high reported rates of poor physical and mental health, including HIV, mental illness and issues associated with gender-affirming treatment. Older TGD people are also reported to be at an increased risk of dementia, which is partly due to high incidences of dementia-associated risk factors. The epidemiology and experiences of older TGD people living with dementia are largely unknown due to limited research. However, the available literature suggests the current health and social care system is ill-equipped to manage their needs.
Greater research exploring the major health problems faced by this population is needed, to address health inequalities. Several approaches have been suggested to help improve services for older TGD people including, expert patient programmes, co-production, and a systems approach.
Providing competent health and social care for older people can be complex and multi-faceted with 54% of >65-year-olds living with long-term health conditions (Kingston et al].Therefore, it is likely that older TGD people will have substantial medical needs, alongside experiencing additional challenges linked to their TGD identity when accessing the health and social care system. Medical conditions affecting cognitive function place a significant strain on the health and social care system. An estimated 50 million people worldwide are living with dementia and this figure is predicted to reach 152 million by 2050 (Patterson). Dementia is known to be associated with many modifiable risk factors including smoking, alcohol use, depression, social isolation, and physical inactivity (Livingston et al.). Despite dementia having such a high-profile role in geriatric health and social care, there is an absence of literature exploring the prevalence and experiences of TGD people living with dementia. Therefore, it is crucial to prioritize research of this community to provide an evidence base for the development of health and social care systems to improve the provision of care.
Older TGD people have high rates of suicidal thinking and behaviour, with a Swedish study reporting every third participant had seriously contemplated suicide (Fabbre & Siverskog). Although suicide rates in the TGD population are thought to decrease with age, they were significantly higher compared to the general population (Grant et al.). High suicide rates are not exclusive to Sweden, with a US study finding 41% of their participants had previously attempted suicide (Clements-Nolle et al.; Grant et al.).
The well-established connection between mental and physical health is also applicable to the older TGD population. Experiences of stigma and discrimination are associated with adverse physical health outcomes (Lambrou et al). As a result, older TGD adults may find themselves caught in a detrimental cycle where societal discrimination heightens their risk of poor health outcomes. This in turn may heighten dependence on health and social care services, exposing them to further discrimination, potentially exacerbating both mental and physical health issues.
One way this problem could be addressed is by providing gender-affirming care, which can promote improvements in mental health (Johnson et al). Appreciative inquiry and partnership may be a useful approach for developing acceptable services (Page et al). Some research also supports oestrogen treatment as being beneficial for improving rates of depression in transgender males (Ettner).
One area that has been studied is the long-term impact of hormone therapy use on venous thromboembolism (VTE) risk in TGD people (Balcerek et al; Delgado-Ruiz et al; den Heijer, 2017). Getahun et al) found there was a 4-fold increased risk of VTE in transgender women taking hormone therapy for eight years compared to two years. Despite this, guidelines still largely rely on research conducted on cisgender men with testosterone deficiency or cisgender women receiving menopausal hormone therapy (Slack & Safer).
TGD adults are more at risk of cardiovascular disease (CVD) and future cardiovascular episodes (e.g. myocardial infarction, VTE, stroke) in comparison with the cisgender population. This may be for various reasons; for example, higher prevalence of smoking (Balcerek et al.) and poor physical health (Fredriksen-Goldsen et al).
In summary, TGD adults, especially transgender women, may have increased risk factors for CVD, and people who are high risk should be offered closer monitoring of their health. However, there is insufficient evidence to propose separate screening recommendations for the older TGD population.
Barriers to accessing appropriate care exist across various sectors of the health and social care system, encompassing primary care, mental health services, transgender health clinics and long-term nursing care (Dhillon et al; Fabbre & Siverskog,; Finkenauer et al; Willis et al). This indicates that challenges associated with providing TGD-affirming care are systemic and institutional (Willis et al), a situation likely exacerbated for individuals with intersecting minority identities (Walker et al). Despite the implementation of policies such as the Gender Recognition Act 2004 and Equality Act (2010), inconsistencies persist in the extent and quality of TGD care.
It is important to consider that older TGD adults have probably experienced lifelong discrimination and, as a result, anticipate discriminatory behaviour every time they access the health and social care system (Benbow & Kingston). Consequently, individuals may delay receiving care (Seelman et al), which can worsen health and wellbeing outcomes (Walker et al). Consistent with this, Seelman et al) found that delayed receipt of care due to discrimination had a greater influence on health outcomes than not receiving TGD-inclusive care. Although, contrary to the main body of literature, this highlights the pivotal role that discrimination plays in determining health outcomes for the older TGD community. Furthermore, experiences of discrimination may worsen with age as older TGD people are vulnerable to “double discrimination” from both ageism and transphobia (Benbow et al.)
TGD people frequently encounter healthcare professionals who lack knowledge of basic TGD health issues. One study reported that 50% of respondents had experienced having to teach their healthcare professional about fundamental TGD health needs (Grant et al). Reflecting this, Willis et al. described TGD people as “reluctant educators and self-advocates”. Members of the TGD community reported feeling burdened by this role (Siverskog) and some perceived healthcare professionals’ lack of knowledge as an “unwillingness to investigate further” (Willis et al). For older TGD patients, these repeated, often lifelong, experiences may result in low confidence in health and social care services (Smolle & Espvall). In contrast, some patients have reported positive experiences,
As well as gaps in the knowledge of healthcare professionals, there is a disconnect between TGD people and their knowledge of what services and facilities are available (Witten).
It has been suggested that TGD people are at an increased risk of developing dementia than the general population (Guo et al). This may be due to the increased prevalence of health problems and risk factors associated with dementia (Davis et al.; Livingston et al), including depression, HIV, smoking, physical inactivity, cardiovascular disease, alcohol consumption and hypertension (NICE).
In conclusion, there is a gap in current literature by offering an overview of the older TGD population’s interactions with the health and social care system and the impact this has upon health outcomes and needs, with a broad scope of review throughout. Although it is not comprehensive and there are some limitations, such as age range. Another limitation of the study is the varying sample sizes and different representations of transgender women, men, and non-binary/gender diverse individuals. It is too simplistic to combine the experiences of these groups under the single label of TGD. In addition only TGD populations n wealthier countries were considered.
>>> From: Cognitive functioning in older transgender individuals receiving long-term gender-affirming hormone therapy. 2025 Van Hessewijk et al.. International Journal Of Transgender health.
Cognitive functioning can be negatively influenced by age, cardiovascular risk (CVR) and mental health challenges, and sex-hormones can have neuroprotective effects. Little is known about cognitive functioning in older transgender individuals receiving long-term gender-affirming hormone therapy (GHT). In a previous, smaller study, cognitive differences between transgender women and cisgender groups were minimal yet statistically significant.
Small cognitive differences between transgender men and cisgender groups do not suggest adverse or beneficial long-term testosterone effects on cognitive functioning. However, transgender women had lower cognitive functioning than cisgender groups, which was largely explained by mental/social health. This warrants further research and clinical awareness of mental and cognitive health in older transgender individuals.
This study assessed cognitive functioning differences between older transgender women and men receiving long-term GHT and age-matched cisgender women and men. Overall, transgender women had significantly and substantially lower cognitive functioning profiles compared to both cisgender groups, which was most prominent for episodic memory.
In light of the general lack of information and clinical guidelines regarding health outcomes in older transgender individuals, this study provides valuable information on cognitive functioning and potential risk factors among older long-term GHT receiving transgender women and men. Transgender women had significantly and substantially lower cognitive functioning compared to cisgender groups, which was largely explained by a higher prevalence of mental health challenges. Also, for transgender men, mental health challenges partly explained cognitive differences with cisgender men. Importantly, however, the small cognitive differences between transgender men and cisgender groups do not suggest adverse or beneficial long-term testosterone effects on cognitive functioning. These findings warrant further research and clinical awareness of mental and cognitive health and other potential risk factors such as minority stress and sex-hormone exposure, especially in older transgender women.
>>> From: Gender-affirming hormone therapy, mental health, and surgical considerations for aging transgender and gender diverse adults. 2023 Iwamoto, Defreyne and Rothman. Sage Journal . Therapeutic Advances in Endocrinology and Metabolism
Gender-affirming care may include gender-affirming hormone therapy (GAHT), gender-affirming surgery, and gender-affirming mental health care, depending on the individual goals of each transgender and gender diverse (TGD) person. Most data informing our knowledge about TGD medical, mental health, and surgical outcomes come from large European cohorts with a small proportion of older adults. The Amsterdam Gender Clinic, which has provided gender-affirming care since 1972, reportedly had 700 of 4432 (16%) transfeminine (i.e. person with male sex recorded at birth who has a female/feminine gender identity) and 250 of 2361 (11%) transmasculine (i.e. person with female sex recorded at birth who has a male/masculine gender identity) adults reach the age of 60 years or above in 2015. The European Network for the Investigation of Gender Incongruence (ENIGI) has published many cross-sectional and prospective results on a variety of topics related to gender-affirming care. In 2016, Dekker et al. described the ENIGI Endocrine protocol, which has included TGD persons since 2010, as monitoring cohorts with relatively young median ages but a wide range of ages among transfeminine (n = 333, median age = 30 years, range = 16–65) and transmasculine (n = 343, median age = 24 years, range = 16–51) adults. By 2022, ENIGI had 1261 transfeminine and 1411 transmasculine patients in its cohort, as reported by Cocchetti et al., with a growing proportion of older TGD adults being followed. Data from ENIGI are currently representative of a younger TGD population but hold promise for future studies assessing older TGD adults and age-related differences in health outcomes impacted by gender-affirming care.
As it is vital to provide gender-affirming care to older TGD persons in a safe and comfortable environment that aligns with individual goals, we aimed to write this perspective review to offer considerations based on existing data while recognizing the above limitations. We review current masculinizing and feminizing GAHT factors surrounding CVD and metabolic diseases, cancer, bone health, and cognitive impairment, highlighting several conditions impacted by advancing age. We also provide discussion of mental health care and gender-affirming surgery in older TGD adults.
>>> From: Transgender and Gender Diverse People’s Fear of Seeking and Receiving Care in Later Life: A Multiple Method Analysis. 2023. Walker, Powers and Witten. Journal Of Homosexuality. Taylor and Francis.
The purpose of the current research is to understand concerns about receiving care in a sample of transgender, gender nonbinary, and gender diverse (TGD) adults across the lifespan. A total of 829 participants, predominantly from the United States and Canada, aged 18–70, completed the Trans Metlife Survey on Later-Life Preparedness and Perceptions in Transgender-Identified Individuals (TMLS) section on caregiving and are included in this study. We found middle-aged adults, people of Colour, and people living with a disability reported the highest level of concern for their ability to function independently because of financial resources, physical concerns, cognitive impairment, or a lack of someone to care for them. Researchers found five overarching thematic categories: (a) No concerns, (b) Anticipated discrimination, (c) Loss of control, (d) Quality of life, and (e) General concerns. Practice implications include recommendations for practitioners to develop care plans with TGD residents and clients to learn the best strategies for affirming their gender identity (e.g., clothing preferences) and to assist TGD residents and clients with the completion of advance directives to allow them to outline their end-of-life care plan, including instructions for gender affirmative care in the event of incapacitation (e.g., dementia, stroke).
>>> ‘I’m going to live my life for me’: trans ageing, care, and older trans and gender non-conforming adults’ expectations of and concerns for later life. 2020. Willis et al. Cambridge University Press
While research on the health and wellbeing of older lesbian, gay and bisexual adults is gradually expanding, research on older trans and gender non-conforming (TGNC) adults lags behind. Current scholarship about this group raises important questions about the intersection of ageing and gender identity for enhancing care and support for older TGNC adults and the lack of preparedness of health and social professionals for meeting these needs. In this paper, we examine the accounts of 22 TGNC individuals (50–74 years) on the topic of ageing and unpack their concerns for and expectations of later life. We present qualitative findings from a study of gender identity, ageing and care, based in Wales, United Kingdom. Data were generated from two-part interviews with each participant. Four key themes are identified: (a) facilitative factors for transitioning in mid- life Willis et al. o later life; (b) growing older as a new lease of life; (c) growing older: regrets, delays and uncertainties; and (d) ambivalent expectations of social care services. We argue that growing older as TGNC can be experienced across a multitude of standpoints, ranging from a new lease of life to a time of regret and uncertainty. We critically discuss emergent notions of trans time, precarity and uncertainty running across participants’ accounts, and the implications for enhancing recognition of gender non-conformity and gender identity in social gerontology.
Under the Equality Act 2010 in England and Wales, ‘gender reassignment’ is a protected characteristic and includes protecting individuals who are pre- and post-transition from discriminatory treatment by service providers (arguably, this does not offer the same legal protection for people who identify outside the gender binary model of male–female, e.g. as non-binary). This is a pivotal time for TGNC citizens in the UK. In 2018, the UK Government initiated a consultation on proposed reforms to the Gender Recognition Act 2004, partly based on a 2016 report from the House of Commons Women and Equalities Committee. Proposed questions in the consultation included whether individuals should be granted the right to self-define their gender identity rather than having to prove this through the current medicalised measures embedded in the 2004 Act (Government Equalities Office). For example, a current requirement is to have a documented mental health diagnosis of gender dysphoria (now reclassified as ‘gender incongruence’ under the World Health Organization (WHO) International Classification of Diseases (ICD)-11) (House of Commons Women and Equalities Committee). This proposal marks a positive shift towards a more individual-centred, self-determining process.
These policy efforts unfold during a time period when hate crime against TGNC individuals has increased by 32 per cent in England and Wales between 2016/17 and 2018/19; this represents crimes reported to the police (Home Office). Anecdotal accounts point to a parallel increase in negative media representation over the course of 2017, both in the UK and internationally (Barker), in which trans people and identities are frequently represented as ‘monstrous’ or ‘dangerous’ (Krutkowski et al.). The recent government consultation on proposed changes to the Gender Recognition Act 2004 evoked intensified media responses from trans-exclusionary groups and individuals voicing anxieties about the perceived violation of women-only spaces by cisgender men posing as trans women (Krutkowski et al). Such arguments reiterate the negative discourse of ‘dangerous’ attached to trans adults’ identities in the popular press.
Four themes speak directly to the question, ‘How do TGNC identities and life experiences shape older individuals’ concerns about and expectations of ageing and later life?’ These are: (a) facilitative factors for transitioning in mid- to later life; (b) growing older: a new lease of life; (c) growing older: regrets, delays and uncertainties; and (d) ambivalent expectations of social care services in later life. Names below are pseudonyms selected by participants.
Theme 1: Facilitative factors for transitioning in mid- to later life
For most participants, gender transitioning was associated with a journey of undergoing social and medical changes (medical transitions encompass hormone therapy treatments and gender-affirming surgeries, such as vaginoplasty and breast implants for trans women and phalloplasty and mastectomy for trans men). The majority were on this journey at different stages – from having recently commenced hormone treatment and waiting on referrals to UK-based gender identity clinics through to having received final surgery in the preceding 12 months. Two participants had transitioned at earlier life-points – one person through a private clinic overseas (an arguably faster process) and another having commenced this journey in the 1970s.
Many individuals described living as TGNC in secrecy in young adulthood (during their teens, twenties and early thirties) and not disclosing their TGNC identity to others to avoid negative repercussions, and not feeling adequately equipped and confident to ‘come out’ as TGNC during earlier lifestages. This was partly compounded by the lack of information about TGNC lives prior to the arrival of the internet in the 1990s. Accessing the internet heralded the emergence of online communities of TGNC individuals who were geographically dispersed (Whittle et al).
Theme 2: Growing older: a new lease of life
Participants ranged in age from 50 to 74 and as such differed greatly in terms of lifestages such as their transition journey (for those transitioning), family circumstances and employment status. Consequently, whether people have had discussions with others about growing older or planned for the future depends on the confluence of these factors. Many of the participants were not concerned about growing older and had not given it much consideration, preferring to focus on living in the moment and taking ‘each week as it comes’:
The inclination to live in the moment means that many of the participants did not often discuss growing older with other people. Moreover, whether people have thought about their health in later life is influenced by how fit and healthy they feel currently. Most of the participants self-reported as physically well and did not have pressing health concerns. However, several of the participants expressed concerns over the increased health risks of taking hormones in older age and the perception that hormone levels are not well monitored by GPs and health-care services. This was a particular worry for Gabriella (56), with a family history of heart problems:
Theme 3: Growing older: regrets, delays and uncertainties
Where people are in their transition journey can impact on an individual’s subjective understanding of ageing. When reflecting on their current age and life circumstances, some participants conveyed regret and sadness for missed opportunities earlier in their lives. Although Barbara did not dwell on getting older, she expressed sadness that she will be 70 years by the time she completes her medical transition:
Theme 4: Ambivalent expectations of social care services in later life
Participants expressed many of the same concerns about needing to access social care services or long-term care provision as might be expected from the general population. This included concerns about a perceived loss of independence, dignity and respect as older people in care settings (Hill et al). Specific to TGNC identities, participants held concerns about being treated with dignity and respect in long-term care settings in relation to maintaining personal appearance. Women participants mentioned the importance of being appropriately dressed and the high dependency of service users on care staff to maintain body/facial hair and wig maintenance, where their mental capacity may be declining or fluctuating:
In summary, although it is legally possible to social transition in the UK, starting off by changing name by deed poll, soft and full transition is a lengthy process, clouded in uncertainty by the Cass review, which seems far more political in its emphasis than medical. Transgender individuals face considerable barriers to receiving care and treatment, in having to negotiate gate keepers. There is a lack of research to inform providers. Given the age range and social background, each transgender person is unique, with an equally unique story.
What is a puzzle is the waiting times for an appointment with a GID. Anything between 4 and 6 years in the UK. Yet there are clinics available, as discussed, for a trans population of about a quarter of a million, and not all will want and need referrals at the same time. Yet 70,000 knee replacement are carried out annually by the NHS with a waiting time of about 4 months. 20% of knee replacement patients report dissatisfaction, as opposed to the < 1% of trans people who report dissatisfaction with what is life affirming surgery for many. Is this wating time a pointless ice of gate keeping, designed to put trans people off?
Key Literature References
(Notable) *** Getting old in the desired gender: a systematic review on aging diseases in transgender people (2025), by C. Ceolin, et al., published in Journal of Endocrinological Investigation
(Notable) *** Sexual and Gender Identity Properties and Associations With Physical and Mental Health Among SGM Midlife and Older Adults: Findings From Aging With Pride: National Health, Aging, and Sexuality/Gender Study (2025), by Karen I. Fredriksen-Goldsen, et al., published in Research on Aging
*** “My support groups… have saved my life.”: facilitators of positive or satisfactory experiences in behavioral healthcare for transgender and gender nonconforming older adults (2025), by Nik M. Lampe, et al., published in Aging & Mental Health
*** Mental health outcomes and loneliness in older transgender individuals receiving long-term gender-affirming hormone therapy compared with older cisgender individuals (2025), by Jason O. van Heesewijk, et al., published in International Psychogeriatrics
*** Transgenderism in studies on the health of older adults: a systematic review (2025), by Jônathas de Lima Arruda, et al., published in Epidemiologia e serviços de saúde : revista do Sistema Unico de Saúde do Brasil
(Notable) *** Lived Experiences of Older LGBTQI+ Adults Aged 60 or Older: A Systematic Review and Qualitative Synthesis (2025), by Richard Huntley, et al., published in Journal of Homosexuality
*** Mental health of gender minority older adults in the United States: A systematic review (2024), by Madeline Kerr, et al., published in the journal Psychology of Sexual Orientation and Gender Diversity
(Notable) *** Transgender and gender diverse older people: health, aging and dementia (2024), by Emily Asti, et al., published in the International Journal of Transgender Health
(Notable) *** Healthcare needs and assets of gender diverse older adults: A systematic integrative review (2024), by Lauren Catlett, published in Journal of Nursing Scholarship
*** Navigating aging as transgender and gender diverse individuals: current realities and future public health challenges. A narrative review (2024), by Angela Ruocco, et al., published in Journal of Sex-Specific Medicine
*** Transgender patients and gender-affirming hormone therapy through the mid-life (2024), by Jaya M. Mehta, et al., published in the journal Mauritas
(Notable) *** “I Want to Grow Older With Dignity”: Older LGBTQ+ Canadian Adults’ Perceptions and Experiences of Aging (2024), by Laura Hurd, et al., published in Journal of Applied Gerontology
(Notable) *** Health Disparities among Lesbian, Gay, Bisexual, Transgender, and Queer Older Adults: A Structural Competency Approach (2024), by Nik M. Lampe, et al., published in the International Journal of Aging and Human Development
(Notable) *** Elderly transgender mental health: Global and local challenges (2024), by Anoushka Thakkar, et al., published in Journal of Geriatric Mental Health
(Notable) *** Caring for the Older Transgender Adults: Social, Nursing, and Medical Challenges (2024), by Charalampos Milionis, et al., published in Clinical Nursing Research
*** Cognitive functioning in older transgender individuals receiving long-term gender-affirming hormone therapy (2023), by Jason O. van Heesewijk, et al., published in the International Journal of Transgender Health
*** Gender-affirming hormone therapy, mental health, and surgical considerations for aging transgender and gender diverse adults (2023), by Sean J. Iwamoto, et al., published in Therapeutic Advances in Endocrinology and Metabolism
(Notable) *** Transgender and Gender Diverse People’s Fear of Seeking and Receiving Care in Later Life: A Multiple Method Analysis (2022), by Ruth V. Walker, published in the Journal of Homosexuality
*** A narrative review of literature on the use of health and social care by older trans adults: what can United Kingdom services learn? (2022), by SM Benbow, et al., published in the journal Ageing & Society
(Notable) *** Older trans individuals’ experiences of health and social care and the views of healthcare and social care practitioners: ‘they hadn’t a clue’ (2022), by Susan Mary Benbow, published in Educational Gerontology
*** Social Support in Older Transgender and Gender Diverse Communities in the United Kingdom and Australia: A Comparative Study During COVID-19 (2022), by Michael Toze, et al., published in the Journal of Gerontological Social Work
*** Forgotten lives: Trans older adults living with dementia at the intersection of cisgenderism, ableism/cogniticism and ageism (2022), by Alexandre Baril and Marjorie Silverman, published in the journal Sexualities
*** Stigma, identity and support in social relationships of transgender people throughout transition: A qualitative analysis of multiple perspectives (2022), by Tom O.G. Lewis, et al., published in The Journal of Social Issues
(Notable) *** Worry and Wisdom: A Qualitative Study of Transgender
Elders’ Perspectives on Aging (2021), by Matthew Adan, et al., published in Transgender Health
(Notable) *** The gender-affirmative life span approach: A developmental model for clinical work with transgender and gender-diverse children, adolescents, and adults (2021), by Katherine G. Spencer, et al., published in the journal Psychotherapy
(Notable) *** Worry and Wisdom: A Qualitative Study of Transgender Elders’ Perspectives on Aging (2021), by Matthew Adan, et al., published in the journal Transgender Health
*** ‘I’m going to live my life for me’: trans ageing, care, and older trans and gender non-conforming adults’ expectations of and concerns for later life (2020), by Paul Willis, published in the journal Ageing & Society
*** A Review of Minority Stress as a Risk Factor for Cognitive Decline in Lesbian, Gay, Bisexual, and Transgender (LGBT) Elders (2020), by Anthony N. Correro, published in Journal of Gay & Lesbian Mental Health
*** Inequalities in older LGBT people’s health and care needs in the United Kingdom: a systematic scoping review (2019), by Dylan Kneale, et al., published in the journal Ageing & Society
>> (Chapter 13) What are the key components of resilience that have been researched among people with diverse gender identity?
Overview by Ian Cameron
From: “It saves lives”: Peer support and resilience in transgender and gender diverse communities. Kia H et al. [2023] SSM Qualitative Research in Health. ScienceDirect.
Transgender (trans) and gender diverse (TGD) populations continue to experience significant inequities in social and health outcomes, often in connection with the systemic exposure of these groups to violence, stigma, and discrimination. Despite the promising role of peer support in mitigating adverse impacts of marginalization, this phenomenon remains under-examined.. We also consider the role of peer support in building resilience among participants. Our findings are organized into four interrelated themes that both represent the constituent parts of peer support, and that explicate the connections between peer support and resilience. These include: (1) becoming visible to connect with similar others, (2) sharing embodiment, experience, and space, (3) constructing possibilities of being and collectivizing, and (4) surviving and thriving (at a cost). We leverage our findings to consider implications for research, policy, and practice, one of which includes the need for ongoing inquiry to substantiate the critical role of peer support in promoting health across diverse TGD communities.
In light of the salience of systemic and intersecting stigma, discrimination, and violence that characterizes the structural context of TGD populations, scholars have in recent years started investigating protective factors that serve to buffer against the impacts of these adverse social conditions. Social support, which has long been recognized for its promise in attenuating the negative effects of minority stressors among marginalized groups, has been centred in much of the emerging inquiry in this area.
Critical resilience scholarship, in contrast with earlier writing in this area, situates resilience amid relations of power by redefining the construct as encompassing survival processes that (1) foreground alternatives to the dominant social order, (2) are actively produced and deployed among individuals and collectives affected by adversity, and (3) function as precursors to resistance and structural transformation.
Our findings are organized into four themes, which together explicate how TGD individuals experience peer support across variable contexts, and highlight how these experiences contribute to the resilience of TGD people. These interrelated themes include: (1) becoming visible to connect with similar others, (2) sharing embodiment, experience, and space, (3) constructing possibilities of being and collectivizing, and (4) surviving and thriving (at a cost).
The research promises to advance existing scholarship on peer support in TGD people, and catalyze ongoing inquiry in this area. Indeed, we hope our findings not only serve to strengthen the existing scholarship, but additionally inform future research, policy, and programming concerning the well-being of TGD populations. With greater recognition of the significance of peer support among TGD people, the scholarship on TGD health may more fulsomely account for a critical dimension of lived experience among those in these groups. In turn, policy and practice may also improve to better respond to the evolving priorities of TGD people.
From: Resilience in Transgender and Nonbinary Communities: Adapting Conceptual Frameworks and Addressing Measurement Challenges. Puckett J, Kimball D, Galupo P. [2024] Gender Resilience, Integration and Transformation. Springer Nature
Transgender and nonbinary (TNB) people experience a range of minority stressors, such as discrimination, harassment, and victimization. In addition to reducing these systemic issues, understanding more about resilience and what promotes positive outcomes for this marginalized community is essential. Furthermore, the importance of research on resilience has grown as we see increasing amounts of anti-trans legislation sweeping across the United States. Although we look to resilience research to learn more about what can help TNB people to persevere in the face of marginalization, the findings in this area have been mixed with considerable challenges related to the measurement of resilience.
Measures of resilience often reflect a general ability to “bounce back” from challenges, yet for TNB people, there can also be unique forms of resilience, such as self-defining one’s own gender experience or developing critical consciousness. We seek to address the mismatch between lived experiences of resilience and quantitative measures of resilience for TNB people by presenting a multidimensional conceptualization of resilience in TNB people’s lives.
From: “Focus more on what’s right instead of what’s wrong:” research priorities identified by a sample of transgender and gender diverse community health centre patients. LeBlanc M et al. [2022] BMC Public Health Springer Nature.
Transgender and gender diverse (TGD) people are individuals whose gender identity differs from their sex assigned at birth. While research demonstrates that TGD communities are subject to disparate health outcomes compared to their cisgender peers, health research regarding the TGD community remains limited and researchers rarely center TGD voices and perspectives in their projects. Conducting TGD research without the inclusion of TGD community input can contribute to disenfranchising the population, ignoring community needs, and causing investigators to miss key topics most influential to TGD population health.
Throughout the FG discussions, the need to address the complexity of identities within TGD public health research was repeatedly raised. Participants indicated the need to include and represent a multitude of identities within TGD health research. Participants also spoke about the impact of cultural shifts and changes in language as a contributing factor as to why it is important to recognize complexity of TGD identities in research. TGD participants wanted investigators to be familiar and responsive to the reality of varying identities and open to cultural shifts and changes in language, in order to truly contribute to TGD public health research. Allowing trans-specific research to be inclusive of non-binary identities was highlighted as both crucial and timely.
The stress experienced from interpersonal social stigma and its effect on health was identified as a main research priority in the FGs. Participants shared that their experiences of street harassment and harmful interactions with others were stressors that impact their health and well-being. TGD individuals face a high level of adversity and are subject to oppressive systemic structures and yet subsequently embody resilience. Participants felt that continuing to only evaluate disparities perpetuates harmful narratives about TGD people; measuring resilience can aide in the effort to combat these harmful narratives.
TGD individuals provided input on priorities and topics about social influences on health for future research. The top research priorities and special topics identified by this sample of TGD community health center patients coalesced around the overarching and overlapping themes of the complexities of identity, the impact of structural and interpersonal stigma and discrimination on health and measuring resiliency and not just disparities. The complexity of identities of TGD individuals can be uniquely understood as “embodiment,” a construct that identifies an individual body as simultaneously biological and rooted in social contexts, highlighting the need for investigators to consider and include the complexity and representation of heterogenous identities of the transgender and gender diverse population in research.
The concept of embodiment reflects that we are simultaneously social and biological organisms whose lived experiences cannot be separated from social context . This study sought to gather insights directly from members of the TGD community about research priorities, needs, and topics meaningful to TGD individuals. The approach of integrating TGD communities reflects patient-centered research practices, a recommendation for conducting TGD health research described by participants within this study.
From: Defining and researching the concept of resilience in LGBT+ later life: Findings from a mixed study systematic review. Jurcek A. Et al. [2022] National Library of Medicine Pubmed.
Within the literature, resilience is described as either a trait, an outcome or a process and no universal definition exists. A growing body of research shows that older LGBT+ adults show signs of resilience despite facing multiple inequalities that negatively impact their health and social wellbeing. However, resilience was rarely the primary focus of the studies and was researched using a variety of measurement instruments and conceptual frameworks. Given the socioeconomic disparities, diverse social relations, histories of discrimination and stigma, and acts of resistance that have shaped the lives of older LGBT+ populations, resilience is a topic of growing interest for researchers and practitioners. Clear definitions of resilience and application of resilience theory could help improve methods used to study the concept and lead to more robust findings and the development of effective interventions. Greater clarity on the concept of resilience could also broaden the focus of research that informs policies and practice, and support practitioner training in resilience and the particular experiences of older LGBT+ adults.
Population ageing within global demography is one of the most significant social transformations of the twenty-first century. Projections show that by 2050, the proportion of people over 65 years will increase from 1 in 11 to 1 in 6. The diversity of the ageing population is a significant factor in understanding any challenges and opportunities in the way in which we respond to demographic changes. While lesbian, gay, bisexual, transgender and gender diverse people (LGBT+) face similar challenges to their heterosexual and cisgender peers in later life, an established evidence base demonstrates specific health, social and structural inequalities for LGBT+ older peopl. (We use the term LGBT with a plus (+) sign to signal inclusion of the wide diversity of sexual and gender identities, unless the paper being cited is focused on specific identities). Inequalities are compounded by the cumulative effects of lifelong exposure to prejudice, discrimination, criminalisation and environmental factors nuanced by a wide range of intersecting identities, including socio-economic status, culture, race and ethnicity, disability and religion. These unique circumstances impacting on ageing experience for LGBT+ people pose risks linked to minority stress and stress adaptation in later life.
A definition of resilience in the context of it being a trait which is the capacity to respond and successfully negotiate stressful life events in addition to it being a set of protective factors.
There has been an increasing growth of research into the experiences of LGBT+ ageing internationally, which has attempted to connect with more recent advances in developing theoretical models of resilience both in the LGBT+ population and ageing. The body of research reviewed here has considered the interactional and contextual features of both ageing and LGBT+ identities sometimes without a clear definition of resilience, and the variety of studies tend to show a lack of coherence in the way in which the concept of resilience is utilised and theorised in LGBT+ ageing.
From: Coping, resilience, and social support among transgender and gender diverse individuals experiencing gender-related stress. Gorman K et al. [2022]. Psychology of Sexual Orientation and Gender Diversity.
Transgender and gender diverse (TGD) individuals experience stigma related to their gender identity. However, little research has been conducted exploring how TGD individuals cope with, build resilience from, or obtain support concerning gender-related stress.
In this study, we recruited TGD individuals (n = 30) to elucidate the coping strategies used in response to gender-related stress; to explore how they developed and maintained resilience; and to understand the impact of social support from others in navigating gender-related stressors. Participants completed individual, semistructured, qualitative interviews, which we coded using consensual qualitative research methods. Many participants underscored the strain of having to educate cisgender friends, family, and health care providers about TGD experiences. Participants endorsed using strategic avoidance or modulating their gender presentation to manage gender-related stress. Additionally, participants discussed various intragroup prosocial behaviors (i.e., developing TGD spaces) to sustain resilience and increase or maintain social support. Despite the expansive literature focused on TGD risk, most participants reported significant self-compassion and effective coping strategies for managing gender-related stress throughout their lives. Unique techniques described by our participants that are infrequently discussed in the coping literature on cisgender individuals (i.e., strategic avoidance and intragroup prosocial behaviors) echo those reported by other marginalized group members.
From: Mental health and resilience in transgender individuals: What type of support makes a difference? Puckett J et al. [2019] Journal of family Psychology.
Research has generally shown the benefits of social support, such as the buffering effects on life stressors, yet there has been little empirical investigation of different types of support resources for transgender individuals. We examined family support, support from friends, and connectedness to a transgender community and how these forms of support come together to influence mental health and resilience.
The sample included 695 transgender participants (mean age = 25.52 years, SD = 9.68, range = 16–73; 75.7% White) who completed an online survey. Greater than half of participants reported moderate to severe levels of anxious and depressive symptoms. Family social support had the strongest correlations with symptoms of anxiety and depression (r = −.31 and −.37, respectively, p < .01) and was the only form of support associated with resilience when controlling for other forms of support.
Latent profile analyses revealed 4 groups based on levels of social support from family and friends and community connectedness. Notably, Class 1 (n = 323; 47.1%) had high levels of support from family and friends and high levels of community connectedness. This class had lower levels of depression and anxiety symptoms and higher levels of resilience compared to other classes (Class 2, n = 276, 40.3%, high friend/community, low family; Class 3, n = 47, 6.9%, low support; Class 4, n = 39, 5.7%, high family, low friend/community).
This study highlights the importance of examining support from a more holistic approach and provides insight into unique associations between familial social support and resilience.
Key Literature References
*** Transgender Joy: A Path to Resisting Oppression (2025), unpublished Master’s degree thesis, Morehead State University, Kentucky
*** Worldbuilding: A Theory of Resilience in Transgender and Gender Expansive Young People (2024), unpublished PhD Dissertation, CUNY, by Jennifer DeBower
*** Measures of Resilience: Do They Reflect the Experiences of Transgender Individuals? (2024), by Jae E. Puckett, published in the journal Transgender Health
(Notable) *** “It saves lives”: Peer support and resilience in transgender and gender diverse communities (2024), by Hannah Kia, et al., published in SSM: Qualitative Research
(Notable) *** Resilience in Transgender and Nonbinary Communities: Adapting Conceptual Frameworks and Addressing Measurement Challenges (2024), by Jae A. Puckett, et al., published in the book Gender Resilience, Integration and Transformation
*** Gender Minority Stress and Resilience Measure: A Meta-Analysis of the Associations with Mental Health in Transgender and Gender Diverse Individuals (2023), by Laura C. Wilson, et al., published in Trauma, Violence & Abuse
*** Comparison of Gender Minority Stress and Resilience Among Transmasculine, Transfeminine, and Nonbinary Adolescents and Young Adults (2022), by Jonathan L Poquiz, et al., published in the Journal of Adolescent Health
(Notable) *** Peer support as a protective factor against suicide in trans populations: A scoping review (2021), by Hannah Kia, et al., published in the journal Social Science & Medicine
(Notable) *** “Focus more on what’s right instead of what’s wrong:” research priorities identified by a sample of transgender and gender diverse community health center patients (2020), by Merrily Leblanc, et al., published in BMC Public Health
*** Breaking the binary: Restriction and reclamation of power among transgender and gender diverse young adults (2022), by Danielle Chiaramonte, et al., published in Journal of LGBT Youth
(Notable) *** Defining and researching the concept of resilience in LGBT+ later life: Findings from a mixed study systematic review (2022), by Anže Jurček, et al., published in PLOSOne
(Notable) *** Coping, Resilience, and Social Support among Transgender and Gender Diverse Individuals Experiencing Gender-Related Stress (2022), by Kaitlyn R. Gorman, et al, published in Psychology of Sexual Orientation and Gender Diversity
(Notable) *** The Roles of Gender Affirmation and Discrimination in the Resilience of Transgender Individuals in the US (2020), by Corina Lelutiu-Weinberger, et al., published in the journal Behavioral Medicine
*** Influences of health care access on resilience building among transgender and gender non-binary individuals (2019), by Jessamyn Bowling, et al., published in the International Journal of Transgenderism
(Notable) *** Mental Health and Resilience in Transgender Individuals: What Type of Support Makes a Difference? (2019), by Jae. A. Puckett, et. al, published in the Journal of Family Psychology
*** Demographic and Psychosocial Factors Associated With Psychological Distress and Resilience Among Transgender Individuals (2015), by Emily Bariola, et al., published in the American Journal of Public Health
*** Resilience and collective action: Exploring buffers against minority stress for transgender individuals (2015), by Aron S. Breslow, et al., published in Psychology of Sexual Orientation and Gender Diversity
*** Strength in the Face of Adversity: Resilience Strategies of Transgender Individuals (2011), by Anneliese A. Singh, et al., published in Journal of Counseling & Development
>> (Chapter 14) What are some of the key issues identified in research focusing on concealment, stigma, and disclosure of gender identity?
Introduction
As Brennan, et al. (2021) recognize, concealment is a common experience for gender minority as well as sexual minority individuals, and many gender minority individuals concurrently identify as sexual minority and have concealed both identities. They note that there is consensus in research on concealment behavior that “engaging in concealment behaviors and having a concealable stigma contribute to negative physical and mental health outcomes.” Rood et al. (2017) have observed, “Gender minority individuals might conceal their identity in social contexts in an effort to avoid stigma and victimization. Unfortunately, identity concealment is thought to impact psychological distress in transgender and gender nonconforming (TGNC) individuals.”
Osmetti, et al., 2025 describe many challenges associated with researching concealment among gender minorities, particularly in terms of the emotional stresses associated with non-disclosure of one’s preferred gender identity.
Overview, by Ian Cameron
From: Shortcomings of transgender identity concealment research: a scoping review of associations with mental health. Osmetti L, Allen K. Kozlowski D. [2025] International Journal of Transgender Health.
Empirical research indicates that high rates of mental health issues in members of marginalised population groups are predicted in part by their decisions to disclose or conceal their stigmatized identities from others—a field of study known as outness research. Transgender outness research is a nascent branch of this field. It reflects neither the multidimensional view of disclosure and concealment adopted in other branches, nor the ability to address unique aspects of trans outness, such as the practical challenges of concealment and the difference between concealing one’s gender identity and concealing one’s assigned sex. Consequently, prior literature may not accurately represent the effects of transgender identity disclosure and concealment.
Findings indicate that the issues outlined above remain unresolved, even in the widely-used nondisclosure subscale of the Gender Minority Stress and Resilience Measure, and are rarely recognized as a potential source of error. Although small detrimental effects of concealment and beneficial effects of disclosure on mental health were reported in the reviewed studies, reliable conclusions about these relationships and their importance to health and safety in the trans community cannot be drawn while these shortcomings are overlooked.
Members of some marginalised groups attempt to avoid distal stressors altogether by concealing their stigmatized identity from others at the cost of isolating themselves from supportive communities and suffering the anxieties and negative emotions generally associated with secrecy. For trans individuals, concealment is often motivated by fears of violence and considered a serious, potentially lifesaving matter of personal safety (Rood et al., Citation2017), and may thus be key to understanding and addressing mental health discrepancies in the population.
This review highlighted three key problems that arise when applying extant outness frameworks to trans populations: researchers may conflate assigned sex concealment and gender identity concealment, take for granted that concealment is achievable for all participants, and overlook unique manifestations of the model in nonbinary populations.
The present review summarized the current body of psychological research regarding the disclosure and concealment of trans identities. It highlighted three unresolved problems in the field: the conceptually distinct strategies of concealing one’s gender identity and concealing one’s assigned sex, the practical complexity of concealing a trans identity, and the unique manifestation of concealment in nonbinary people. As concealment decisions are frequently motivated by fears of violence, the benefit of research in this field to health and safety in the broader trans community can be immense if it is conducted thoroughly. Despite their inconsistency and conceptual shortcomings, most of the reviewed papers did provide evidence of a negative correlation between concealment and mental health or a positive correlation between disclosure and mental health. While the existence of relationships between disclosure, concealment, and mental health for trans people is not contested, addressing the issues highlighted in this review and establishing consistent, robust definitions and measurement strategies will greatly enhance our understanding of that relationship and ensure that research findings on the topic are rigorous, reliable, and adequately reflect the real lives and attitudes of trans participants. This will allow research to be of practical benefit to the trans community by informing public policy and healthcare standards and providing accurate information to individuals facing their own disclosure and concealment decisions.
From: Rethinking minority stress: A social safety perspective on the health effects of stigma in sexually-diverse and gender-diverse populations. Diamond L and Alley J {2022] Neuroscience and Biobehavioural Reviews. ScienceDirect.
For over two decades, the minority stress model has guided research on the health of sexually-diverse individuals (those who are not exclusively heterosexual) and gender-diverse individuals (those whose gender identity/expression differs from their birth-assigned sex/gender). According to this model, the cumulative stress caused by stigma and social marginalization fosters stress-related health problems. Yet studies linking minority stress to physical health outcomes have yielded mixed results, suggesting that something is missing from our understanding of stigma and health. Social safety may be the missing piece. Social safety refers to reliable social connection, inclusion, and protection, which are core human needs that are imperilled by stigma.
The absence of social safety is just as health-consequential for stigmatized individuals as the presence of minority stress, because the chronic threat-vigilance fostered by insufficient safety has negative long-term effects on cognitive, emotional, and immunological functioning, even when exposure to minority stress is low. We argue that insufficient social safety is a primary cause of stigma-related health disparities and a key target for intervention.
Minority stress is defined as the chronic, cumulative stress associated with stigma, due to objective events (such as discrimination and victimization) and psychological responses to these events (such as internalized shame). According to minority stress theory, repeated exposure to such experiences overtaxes individuals’ stress response systems, heightening their vulnerability to stress-related health problems over the life course.
Our discussion focuses on sexual and gender stigma, but a social safety perspective also broadens our understanding of the health effects of other forms of marginalization, such as race, ethnicity, age, socioeconomic status, religion, citizenship, neurodiversity, physical ability, etc. Whenever individuals are considered lesser by others, their lives are fundamentally devalued, making them more vulnerable to harm and less likely to receive assistance from others.
From: Management of a concealable stigmatized identity: A qualitative study of concealment, disclosure and role flexing among young, resilient sexual and gender minority individuals. Bry L et al. [2017] Journal of Homosexuality.
Disclosure of a sexual or gender minority status has been associated with both positive and negative effects on wellbeing. Few studies have explored the disclosure and concealment process in young people. Interviews were conducted with 10 sexual and/or gender minority individuals, aged 18–22 years, of male birth sex. Data were analyzed qualitatively, yielding determinants and effects of disclosure and concealment. Determinants of disclosure included holding positive attitudes about one’s identity and an implicit devaluation of acceptance by society. Coming out was shown to have both positive and negative effects on communication and social support, and was associated with both increases and decreases in experiences of stigma. Determinants of concealment included lack of comfort with one’s identity and various motivations to avoid discrimination. Concealment was also related to hypervigilance and unique strategies of accessing social support. Results are discussed in light of their clinical implications.
Public identification with a stigmatized identity can result in acts of discrimination or rejection. Conversely, refraining from public association with a stigmatized identity that is relatively concealable can provide opportunities to circumvent discriminatory experiences. Thus, individuals who relate to concealable stigmatized identities (e.g., HIV positive serostatus, sexual minority status, mental health disorder, infertility status or previous abortion, Irritable Bowel Diseases or other stigmatized chronic health conditions, low-income level, gender identity [one’s subjective and potentially concealable sense of one’s gender] that falls outside societal conventions given one’s biological sex) may continually undergo complex decision making to manage the information they choose to present to their social environment.
With regard to potential health benefits, coming out has been associated with positive outcomes, including higher self-esteem. Self-disclosure has also been associated with fewer mental health problems, including emotional distress and conduct problems. For individuals whose families react to their disclosure with acceptance, disclosure is associated with better social support systems and health, and fewer symptoms of depression, substance abuse, and suicidality. When adolescents or young adults begin to express a public sexual or gender minority identity, their behaviours may fall more in line with their internal beliefs and attitudes, thus decreasing cognitive dissonance they may have experienced previous to disclosure. Individuals who are “out” may also be more likely to participate in the LGBT community, which can help them to cultivate a unique and important source of social support.
However, keeping a key aspect of one’s identity concealed over time can have deleterious effects on well-being. Adolescence is a period when individuals gain a better understanding of their multiple identities and begin incorporating these identities into a cohesive whole. However, coming of age in a heterosexist society can indoctrinate individuals from a young age to these stigmatizing attitudes, and thus deems it necessary to disentangle such attitudes from personal characteristics and experiences. Indeed, for individuals whose sexual identity deviates from the heterosexual norm, integrating a stigmatized identity into the whole self can be met with fear and shame. During this time, to avoid social alienation, young people may portray a sexual identity that lays more in line with societal norms, but contradicts their internal attitudes and desires. This may lead to cognitive dissonance, avoiding contact with same-sex friends, and enacting sexual stigma toward others. Over time, chronic concealment of a sexual or gender minority status may lead to social isolation and a denial of one’s sexual identity, both of which have negative effects on mental health.
This investigation fills an important gap in the literature. Previous research on the subject of disclosure focuses largely on adult samples, and as a result, those findings may not generalize to young people. Further, qualitative studies among young people did not characterize their samples in terms of mental health, and thus it is more difficult to gauge the extent to which the strategies described are adaptive.
The clinical implications of these findings are broad. Young LGBT individuals show increased rates of mental health difficulties compared to their heterosexual and cisgender counterparts. There is a call for a greater number of culturally sensitive mental health providers to treat the specific needs of LGBT people, and understanding the complex processes behind identity management is crucial to providing culturally relevant support to young people in the midst of these deliberations. Disclosure is associated with both positive and negative outcomes.
Identity management represents a dynamic process that requires new evaluations upon each unique social environment.
From: Identity concealment in transgender adults: A qualitative assessment of minority stress and gender affirmation. Rood B. et al. [2017] American Journal of Orthopsychiatry.
Minority individuals might conceal their identity in social contexts in an effort to avoid stigma and victimization. Unfortunately, identity concealment is thought to impact psychological distress in transgender and gender nonconforming (TGNC) individuals. Thus, through 30 in-depth interviews, we sought to understand if and how identity concealment was experienced by TGNC individuals. Findings indicated that
(a) TGNC identity concealment is a source of stress,
(b) individuals might conceal their TGNC identity based on social context,
(c) concealment of assigned sex and gender history can function to affirm one’s true gender identity, and
(d) concealment of gender history is a rejection of one’s assigned sex.
In addition:
(a) passing/blending is an important interpersonal and intrapersonal process,
(b) the importance of passing/blending can change over time, and
(c) not passing/blending may result in worrying about personal safety.
From: The significance of structural stigma towards transgender people in health care encounters across Europe: Health care access, gender identity disclosure, and discrimination in health care as a function of national legislation and public attitudes. Falck F and Branstrom R. [2023] BMC Public Health.
According to the minority stress theory, stigma affects the health of marginalized populations. Previous stigma research has focused on the health effects of individual and interpersonal stigma, paying less attention to structural factors. Laws on legal gender recognition affect the lives of transgender individuals in unique ways. The fact that these laws and population attitudes vary greatly between European countries, offer a unique opportunity to study the role of structural stigma in the lives of transgender individuals. Little is known about how transgender specific structural stigma relates to individual health determinants. Consequently, the aim of this study was to explore the association between structural stigma and access to gender affirming care, gender identity disclosure in health care, and experiences of discrimination in health care across 28 European countries.
Country-level structural stigma was negatively associated experiences of seeking gender affirming care and positively associated with concealment of being transgender to health care providers. Identity concealment was associated with a lower likelihood of exposure to discrimination in the health care setting across countries regardless of their level of structural stigma. The most prevalent reasons to forgo gender affirming care were shared between low and high structural stigma country groups and cantered around fear.
The results highlight the importance of changing stigmatizing legislation and population attitudes to promote access to gender affirming care as well as openness of being transgender towards providers. Measures to decrease discrimination in the health care setting are warranted in high as well as in low structural stigma countries.
Stigma is the result of a process whereby certain groups of people are identified and labelled as different, assigned stereotypical traits, and associated with undesirable characteristics. By creating a distinction between us and them, those who are seen as different are devalued, rejected, excluded, and labelled as deviants, resulting in a loss of status, social, cultural, financial, and political power.
Stigma operates at structural, interpersonal and individual levels, as well as across these levels. Individual level stigma involves cognitive, affective, and behavioural responses to discrimination and devaluation, and includes the perceptions that individuals have about themselves as well as their notions of what other people think and feel about them. Interpersonal stigma focuses on interactions between people involving exposure to verbal harassment, physical and sexual violence, unintentional demeaning comments, and a lack of family support. Structural stigma is the most distal form of stigma. It encompasses societal norms, laws, and policies, which restrict the opportunities and resources of stigmatized groups or fail to protect their equal rights.
Across countries and regardless of the level of structural stigma, individuals who concealed their gender identity from health care providers were considerably less likely to report discrimination in health care as compared to those who were open about being transgender (p < .001). Among those who concealed their transgender status to their health provider, 68.5% reported that they had not encountered any of the types of discrimination in health care that was outlined in the survey. When looking at those who were open with their transgender identity, the prevalence of transgender-related discrimination in health care almost doubled.
By combining an unusually large data set on gender identity disclosure, health seeking behaviours, and experiences of discrimination in the health setting among transgender individuals living in 28 countries across Europe with an objective stigma index based on national laws and attitudes, we find evidence that structural stigma predicts whether a transgender individual will come out to their health provider as transgender and seek gender affirming care. The higher the level of structural stigma is in a country, the less likely transgender individuals are to disclose to their healthcare provider that they are transgender and to seek gender affirming care. These findings highlight the important role that general attitudes and laws pertaining to transgender individuals play in shaping individual health outcomes, linking structural and individual stigma levels.
Interventions to decrease stigma towards transgender individuals who come out to their health care provider are warranted in high- as well as lower-structural-stigma settings. Since transgender people face specific structural challenges, such as barriers to legal gender recognition and gender affirming care that meet their needs, it is essential to continue to explore how this affects their health as well as health-related needs.
Key Literature References
*** The Challenge of Living in a Body One Doesn’t Identify With: Accounts From Transgender Individuals (2025), by Maria Rita Lerri, et al., published in the Journal of Pediatric Healthcare
(Notable) *** Shortcomings of Transgender Identity Concealment Research: A Scoping Review of Associations with Mental Health (2025), by Lily Osmetti, et al., published in the International Journal of Transgender Health
(Notable) *** Children’s attitudes about transgender identity disclosure and concealment (2025), by Daniel J. Alonso, et al., published in the British Journal of Developmental Psychology
*** Lesbian, Gay, Bisexual, Transgender and Queer People’s Experiences of Stigma Across the Spectrum of Inpatient Psychiatric Care: A Systematic Review (2025), by Kristen D. Clark, et al., published in International Journal of Mental Health Nursing
*** Beyond the Centrality of Shame: How Self-Concealment and Fear of Receiving Compassion From Others Impact Psychological Suffering in Transgender Adults (2024), by Sérgio A. Carvalho, et al., published in the Journal of Homosexuality
*** Structural stigma, gender-affirming interventions, and identity concealment as determinants of depression and life satisfaction among trans adults in 28 European countries (2024), by Berk C. Ünsal, et al., published in the International Journal of Transgender Health
(Notable) *** “I Have Kept it a Secret My Whole Life”: Sexual and Gender Minority Identity Concealment, Secret Keeping, and Minority Stress (2024), by Marc Troy Dennis, unpublished Master’s thesis, Carleton University
(Notable) *** Age of Realization and Disclosure of Gender Identity Among Transgender Adults (2023), by Jack L. Turban, et al., published in the Journal of Adolescent Health
*** The significance of structural stigma towards transgender people in health care encounters across Europe: Health care access, gender identity disclosure, and discrimination in health care as a function of national legislation and public attitudes (2023), by Felicitas Falck, published in BMC Public Health
(Notable) *** Rethinking minority stress: A social safety perspective on the health effects of stigma in sexually-diverse and gender-diverse populations (2022), by Lisa M. Diamond & Jenna Alley, published in Neuroscience & Biobehavioral Reviews
*** Inconcealable: A Cognitive–behavioral Model of Concealment of Gender and Sexual Identity and Associations with Physical and Mental Health (2021), by James M. Brennan, et al., published in Psychology of Sexual Orientation and Gender Diversity
*** Internalized Transphobia, Nondisclosure of Gender Identity, and Life Satisfaction among Transgender and non-binary Adults: The Moderating Roles of Psychological Flexibility and Inflexibility (2021), by Maureen K. Flynn & Yash Bhambhani, published in the Journal of Contextual Behavioral Science
*** Real-time Associations Between Discrimination and Anxious and Depressed Mood Among Sexual and Gender Minorities: The Moderating Effects of Lifetime Victimization and Identity Concealment (2020), by Nicholas A. Livingston, et. al, published in the journal Psychology of Sexual Orientation and Gender Diversity
(Notable) *** Management of a concealable stigmatized identity: A qualitative study of concealment, disclosure and role flexing among young, resilient sexual and gender minority individuals (2017), by Laura Jane Bry, et al., published in the Journal of Homosexuality
*** Identity Concealment in Transgender Adults: A Qualitative Assessment of Minority Stress and Gender Affirmation (2017), by Brian A. Rood, et al., published in the American Journal of Orthopsychiatry
*** The Disclosure Experiences of Male-to-Female Transgender Individuals: A Systems Theory Perspective (2013), by Maureen S. Bethea, published in the Journal of Couple and Relationship Therapy
>> (Chapter 15) What research has investigated suicide risk among gender-diverse individuals (adults and youths)?
Overview, by Laura Henton, DNP, APRN, FNP-C
Suicide is an urgent and growing public health crisis. According to the Centers for Disease Control and Prevention (CDC, 2025), it is the leading cause of death in the United States, responsible for over 49,000 deaths in 2023. The discrimination and emotional distress faced by transgender and gender diverse individuals is seen as a key risk factor of suicidality. The highest rate of suicide attempts of any marginalized group is the transgender and gender diverse: 40 percent of transgender individuals have attempted suicide at least once (Dickey & Budge, 2020). This section will address a variety of the research that has been investigated on this topic.
Polidori and colleagues (2023) were interested in the connection between co-occurring gender diversity and neurodiversity, especially as they pertained to suicide attempt rates. They carried out systematic reviews of research literature and found that suicide attempt rate was 20 percent higher in gender diverse individuals than the general public (the control group), and slightly higher (31 percent) among female-to-male transgender individuals than male-to-female (29 percent) individuals.
Research by Mak and colleagues (2020) looked at data from the electronic medical records of 6327 transgender and gender diverse individuals served by the Kaiser health plans of California and Georgia. They found that those most at risk were those with prior suicidal ideation or attempts, those with multiple mental health diagnoses, and younger individuals. Although attempt rates were somewhat higher for transmasculine than for transfeminine individuals, the lifetime prevalence for suicide attempt was found to be 32-41 percent for transgender and gender diverse individuals versus 2-8 percent for the general population. Additional risk factors include unemployment, lower income, and experiences of violence.
Researchers Pellicane and Ciesla (2021) examined 85 quantitative studies, interested in depression and suicidality due to internal and external stressors related to transgender and gender diverse identity. These researchers identified that external stressors, expectations of rejection, internalized transphobia, and concealment were associated with increased depression and suicidal ideation/suicide attempt. Examples of relevant external stressors are cited as non-affirmation from healthcare providers and denial of gender-affirming care by insurers.
Researchers Kaniuka and colleagues (2024) queried 30 transgender/gender diverse adults with a history of suicidal ideation and/or suicide attempt, interested in what contributes to (or thwarts) suicidal ideation, and what contributes to the progression from suicidal ideation to attempt. They found that the progression from suicidal ideation to suicide attempt was halted by accessing mental health services, emotional regulation, connecting with others, and identifying reasons for living.
Interested in suicidal ideation and internal and external minority stressors, researchers Testa and colleagues (2017) surveyed 816 transgender and gender diverse individuals, who were predominantly young (aged 18-30, 58 percent) white (86 percent) adults. Thirty percent of those surveyed were transfeminine; 46 percent were transmasculine. These researchers found that victimization was associated with negative expectations, and internalized transphobia and negative expectations were associated with suicidal ideation.
Transphobic laws and policies were the focus of research by Price et al. (2024), who surveyed 27,279 transgender adults across the United States. These researchers found that transgender individuals living in states with higher levels of transphobia had higher levels of suicidal ideation and suicide attempts. Those states with the highest state-level transphobia are the southern states of Alabama, Mississippi, Arkansas, Louisianna, Georgia, and Oklahoma, as well as Idaho and Kentucky.
Researchers Boase and McLaren (2023), interested in self-compassion and self-coldness, surveyed 385 transgender and gender diverse adults. Variables studied were self-compassion, self-coldness, discrimination, and suicide risk; findings included higher self-compassion associated with lower suicide risk.
Battalen and colleagues (2021) examined the constellation of discrimination, suicidal thoughts, suicide attempts, and depressive symptoms in 94 adolescents who were already affiliated with a transgender youth clinic. The majority of the respondents reported being discriminated against (94 percent) and victimized (64 percent), and nearly half (49 percent) stated that they had had at least one suicide attempt.
Bluth and colleagues (2024) led an eight-session online self-compassion program for 35 transgender adolescents. Well-being improved, and suicidal ideation decreased. Researchers Bosse and colleagues (2024), knowing the connection between parental rejection and worsening mental health among transgender adolescents, studied sibling acceptance and rejection. High rejection from a male parent or both parents was associated with worse depression and suicidality; “sibling high rejection was not significant when considered with high rejection from parents” (Bosse et al., 2024, p. 97).
Researchers Allen et al. (2019) studied 47 adolescents who had been given gender-affirming hormones. They found that the participants’ well-being scores significantly increased, and suicidality decreased, three months post-treatment. Causation cannot be implied as there was no control group.
This is not a public health crisis limited to the United States. North of us, Eccles et al. (2024) surveyed 9861 Canadians and found that substance use disorders and suicidal ideation were significantly higher in transgender and gender diverse (TGD) individuals (25 percent) than the cisgender participants (3 percent). Kingsbury and colleagues (2022) surveyed 6800 Canadian adolescents aged 15-17, 1440 of whom identified as other than heterosexual. These researchers found that adolescents who identify as transgender or gender-nonconforming are at higher risk of suicidal ideation and suicide attempt. More than 3000 transgender and gender diverse adolescents (n=3713) living in the United Kingdom were surveyed on their school experiences and suicidal ideation/suicide attempts (Jadva et al., 2021). It was found that trans adolescents were twice as likely [as their cisgendered peers] to report attempted suicide and three times as likely to report suicidal ideation.
Adams et al. (2017) conducted a meta-synthesis of 42 studies which focused on transgender suicidality. They determined that the average rate of suicidality in the transgender population in the United States and Canada was 14 to 22 times that of the general public, and higher among transfeminine than transmasculine individuals.
Dickey and Budge (2020) write in general terms about the high rates of transgender individuals’ suicide attempt rate , and three theories that explain suicidality: interpersonal theory (due to burdensomeness and thwarted belongingness), minority stress theory (internal and external stress, and anticipation of external stress), and intersectionality (how race, gender, and class interact). They identify resilience and social supports as protective factors.
References
Adams, N., Hitomi, M., & Moody, C. (2017). Varied reports of adult transgender suicidality: Synthesizing and describing the peer-reviewed and gray literature. Transgender Health, 2(1), 60-75. https://doi.org/10.1089/trgh.2016.0036
Allen, L. R., Watson, L. B., Egan, A. M., & Moser, C. N. (2019). Well-being and suicidality among transgender youth after gender-affirming hormones. Clinical Practice in Pediatric Psychology, 7(3). https://doi.org/10.1037/cpp0000288
Battalen, A. W., Mereish, E., Putney, J., Sellers, C. M., Gushwa, M., & McManama O’Brien, K.H. (2021). Associations of discrimination, suicide ideation severity and attempts, and depressive symptoms among sexual and gender minority youth. Crisis, 42(4), 301-308. https://doi.org/10.1027/0227-5910/a000718
Bluth, K., Bryce, A., Lathren, C. R., Park, J., Pflum, S., & Clayton, M. (2024). Reducing suicide ideation in transgender adolescents with mindful self-compassion: An open trial. Mindfulness, 15, 3107-3128. https://doi.org/10.1007/s12671-024-02421-7
Boase, E.-R., & McLaren, S. (2024). Discrimination and suicide risk among transgender and gender-diverse adults: The moderating roles of self-compassion, self-coldness, and gender identity. Psychology of Sexual Orientation and Gender Diversity, 11(4), 606-618. https://doi.org/10.1037/sgd0000634
Bosse, J. D., Clark, K. D., Dion, K. A., & Chiodo, L. M. (2024). Transgender and nonbinary young adults’ depression and suicidality is associated with sibling and parental acceptance-rejection. Journal of Nursing Scholarship, 56(1), 87-102. https://doi.org/10.1111/jnu.12917
Burnside, A., Lorenz, D., Harries, M., Janssen, A., & Hoffman, J. (2025). Suicide risk identified among transgender and gender diverse youth in the emergency department (2019–2022). Academic Pediatrics, 25(2), 102574.
Dickey, L. M. & Budge, S. L. (2020). Suicide and the transgender experience: A public health crisis. American Psychologist, 75(3), 380-390. https://doi.org/10.1037/amp0000619
Eccles, H., Abramovich, A., Patte, K. A., Elton-Marshall, T., Racine, N., Ferro, M. A., Edwards, J., Anderson, K. K., Afifi, T. O., Geoffroy, M. C., Kingsbury, M., & Colman, I. (2024). Mental disorders and suicidality in transgender and gender-diverse people. JAMA Network Open, 7(10), e2436883. https://doi.org/10.1001/jamanetworkopen.2024.36883
Jadva, V., Guasp, A., Bradlow, J. H., Bower-Brown, S., & Foley, S. (2023). Predictors of self-harm and suicide in LGBT youth: The role of gender, socio-economic status, bullying and school experience. Journal of Public Health, 45(1), 102-108. https://doi.org/10.1093/pubmed/fdab383
Kaniuka, A. R, Nanney, E. M., Robertson, R., Hoff, R., Smith, M., Bowling, J., Basinger, E. D., Dahl, A. A., & Cramer, R. J. (2024). A grounded theory of sexual and gender minority suicide risk: The sexual and gender minority suicide risk and protection model. Psychology of Sexual Orientation and Gender Diversity. https://doi.org/10.1037/sgd0000699
Kingsbury,. M., Hammond, N. G., Johnstone, F., & Colman, I. (2022). Suicidality among sexual minority and transgender adolescents: A nationally representative population-based study of youth in Canada. Canadian Medical Association Journal, 194(22), E767-E774. https://doi.org/10.1503/cmaj.212054
Mak, J., Shires, D. A., Zhang, Q., Prieto, L. R., Ahmedani, B. K., Kattari, L., Becerra-Culqui, T. A., Bradlyn, A., Flanders, W. D., Getahun, D., Giammattei, S. V., Hunkeler, E. M., Lash, T. L., Nash, R., Quinn, V. P., Robinson, B., Roblin, D., Silverberg, M. J., Slovis, J., Tangpricha, V., … Goodman, M. (2020). Suicide attempts among a cohort of transgender and gender diverse people. American Journal of Preventive Medicine, 59(4), 570-577. https://doi.org/10.1016/j.amepre.2020.03.026
Pellicane, M. J. & Ciesla, J. A. (2021). Associations between minority stress, depression, and suicidal ideation and attempts in transgender and gender diverse (TGD) individuals: Systematic review and meta-analysis. Clinical Psychology Review, 91, 102113. https://doi.org/10.1016/j.cpr.2021.102113
Polidori, L., Sarli, G., Berardelli, I., Pompili, M., & Baldessarini, R. J. (2024). Risk of suicide attempt with gender diversity and neurodiversity. Psychiatry Research, 333, 115632. https://doi.org/10.1016/j.psychres.2023.115632
Price, M. A., Hollinsaid, N. L., McKetta, S., Mellen, E. J., & Rakhilin, M. (2024). Structural transphobia is associated with psychological distress and suicidality in a large national sample of transgender adults. Social Psychiatry and Psychiatric Epidemiology, 59(2), 285-294. https://doi.org/10.1007/s00127-023-02482-4
Testa, R. J., Michaels, M. S., Bliss, W., Rogers, M. L., Balsam, K. F., & Joiner, T. (2017). Suicidal ideation in transgender people: Gender minority stress and interpersonal theory factors. Journal of Abnormal Psychology, 126(1), 125-136. https://doi.org/10.1037/abn0000234
U.S. Centers for Disease Control and Prevention (CDC) (2025). About suicide prevention. https://www.cdc.gov/suicide/about/index.html
Key Literature References
*** All-cause and suicide mortalities among adolescents and young adults who contacted specialised gender identity services in Finland in 1996–2019: a register study (2025), by Sami-Matti Ruuska, et al., published in BMJ Mental Health
(Notable) *** Mental Disorders and Suicidality in Transgender and Gender-Diverse People (2024), by Heidi Eccles, et al., published in JAMA Network Open
*** Structural transphobia is associated with psychological distress and suicidality in a large national sample of transgender adults (2023), by Maggi A. Price, et al., published in the journal Social Psychiatry and Psychiatric Epidemiology
*** Discrimination and suicide risk among transgender and gender-diverse adults: The moderating roles of self-compassion, self-coldness, and gender identity (2024), by Ella-Rose Boase, published in the journal Psychology of Sexual Orientation and Gender Diversity
*** A grounded theory of sexual and gender minority suicide risk: The sexual and gender minority suicide risk and protection model (2024), by Andrea Kanaiuka, et al., published in the journal Psychology of Sexual Orientation and Gender Diversity
*** Transgender and nonbinary young adults’ depression and suicidality is associated with sibling and parental acceptance-rejection (2024), by Jordon D. Bosse, et al., published in the Journal of Nursing Scholarship
*** Reducing Suicide Ideation in Transgender Adolescents with Mindful Self-Compassion: An Open Trial (2024), by Karen Bluth, et al., published in the journal Mindfulness
(Notable) *** Predictors of self-harm and suicide in LGBT youth: The role of gender, socio-economic status, bullying and school experience (2023), by V Jadva, et al., published in Journal of Public Health
(Notable) *** Associations between Minority Stress, Depression, and Suicidal Ideation and Attempts in Transgender and Gender Diverse (TGD) Individuals: Systematic Review and Meta-Analysis (2022), by Michael J. Pellicane & Jeffrey A. Ciesla, published in the journal Clinical Psychology Review
(Notable) *** Suicidality among sexual minority and transgender adolescents: a nationally representative population-based study of youth in Canada (2022), by Mila Kingsbury, et al., published in Canadian Medical Association Journal
*** Associations of Discrimination, Suicide Ideation Severity and Attempts, and Depressive Symptoms Among Sexual and Gender Minority Youth (2021), by Adeline Wayman Battalen, et. al, published in the journal Crisis: The Journal of Crisis Intervention and Suicide Prevention
*** Suicide and the Transgender Experience: A Public Health Crisis (2020), by Lore M. Dickey & Stephanie L. Budge, published in the journal American Psychologist
(Notable) *** Well-being and Suicidality among Transgender Youth after Gender-Affirming Hormones (2019), by Luke R. Allen, et. al, published in the journal Clinical Practice in Pediatric Psychology
*** Varied Reports of Adult Transgender Suicidality: Synthesizing and Describing the Peer-Reviewed and Gray Literature (2017), by Noah Adams, et. al, published in the journal Transgender Health
(Notable) *** Suicidal ideation in transgender people: Gender minority stress and interpersonal theory factors (2017), by Rylan Testa, et al., published in Journal of Abnormal Psychology
>> (Chapter 16) What is gender euphoria and how has it been researched?
Overview, by Scott Kerlin
What is gender euphoria?
There is a tremendously valuable and liberating body of published research with deep investigation of the concept of gender euphoria. Australian researchers Stella Kulesza, et al., 2025 state, “The term gender euphoria captures the elation caused by positive experiences of gender for trans and gender diverse people. Gender euphoria is a trans-driven concept that has long existed within trans communities. Yet as noted above, gender euphoria as a concept exists within the academic literature as a relatively under-researched experience that requires further exploration to understand its nuances and facets.”
Sari L. Reisner and colleagues (2023) recognize that transgender and gender-diverse (TGD) individuals experience mental health inequities, including high rates of psychological distress. They note that “gender euphoria is a concept often discussed in TGD communities that has only recently been considered by the research community. Although there is no agreed upon definition, gender euphoria generally refers to positive emotions, such as happiness or intense joy and feelings of calm, resulting from gender self-actualization, affirmation of gender identity or expression, and/or achievement of desired transgender milestones.”
As described by Ashley Austin & colleagues (2022), gender euphoria is a term increasingly used in transgender and gender diverse (TGD) communities. Experiences of gender euphoria are often overlooked during clinical assessment and most academic research tends to focus solely on discussions of gender dysphoria. In a study intended to investigate the occurrence of gender euphoria in individuals, descriptive and visual data was used to clarify gender euphoria as a concept as well as reveal the ways in which it is experienced among TGD adults. The primary themes emerging from the study yielded the following four key processes, which explain experiences of gender euphoria: 1. Being exposed to a gender affirming antecedent, 2. Having an affirming thought, 3. Feeling a positive emotion, and 4. Experiencing enhanced quality of life. Participants’ discussions elicited through self-selected images contribute to a more meaningful understanding of gender affirmation in the lives of TGD people.
Beischel and colleagues, 2022 observe that gender euphoria is an important experience and concept for many, especially transgender and/or nonbinary individuals, but has not received much attention from psychological and clinical research. In contrast to gender dysphoria, which originates in psychiatry, the term “gender euphoria” has been mobilized by some LGBTQ people to describe the powerfully positive emotions that can come from one’s gender/sex. In a qualitative online study of individuals of diverse sexualities and gender/sexes (including transgender, cisgender, and/or nonbinary participants), they noted the following results: “Analyses resulted in five themes: (1) gender euphoria describes a joyful feeling of rightness in one’s gender/sex, (2) gender euphoric experiences can be external, internal, and/or social, (3) “gender euphoria” originated in and circulates in online and in-person gender/sex minority communities, (4) dysphoria describes a negative feeling of conflict between gender/sexed aspects of one’s self, and (5) the relationship between euphoria and dysphoria is complex.”
What has Research on Gender Euphoria Revealed Over Time?
Leitch, et al., 2025 provide an excellent overview of the history of research on this subject. They observe, “Research on gender euphoria and positive TGNC (transgender/gender non-conforming) identity experiences has evolved, with increasing focus on understanding how joy and gender euphoria function and contribute to well-being. Studies show that gender euphoria is influenced by factors such as gender congruence, social affirmation, and community support. These are often linked to gender congruence, affirmation, and social support for TGNC people. This developing area of study has several important gaps that must be addressed. Although the term gender euphoria is the most commonly-used in current research, it should be more clearly defined, and research should distinguish between positive gender fulfillment and fleeting feelings of joy.”
Grant, et al., 2024 in a study conducted in Australia explored the association of gender euphoria with potentially better mental health outcomes for transgender adults. Among other areas of emphasis, they investigated several sociodemographic factors that were associated with having ever experienced gender euphoria. According to their findings, “compared to lesbian participants, those who identified as asexual had higher odds of ever experiencing gender euphoria. Non-binary participants had lower odds than trans men of experiencing gender euphoria. Compared to those aged 18-24 years, 35-44-year-olds had lower odds of ever experiencing gender euphoria. Participants with an undergraduate university degree had higher odds than those with a secondary school education of having experienced gender euphoria. Finally, participants living in a regional city or town had lower odds of experiencing gender euphoria than those living in an inner-suburban area”.
Further, they noted, “Taken together, these findings suggest that current experiences of gender euphoria may be related to improved mental wellbeing for trans people. Given that gender euphoria can be characterized by feelings of happiness, joy, pride, relief, comfort, and self-love, it is perhaps not surprising that such feelings may allay distress and suicidality, even if only in the short term. Conversely, those not experiencing mental ill-health may have more opportunities to experience gender euphoria.”.
How is Gender Euphoria Measured?
In 2024, Blacklock et al. set out to build “The Gender Euphoria Scale (GES)” in a “protocol paper (that) illustrates our process for developing and validating a new tool to measure gender euphoria, known as the Gender Euphoria Scale (GES), for use with trans populations.” They recognize that “while it has been suggested that gender euphoria could be the antithesis of gender dysphoria, recent studies indicate that gender euphoria is likely a construct in its own right.” In their overview, they propose “we will develop and validate a tool to measure gender euphoria for use with trans individuals. In doing so, we aim to create a tool which measures the frequency, intensity, and stability of gender euphoria, in addition to identifying experiences that contribute to gender euphoria. Moreover, we intend for this tool to be sensitive to change, relevant to people of all trans gender identities, and suitable for use in both research and clinical settings.”
Stella Kulesza, et al., 2025, through their systematic review of published gender euphoria research, note 5 themes based on articles with a targeted focus on gender euphoria: The themes of motivation for self-exploration, embodiment and affect, a sense of community, and function as a protective factor align strongly with current academic theories on gender euphoria. The use of self-exploration as a vehicle to experience euphoria follows the idea that euphoria is something that trans people seek; wanting to be happy and live as their experienced gender. The idea of euphoria as embodiment was reiterated through the participants’ visceral descriptions of euphoria as intrinsically tied to physical sensations and their bodies. A sense of community has commonly been understood as a salient aspect of transness that enhances trans joy and euphoria through support, acceptance, and pride. Further, the conceptualization of gender euphoria as a protective factor has long been theorized and was evident in the quantitative studies which predominantly focused on establishing a significant link between well-being and euphoria.”
Key Literature References
(Notable) *** Beyond dysphoria and stress: a theory of gender euphoria and gender fulfillment (2025), by Judith Leitch, Van Nguyen & Sam Potter, published in the International Journal of Transgender Health
(Notable) *** The Gender Euphoria Scale (GES): Development of a tool to measure gender euphoria (2025), by Charlotte A. Blacklock, et al., published in the International Journal of Transgender Health
(Notable) *** Exploring understandings of trans people’s experiences of gender euphoria: A systematic review and metasynthesis (2025), by Stella Kulesza, published in the International Journal of Transgender Health
*** Exploring Experiences of Gender Euphoria for Transgender and Gender Diverse Individuals (2025), by Danielle Carli Lefebvre, unpublished PhD dissertation, University of Calgary (Canada)
(Notable) *** From euphoria to wellbeing: Correlates of gender euphoria and its association with mental wellbeing among transgender adults (2024), by Ruby Grant, et al., published in the International Journal of Transgender Health
(Notable) *** Pathways to Euphoria: Deconstructing Gender-Expansive Adults Conceptualizations of Wellbeing (2024), by Taine Hall, et al., International Journal of Applied Positive Psychology
(Notable) *** The Gender Euphoria Scale (GES): a protocol for developing and validating a tool to measure gender euphoria in transgender and gender diverse individuals (2024), by C. A. Blacklock, et al., published in Frontiers in Psychology
*** “The whole world opened up, there’s no better word for it than euphoria”: Experience Of Embodiment In Trans*feminine Individuals (2024), unpublished Master’s degree thesis, Western University
*** Experiences of Gender Euphoria and Gender Contentment Among Transgender, Non-Binary, and Gender Diverse Adults (2024), by Sam Potter, unpublished Master’s in Social Work thesis, California State University, Sacramento
(Notable) *** Exploring gender euphoria in a sample of transgender and gender diverse patients at two U.S. urban community health centers (2023), by Sari L. Reisner, et al., published in the journal Psychiatry Research
(Notable) *** Gender euphoria: a grounded theory exploration of experiencing gender affirmation (2022), by Ashley Austin, et al., published in the journal Psychology & Sexuality
*** ‘ A Little Shiny Gender Breakthrough’: Community Understandings of Gender Euphoria (2022), by Will J. Beischel, et. al, published in the International Journal of Transgender Health
(Notable) *** Moving from Gender Dysphoria to Gender Euphoria: Trans Experiences of Positive Gender-Related Emotions (2022), by Kai Jacobsen & Aaron Devor, published in the Bulletin of Applied Transgender Studies
(Notable) *** Hair removal and psychological well-being in transfeminine adults: associations with gender dysphoria and gender euphoria (2021), by Nova J.Bradford,et al., published in the Journal of Dermatological Treatment
*** Where Do You Go When You Go Home? Narrative Studies of Gender Euphoria (2021), by Silas-Crewe-Kluge, Honors Thesis, Oberlin University
>> (Chapter 17) What research has been conducted that focuses on gender fluidity?
Overview, by Ian Cameron
From: The association between gender identity fluidity and health outcomes in transgender and gender diverse people in New Orleans and Los Angeles, USA. Ocasio M and Fernandz M. [2024] Preventative Medicine Reports.
This is an on-going area of research. National Academies of Science assert that Transgender and gender diverse people (TGD) face considerable stigmatization and marginalization that contribute to poor health. Studies have documented health inequities across mental and physical health outcomes when comparing TGD to non-TGD people. In recent years, there has been a growing recognition in research and public health practice that gender identity is not a binary construct and non-binary TGD may have unique experiences and health challenges relative to their binary TGD counterparts.
Many studies comparing binary TGD and non-binary TGD report significant differences in health outcomes, including depression, anxiety, suicidal ideation, and addictions. Furthermore, non-binary TGD patients have different gender-affirming treatment needs relative to their binary TGD counterparts and report that providers are insufficiently equipped to treat non-binary TGD patients due to unfamiliarity with identities outside the gender binary. These studies, and a vast majority of studies with TGD populations, define gender identity cross-sectionally. Though gender fluid is an identity in and of itself, this fixed approach directly counters the notion that gender identity and expression can fluctuate situationally and over time with no particular end point.
A number of qualitative studies have explored gender fluidity. In a study of 15 binary and non-binary TGD adults, participants described gender identity selection more commonly as an iterative, rather than linear process as they navigated identity formation. Galupo et al interviewed 197 TGD adults and fluidity emerged in interviews as both a self-ascribed identity and as a process, in which participants stated they felt “some days male, some days female” and “like a constantly flowing river.”.
More recently, researchers have also begun to examine gender identity fluidity, that is self-reported changes in gender identity, using quantitative data. A 2023 study found that in a sample of TGD adolescents (83.6 % white), 29 % changed their gender identity at least once over a 1.5-year period. A similar study in an enthoracially diverse sample of 225 adolescents and young adults (34 % non-Latinx Black, 38 % Latinx), 77 % changed their identity at least once during the two-year study period, and 17 % at least twice. This may suggest that gender identity fluidity exists across ethnoracial identities and throughout the life course. Despite the preponderance of gender identity fluidity, few studies examine how this fluidity impacts physical and mental health outcomes among TGD people.
Similar to studies comparing non-binary TGD and binary TGD, the few available studies focused on gender identity fluidity and health report mixed results. For instance, a recent study using a nationally representative sample of adolescents and adults from the 2014–2018 Population Assessment of Tobacco and Health in the US reported a higher prevalence of past 30-day tobacco use among gender identity fluid participants than those who were gender identity consistent. There were no differences in tobacco use between transgender-consistent and cisgender-consistent participants. On the other hand, a study of a community sample of 78 TGD young people ages 15–21 years old reported no significant difference in depressive symptoms between gender identity fluid and gender identity consistent participants. Elucidating the impact that gender identity fluidity may have on health and mental health outcomes, particularly during the critically important developmental period of adolescence and young adulthood, merits further investigation.
From: Gender Fluidity: Consequences for Youth’s mental health and important protective factors. Mavrova G [2024] Development and Adolescent Heath.
The aim of this review is to delineate and analyse the acceptance of gender fluidity which refers to an individual’s gender identity being flexible and not confined to traditional binary gender categories of male and female. Important differences in various terms that may or may not fall under the term gender fluidity such as ‘Genderqueer’ and ‘Non-binary’ etc. will be discussed.
After presenting the definition, the important differences and the historical background of the concept, data from various studies will follow. The survey data are mainly from the USA, Canada and Greece and cover the period 2009 to 2023. Very often the exact words of people with gender non-conforming are quoted.
Evidence was recorded on the mental health consequences for gender fluid young people due to non-acceptance by family, school and friends. Negative mental health consequences for young people lead to a model of minority anxiety about the health of sexual minorities. Instead, attempts of acceptance by the family and school lead to a supportive framework. For example, the Genders & Sexualities Alliances (GSA program operating in Canada will be mentioned and its results will be presented. Finally, there is a reference to the international legislation and that of Greece in particular, and the governmental treatment of gender fluid people.
The negative consequences on mental health as a consequence of the non-acceptance of gender fluidity make evident the need for direct intervention and recognition of young people who want to express themselves in this way.
From: “Like a Constantly Flowing River”: Gender Identity Flexibility Among Nonbinary Transgender Individuals. Galupo M. Pulice-Farrow L and Ramirez J. [2017] Identity Flexibility During Adulthood.
Gender is one of the first identities we learn and binary distinctions based on gender (e.g. girl/boy, woman/man, cisgender/transgender) are pervasive. The conceptualization of gender identity among transgender individuals is uniquely complicated by dichotomous notions of gender/sex. This is particularly true for individuals in the transgender community who are gender non-conforming or experience their gender outside the binary. The present research investigates the conceptualization of gender identity among non-binary transgender individuals by exploring the gender identity labels they choose and the descriptions they provide for their gender identity and experience.
Participants included 197 adults recruited from a larger study on transgender experience who completed an online study. Participants ranged in age between 18-70 and self-identified as gender variant (n = 129) or agender (n = 68). Qualitative responses were analysed via thematic analysis. Six themes were identified as related to the way gender non-conforming individuals describe their gender identity:
1) Gender Identity Using Binary Terms of Gender/Sex;
2) Gender Identity as Blended;
3) Gender Identity as Fluid;
4) Gender Identity as Non-Binary;
5) Transgender as Gender Identity; and
6) Agender Conceptualizations. Discussion focuses on the ways that gender non-conforming individuals’ experience of gender identity may contribute to the way we conceptualize identity flexibility.
From: Sexual Fluidity: Implications for Population Research. Mittleman J {2023] Demography.
For the first time ever, national censuses have begun asking adults to report their sexual orientations. However, because such surveys provide only cross-sectional snapshots of populations, these data obscure one key complexity: that sexuality can be fluid, with sexual self-identification evolving over time. Drawing on unique, restricted-use data from the Population Assessment of Tobacco and Health, the current study documents the prevalence, correlates, and empirical consequences of sexual fluidity in the contemporary United States. Overall, about 1 in 11 American adults changed sexual identities over five annual surveys, including 6% of cisgender men, 11% of cisgender women, and 35% of gender minorities. Fluidity was particularly pronounced among young adults and among those who had ever identified as bisexual or “something else.” Despite the frequency and patterning of sexual fluidity, accounting for fluidity did little to change observed patterns of disadvantage on three measures of sexual minority well-being: mental health, financial insecurity, and substance use. Given these facts, I argue that demographic research should foreground the complexities inherent in quantifying sexuality, focusing less on how many people “are” a given sexual orientation and more on the social dynamics that continue to produce sexual minority disadvantage.
After long rendering sexual minority populations invisible, major demographic surveys are increasingly inviting adults to report their sexual orientations. For the first time ever, the 2021 Census of England and Wales included a voluntary question asking all adults, “Which of the following best describes your sexual orientation? Straight or Heterosexual; Gay or Lesbian; Bisexual; Other sexual orientation” (Office for National Statistics. The 2023 New Zealand Census included a nearly identical question In the United States, the Census Bureau included a similar measure in its Household Pulse Survey, a first step in the Biden administration’s plan to expand the collection of sexual orientation data. As of 2019, a total of 15 OECD countries had assessed sexual orientation in at least one nationally representative survey.
Given the historic erasure of sexual minority lives in demographic data, the inclusion of sexual identity items in population-representative surveys is a vitally important development. And yet, cross-sectional data like these are only able to capture individuals’ sexual identification at a single point. As a result, these data freeze in time what many people experience as a much more dynamic and ongoing process. To produce stable estimates of how many people “are” a given sexual identity, demographers must sidestep this issue, implicitly assuming a fixed, static conception of sexuality.
Taken together, existing research affirms the importance of sexual fluidity but provides only fragmented evidence regarding its prevalence and implications for ongoing population research.
Across the English-speaking world and beyond, efforts are underway to add measures of sexual orientation into national censuses and other major demographic surveys. The data produced by these efforts will present historic opportunities to generate knowledge and shape policy. Yet these data will also be limited in one important regard: by only capturing individuals at a single point in time, these data will obscure the impact of sexual fluidity in many people’s lives.
To understand the implications of sexual fluidity for ongoing population research, the current study drew on the Population Assessment of Tobacco and Health—a large, nationally representative cohort study of American adults. Analyzing five waves of survey data, I find that 8.7% of adults—about 1 in 11—changed sexual identities at least once between 2013 and 2019. Although all groups reported some degree of sexual fluidity, fluidity was especially common among gender minorities and among young cisgender women aged 18–24 at baseline. Roughly 1 in 3 gender minorities and 1 in 5 young cisgender women changed sexual identities at least once. An even greater proportion of respondents reported changes in sexual attractions, with attraction changes reported by 24% of all respondents, 46% of young cisgender women, and 52% of gender minorities. Because the PATH data cover only five years and begin at age 18, all of these estimates are surely lower bounds on the full extent of sexual fluidity that individuals experience over the course of their lives.
In January 2023, the British government released a report summarizing the first national census to ever ask all adults about their sexual orientation (Office of National Statistics 2023). At this historic juncture, the current study reminds demographers of a fact that has been apparent since the establishment of modern sex research: human sexuality is more complex than the categories we create to contain it. As Kinsey et al. (1948:639) famously concluded: “the world is not to be divided into sheep and goats . . . only the human mind invents categories and tries to force facts into separated pigeon-holes.” Although dividing individuals into quantifiable categories lies at the heart of demographic research, the current study reminds researchers that the boundaries between these categories are much more fluid than our data might suggest.
From: Fluidity in Gender Identity and Sexual Orientation Identity in Transgender and Nonbinary Youth. Katz-Wise S [2023] The Journal Of Sex Research.
Changes in sexual orientation identity (SOI) and gender identity (GI) have rarely been studied in transgender and/or nonbinary youth (TNBY), but documenting such changes is important for understanding identity development and gender transition and supporting the needs of TNBY.
This study examined the frequency and patterning of changes in GI and SOI across 3 months (T1-T2) and 1.5 years (T1-T4) among 183 TNBY (baseline age 14–17 years; 83.6% White, 16.9% Hispanic/Latinx) who participated in a longitudinal US study. Participants completed online surveys including measures of GI and SOI. The most common gender identity selected at T1 (with or without another gender identity) was nonbinary (56.3%), and more than half (57.4%) of youth identified with a plurisexual identity (e.g., bisexual, pansexual). GI fluidity from T1-T2 was 13.2% and from T1-T4 was 28.9%.
It was equally common to move toward a nonbinary gender identity as toward a binary gender identity. SOI fluidity was more common (30.6% from T1-T2; 55.8% from T1-T4) than GI fluidity. Shifts toward plurisexual identities were more common than shifts toward monosexual identities (e.g., straight, gay). Findings highlight the need to assess changes in GI and SOI in research and clinical practice to address the unique needs of TNBY accurately and effectively.
From: Fixed or Fluid? Sexual Identity Fluidity in a Large National Panel Study of New Zealand Adults. Lilly K et al [2023] The Journal Of Sex Research
Sexual orientation has been defined as an enduring aspect of the self, but emerging evidence reveals that people’s sexual attractions, behaviours, and identities can shift over time. To examine this possibility, we present a large longitudinal analysis of sexual orientation identity fluidity among New Zealand adults (Ntotal = 45,856; age = 18–99; lesbian, gay, bisexual, and other sexual minority (LGB+) ns = 746–3,387). Over seven years, 5.7% of participants changed sexual identities at least once.
Change was bi-directional (i.e. toward and away from LGB+ identities) and most common in people who initially reported a plurisexual identity. Although women reported higher rates of plurisexuality than men, they were not more fluid in their identities, contradicting the notion of male fixedness and female plasticity in sexuality. Moreover, openness to experience was associated with increased odds of changing from a heterosexual to a plurisexual identity, while political liberalism and lower conscientiousness were associated with increased odds of changing from a heterosexual to a plurisexual identity and more identity changes over time. Overall, our study shows that sexual identity can be fluid into adulthood and has implications for how we understand contemporary human sexuality.
Sexual orientation is popularly defined as an enduring aspect of one’s self based on a pattern of attraction to men, women, or people regardless of gender (American Psychological Association. Indeed, the “master narrative” of sexual orientation posits static categories of sexual orientation that develop early and remain stable over time. However, a growing body of literature reveals that sexual behaviour, attractions, and identity do change over time; Katz-Wise & Todd. Rather than categorizing sexual orientation as static categories, this alternative model of sexual fluidity argues that these dimensions can change in response to situational, interpersonal, and societal factors; Diamond et al. Since Diamond’s seminal work, sexual fluidity research has exponentially increased, with research across multiple populations and dimensions of fluidity (Katz-Wise & Todd].
More broadly, examining sexual fluidity allows those who identify outside of more restrictive “categories” of sexuality to be counted in sexuality research. Indeed, the construction of sexual identity as static, discrete categories has led to the erasure of many lesbian, gay, bisexual, and other non-heterosexual (hereafter LGB+) people (among others) in national studies and censuses. However, just how fluid (or enduring) sexual identity is in adulthood remains in question. One reason for this is pragmatic; sexual fluidity is best investigated longitudinally to allow for observation of stability or fluidity over weeks, months, or, ideally, when it comes to identity, years.
Another reason is sociopolitical; until recently, there were very few places where LGB+ people had adequate legal and social protections to report their sexual orientation openly and freely over time. Indeed, same-gender sexual behaviour remains illegal across much of the world, and in nations that have decriminalized LGB+ orientations, other barriers to true social equality remain.
A popular theory of sexual fluidity proposes a linear pathway: people begin heterosexual and then either remain so (i.e., are stable) or travel (i.e., are fluid) unidirectionally to either an LGB+ identity or through a bisexual identity to a gay/lesbian identity. Linear theorists argue that, in a world where heterosexuality is portrayed as the only acceptable outlet for sexual expression, sexual identity formation must start with some form of incongruence with heterosexuality and “end” with congruent identity formation.
In addition to age and gender effects, we examined the associations personality, health, and political ideology had with the magnitude of sexual fluidity (number of changes over a seven-year period; negative binomial regression) as well as with movement between heterosexual and plurisexual sexual identities (but not between other sexual identities due to sample size constraints) over a one-year period (logistic regression; RQ5). The results of a negative binomial regression model assessing the full range of psychological correlates of the number of identity changes (regardless of direction) are displayed on the right side of Table 6. The effects of emotionality (p = .710) and subjective health (p = .970) were small and positive yet not significantly associated with the number of times people reported a change in their sexual identity over the seven-year period. However, psychological distress was positively associated with the number of changes (p = .005).
Our results provide data on sexual identity fluidity, in line with the preeminent work by Diamond. Overall, our work shows that sexual identity is fluid for a meaningful minority of people and challenges the notion that such change is directional or the domain of women. We also showed that change itself was predicted by demographics, political conservatism, and personality, highlighting the dynamic nature of sexual identity across adulthood. This is important, given that many national censuses are moving toward measuring sexual orientation. Yet, our results show that who is counted as part of the LGB+ community in any given snapshot will likely change over time. Thus, the present study provides the foundation for future investigations into the expanding and ever-changing ways we understand human sexualities.
Key Literature References
(Notable) *** The association between gender identity fluidity and health outcomes in transgender and gender diverse people in New Orleans and Los Angeles, USA (2024), by Manuel A. Ocasio and M. Isabel Fernández, published in Preventative Medicine Reports
*** Fixed or Fluid? Sexual Identity Fluidity in a Large National Panel Study of New Zealand Adults (2024), by Kieren J. Lilly, et al., published in The Journal of Sex Research
*** Sexual Fluidity, BDSM and Gender: An Exploratory Study on Portuguese BDSM Practitioners (2024), by Catarina Marujo, et al., published in Sexuality and Culture
(Notable) *** Gender Fluidity: Consequences for Youth’s mental health and important protective factors (2024), by Gabriela Mavrova, published in Developmental & Adolescent Health
*** Fluidity in Gender Identity and Sexual Orientation Identity in Transgender and Nonbinary Youth (2023), by Sabra L. Katz-Wise, et al., published in The Journal of Sex Research
*** Sexual Fluidity: Implications for Population Research (2023), by Joel Mittleman, published in the journal Demography
*** Genderfluid Identity: The Role of Friendships in The Experience,
Understanding, and Expression of Fluctuating Gender (2022), unpublished PhD dissertation, University of Iowa
*** Sexual Fluidity and Psychological Distress: What Happens When Young Women’s Sexual Identities Change? (2022), by Alice Campbell, et al., published in Journal of Health and Social Behavior
*** Gender Fluidity and Nonbinary Gender Identities Among Children and Adolescents (2020), by Lisa M. Diamond, published in Child Development Perspectives
(Notable) *** “Like a Constantly Flowing River”: Gender Identity Flexibility Among Nonbinary Transgender Individuals (2017), by M. Paz Galupo, et al., published in the textbook Identity Flexibility During Adulthood
>> (Chapter 18) What research has been conducted that focuses on body image and medical surgery/transition for gender-diverse individuals?
Overview by Ian Cameron
From: Exploring body image among transgender and nonbinary adults: Considering positive body image and the pursuit of gender-affirming surgery. Markey C, Goodwin C and Schweitzer J. [2025]. Journal of Health Psychology.
This study explored body image among transgender and nonbinary adults, including their body appreciation, embodiment, general psychological distress, and gender identity-related pride. This study also considered participants’ pursuit of gender-affirming surgery and mental health services. This cross-sectional survey examined participants’ body image and psychological well-being and how these may differ when considering participants’ interest in gender-affirming surgeries and gender-affirming mental health services.
Transgender and nonbinary participants were similar in terms of their body image, but transgender participants had less psychological distress than nonbinary participants. Participants who had no interest in or had pursued a gender-affirming surgery were more likely to experience positive body image than those who desired but had not completed a gender-affirming surgery. Participants who had no interest in or had pursued mental health services also had more positive body images than those who desired treatment but had not pursued it.
From: Experiences of body image in the gender non-binary community: A qualitative analysis. Burstall J et l. [2024]. Body Image, Science Direct.
One aspect of non-binary people’s mental health that is likely to be affected by their gender diversity is their body image – a multidimensional construct that involves evaluative thoughts, feelings, and behaviours relating to the body. Indeed, much of the distress associated with gender dysphoria (clinically significant distress resulting from a marked incongruence between one’s gender and sex presumed at birth, is related to a dissatisfaction with primary and secondary sex characteristics. Primary sex characteristics are those present at birth, including external and internal genitalia, while secondary sex characteristics are those that appear during puberty, such as breasts for those presumed female at birth (PFAB), and facial hair for those presumed male at birth.
Gender dysphoria might impact non-binary and binary transgender individuals differently. For instance, some studies report that non-binary people report less gender dysphoria than their binary transgender counterparts, and are at higher risk of eating disorders and purging (vomiting) after eating, suggesting there may be differences in their experiences of body image. Androgynous body ideals were endorsed by participants to attain a neutral gender appearance and manage gender dysphoria, describing their gender-neutral body ideal as pre-pubescent (e.g., prior to the development of secondary sex characteristics). Furthermore, participants described feeling affirmed when their appearance challenged other’s ability to read their gender within binary constructs.
Participants’ body image was determined by the complex interaction between aesthetic, physiological, and cognitive factors, contributing to experiences consistent with gender dysphoria. Sources of body image-based gender dysphoria included physical attributes (including body size and shape), genitals, menstruation, and reproductive organs, as well as related sources of dysphoria including vocal pitch, clothing, and being misgendered. Gender dysphoria was discussed as being associated with feelings of discomfort, disconnection from one’s body, disgust, isolation, invalidation, depression, anxiety, and suicidal ideation, as well as avoidance behaviours, dissociation, disordered eating, and deliberate self-harm.
Hair was a source of gender dysphoria for many participants, expressing discomfort with facial and body hair, because they associated it with masculinity and incongruence with androgyny. The pitch of their voice as a source of significant distress for its incongruence with their internal experience of gender, and for being a reminder that their intrinsic perception of how they present in the world is not always how they are perceived by others. Clothing was a source of gender dysphoria for participants. Participants described feeling dysphoric when they were unable to present in the way that they intended or desired, due to ill-fitting clothing, or perceived pressure to present as their sex presumed at birth.
Despite the severity of experiences detailed above, participants described frequent occurrences of gender euphoria; the distinct comfort, connection, pleasure, or excitement associated with gender-affirmation. Two hundred and fifty individual references to sources of gender euphoria were identified across the data and included packing (i.e., wearing a phallic object to create a visible bulge), chest binding (i.e., flattening breasts using constrictive materials), presentation choices (e.g., clothing, makeup, hairstyles), body modifications (e.g., piercings, tattoos, dying hair), anticipated or active hormone therapy, anticipated or complete gender-affirming surgery, viewing gender-affirming images of oneself and gender-affirming social encounters.
Most commonly, gender euphoria was derived from a sense of comfort and satisfaction with one’s body, achieved by physically affirming one’s gender identity. One participant reported packing, while seven participants reported chest binding, as sources of gender euphoria. Gender euphoria frequently manifested cognitively for participants, based in the anticipation or visualisation of their future selves, post-gender-affirming hormone therapy or surgery.
Participants described either undergoing or visualising future gender-affirming surgery as a source of gender euphoria. Participants expressed excitement and pleasure describing gender-affirming surgery. In addition to participants’ self-perception, external perspectives, and interactions with one’s social environment were a source of gender euphoria for five participants. This included being in romantic relationships, receiving compliments, and being gendered correctly.
The present findings illustrate the diversity of experiences of body image within the non-binary community. The current findings have several important implications for researchers, clinicians, and policy makers. First, the findings suggest that having access to gender-affirmation (for those who want it) can play a key role in reducing gender dysphoria, facilitating euphoria, and shaping general positive wellbeing for gender non-binary people. Second, these findings suggest there may be some utility in making ‘pubertal blockers’ available for non-binary adolescents experiencing gender dysphoria. Third, the finding that menstruation was a source of severe gender dysphoria for most participants, presents preliminary support that there may be benefit to increased availability of hormonal contraception for non-binary people.
Some participants valued medical and surgical affirmation as important sources of gender euphoria that simultaneously make their gender visible, other participants had gained body confidence since psychologically affirming their non-binary identity and described feeling liberated from cis-normative expectations of body image. Overall, the findings highlight the heterogeneity of gender non-binary experiences of body image and deepen current theoretical understandings of the conceptualisations of non-binary body, body image, and body ideals.
From: Body image and treatment desires at clinical entry in non-binary and genderqueer adults. Huisman B et al. [2022] International Journal of Transgender Health.
Gender identity clinics around the world report an increasing number of individuals with symptoms of gender incongruence (GI) who seek medical assistance. GI refers to those individuals whose gender identity, the experience of being or belonging to a gender, is not in line with their birth-assigned sex. When this incongruence results in significant psychological distress or physical discomfort, it is described as gender dysphoria (GD). Historically, most individuals with GD reported to have a binary gender identity, referring to the experience of being male or female. Overall, this study provides considerable insight into the experience of body dissatisfaction in NBGQ people and their motives for GAMT at clinical entry. There are three key findings of this study.
First, the study provides supporting evidence that NBGQ individuals, much like BT people, seek GAMT due to discomfort with their bodies. However, their body dissatisfaction appears less severe and more cantered on specific regions of the body compared to BT individuals. NBGQ referrals are primarily dissatisfied with publicly visible body regions, but less so with more private body areas such as the genital area. The body dissatisfaction of BT individuals appears to reside more broadly across the body, as they report dissatisfaction with both genital and non-genital areas.
The second main finding of this study is that NBGQ people opt for less modalities of GAMT, primarily by showing less interest in gender-affirming genital surgery.
Third, gender identity appeared a significant predictor of the likelihood that one would prefer a selection of GAMT. At equal levels of body dissatisfaction, NBGQ persons desire fewer GAMT interventions than BT people. NBGQ individuals thereby report their gender identity and the lack of genital dysphoria as primary motivators, whereas BT individuals who do not opt for specific medical interventions more frequently motivate this decision from the perspective of anticipated risks of interventions or unsatisfactory results.
This study nevertheless indicates dissatisfaction with the body as an important contributing component of gender distress in NBGQ individuals seeking GAMT. By interpreting their body dissatisfaction in the context of social gender stressors, it may be possible to understand why their body dissatisfaction is primarily focused on body features that affect gender expression and social gender recognition, and less cantered around private areas of the body.
Satisfactorily enacting a NBGQ identity appears to be a complex balance between various gender domains in interaction with one’ s social context. Body dissatisfaction has a significant role in the experience of GI, But should be contextualized in relation with other gender domains. Although GAMT leads to greater body satisfaction and reduced physical distress, it may insufficiently alleviate overall gender distress in NBGQ people.
In conclusion, similar to BT individuals, physical gender distress appears to be a major motivator for initiating GAMT in NBGQ individuals. However, NBGQ body dissatisfaction seems less severe and NBGQ people desire fever GAMT interventions. In clinical practice, it is important to be attentive to the unique treatment desires and motives of NBGQ individuals, and to carefully assess how GAMT can reduce their gender distress. Hence, clinical practice should aim to provide personalized treatment pathways that both improve body satisfaction and reduce GI in other areas of life.
From: Hair removal and psychological well-being in transfeminine adults: associations with gender dysphoria and gender euphoria. Bradford N, Rider G, Spencer K. [2019] Journal of Dermatological Treatment.
Hair removal procedures, including electrolysis and laser hair removal, are the most commonly pursued gender-affirmative medical interventions by transfeminine people, but previous empirical studies have not examined their relationship to psychological well-being.
Satisfaction with one’s current state of hair removal was negatively correlated with situational body image dysphoria, depression symptoms, anxiety symptoms, and negative affect, and positively correlated with positive affect.
Results of this study suggest that hair removal is associated with both decreased distress but also increased subjective well-being (e.g. higher positive affect). Though the construct of ‘gender euphoria’ has been introduced in previous publications, it has thus far not been rigorously defined or operationalized within health research. These results suggest that gender euphoria can be understood in terms of increased subjective well-being associated with gender affirmation, including gender-affirmative medical interventions. This study demonstrates a significant association between hair removal services and depression symptoms, anxiety symptoms, situational body image dysphoria, positive affect, and negative affect in transfeminine adults. These findings cast significant doubt on the assertion that hair removal services for transfeminine people are ‘cosmetic.’
From: Analyzing body dissatisfaction and gender dysphoria in the context of minority stress among transgender adolescents. Brecht A et al. [2024] Child and Adolescent Psychiatry and Mental Health.
Gender dysphoria among transgender adolescents has predominantly been examined in relation to body dissatisfaction. While in adult transgender samples, body dissatisfaction is higher than in cisgender controls, this has so far rarely been investigated for adolescents. In the context of a cisnormative society, the impact of influences from the social environment on body dissatisfaction and gender dysphoria has been neglected in research. Therefore, this study aimed to (1) provide a detailed analysis of body dissatisfaction among young transgender people and (2) investigate whether body dissatisfaction and gender dysphoria are associated with experiences of minority stress such as trans hostility and poor peer relations (PPR).
Transgender adolescents reported more body dissatisfaction than cisgender peers. The dissatisfaction with sex characteristics, non-hormonal reactive body regions and the total score for body dissatisfaction were positively related with gender dysphoria. The majority had experienced trans hostility in the present and/or past (54.1%) and PPR (63.5%). More body dissatisfaction was correlated with more PPR regarding visible body parts i.e., hair, overall appearance and muscles, whilst PPR and gender dysphoria were not associated. Transgender adolescents who experienced trans hostility showed higher gender dysphoria and PPR, but not more body dissatisfaction. In multiple regression, trans hostility predicted gender dysphoria, whilst age and PPR predicted body dissatisfaction.
Undoubtedly, transgender people still represent a marginalized group in mostly cis normative (social norms that strongly rely on cisgender and binary ideas) societies and experience discrimination and (micro)-aggression on a daily basis, covered by the term minority stress. Transgender adolescents experience bullying and poor peer relations (PPR) significantly more often than their cisgender peers. Chronic exposure of discrimination and hostility leads to their internalization (Internalized Transphobia) and eventually auto-aggression, self-depreciation and other related mental health issues.
This study indicates that clinic-referred transgender adolescents show higher body dissatisfaction for all body regions than their cisgender peers. Experiences of minority stress such as poor peer relations and trans hostility are specifically associated with body dissatisfaction and with gender dysphoria. Adequate, validated and revised instruments – in line with recent changes in terminology and classification – to assess body dissatisfaction, gender dysphoria and aspects of minority stress are needed, especially for the age group of adolescents. While this research needs time, clinicians need to be aware of the societal impact on gender minority individuals, address this in the counselling setting and provide support for the youth.
From: Preferences for and barriers to gender affirming surgeries in transgender and non-binary individuals. Tristani-Firouzi B. [2021] International Journal of Transgender health.
The transgender/non-binary community continues to be an underserved population in medicine, and our understanding of their interests, disinterests, and barriers to transition-related healthcare is quite limited, especially among the diverse gender identities within the transgender/non-binary umbrella.
Compared to the 2015 US Transgender Survey, interest in gender affirming surgeries was higher across all gender identities surveyed and for all procedures, by an average of 38%. Interest overall in gender affirming procedures varied greatly among gender identity groups as well as with age differences. Barriers were found to be a mixture of lack of resources for recovery, financial, and a fear of complications.
Results highlight that a desire for these procedures is unique for each individual and should never be assumed for transgender/non-binary patients. In order to better aid this underserved population, the medical community must further work to mitigate the barriers to gender affirming procedures by decreasing cost, investigating ways to increase access to resources for recovery, and improving outcomes for each of the gender affirming surgeries.
To better aid a drastically underserved population in medicine, we must fully understand the desires for and barriers to trans/non-binary people’s healthcare. While a direct comparison to the 2015 USTS is not possible, our data suggests that since 2015 interest in surgical transition has increased across all gender identities for all procedures, most dramatically for non-binary individuals. This study also demonstrated that barriers to the procedures are varied and diverse. It is not only the cost that must be mitigated to increase access, but there must be more resources for recovery on a broader societal level, meaning less stigma of taking time off work for a gender affirming procedure, as well as more research into improving outcomes for specific surgeries. It is further critical to keep in mind that transition means different things for each individual. Given that the interest to GAS varied considerably within each gender identity, is it important never to assume that any one trans/non-binary person wants or needs a particular procedure for their transition. Recognizing that not all trans/non-binary people wish to partake in all GAS is an important step toward improving healthcare for this community. With the high risk of mental illness in this population, it is especially critical that we improve our understanding of trans/non-binary patients’ needs and desires to work at improving their healthcare experiences.
Key Literature References
*** Gynecological gender-affirming surgeries: what are the motivations and experiences? A qualitative study (2025), by Asra Vestering, et al., published in The Journal of Sexual Medicine
(Notable) *** Exploring body image among transgender and nonbinary adults: Considering positive body image and the pursuit of gender-affirming surgery (2025), by Charlotte H Markey, et al., published in Journal of Health Psychology
*** Analyzing Body Dissatisfaction and Gender Dysphoria in the Context of Minority Stress among Transgender Adolescents (2024), by Alexandra Brech, et al., published in the journal Child and Adolescent Psychiatry and Mental Health
*** Body Contouring as Gender-Affirming Surgery in Transgender Patients: A Systematic Review of the Current Literature (2024), by Alejandra Aristizábal, et al., published in the Journal of Clinical Medicine
*** Transgender Women’s Perspectives on Mental Health Care Related to Vaginoplasty for Gender Affirmation (2024), by Emily E. Marra, et al., published in BMC Women’s Health
*** Dermatological aspects of gender affirming medical treatment in transgender and gender diverse people: a systematic review (2024), by Jon Arcelusa Nottingham, et al., published in the International Journal of Transgender Health
(Notable) *** Experiences of body image in the gender non-binary community: A qualitative analysis (2024), by Jaz Burstall, et al., published in the journal Body Image
(Notable) *** Association between genital gender-affirming surgery and psychiatric comorbidities in individuals with gender incongruence (2024), by Kassra Garoosi, et al., published in The Journal of Sexual Medicine
*** Outcomes of a Standardized Pain Pathway for Transgender Patients Undergoing Vaginoplasty and Vulvoplasty (2024), by Emily Burney, et al., published in the journal Urology
(Notable) *** “Coming home to my body”: A qualitative exploration of gender-affirming care-seeking and mental health (2023), by Teddy G. Goetz, et al., published in the Journal of Gay & Lesbian Mental Health
*** Effects of Hormones on Breast Development and Breast Cancer Risk in Transgender Women (2023), by Martine Berliere, et al., published in the journal Cancers
*** Genital gender-affirming surgery for transgender women (2023), by Wouter B. van der Sluis, et. al., published in Best Practice & Research Clinical Obstetrics & Gynaecology
(Notable) *** Body Image and Treatment Desires at Clinical Entry in Non-binary and Genderqueer Adults (2022), by Bodi Huisman, et. al, published in the International Journal of Transgender Health
*** Preferences for and barriers to gender affirming surgeries in transgender and non-binary individuals (2022), by Bita Tristani-Firouzi, et al., International Journal of Transgender Health
*** Assigned-Female-at-Birth Trans Masculine and Non-Binary Individuals Differ in their Body Satisfaction and Desire for Gender Affirming Treatments (2022), by Catherine Schaeff, published in the journal Archives of Sexual Behavior
*** Complications and Patient-reported Outcomes in Transfemale Vaginoplasty: An Updated Systematic Review and Meta-analysis (2021), by Samyd S. Bustos, published in Plastic & Reconstructive Surgery
(Notable) *** Hair removal and psychological well-being in transfeminine adults: associations with gender dysphoria and gender euphoria (2021), by Nova J.Bradford,et al., published in the Journal of Dermatological Treatment
*** “Certain Parts of my Body Don’t Belong to Me”: Trans Individuals’ Descriptions of Body-Specific Gender Dysphoria (2020), by Lex Pulice-Farrow, M. Paz Galupo, and Claire E. Cusack, published in the journal Sexuality Research and Social Policy
>> (Chapter 19) How has sexuality among transgender and gender-diverse individuals been researched in recent years?
Overview by Laura Henton, DNP, APRN, FNP-C
Research on sexuality among transgender and gender-diverse individuals has centered around the development of gender identity and sexual orientation in this population, challenging cultural and scientific assumptions about gender and sexuality. Several narratives exist (in the United States), which support “sexual and gender diversity: (a) gender as self-constructed; (b) sexuality as plural, playful, flexible, and fluid; (c) sexuality and monogamy as cultural compulsions; and (d) intersectionality as central to the experience of sexuality and gender” (Hammack & Manago, 2025, p. 375). This section will address a variety of the research that has been performed on these topics.
Gender as Self-Constructed
Burns and colleagues (2024) write on the topic of hormone therapy and sexuality in trans individuals. They looked at a large number of completed studies (their reference list encompasses 165 citations) and focused on specific aspects of sexuality: “… physical changes, sexual desire, contributors to sexual satisfaction and sexual distress, experiences of sexual orientation or identity, and sexual behaviors,” (Burns et al., 2024, p. 17) as they relate to hormone therapy. Physical changes brought on by hormone therapy are viewed by these authors as “built upon white supremacy” and “associated with whiteness” (Burns et al., 2024, p. 20). Sexual desire after hormone therapy inversely correlated with gender dysphoria: individuals with lower baseline dysphoria experienced higher sexual desire. Unsurprisingly, sexual satisfaction was found to be related to body satisfaction, especially in trans women. These researchers uncovered that hormone therapy prompts some trans individuals to change their sexual orientation, through increased self-confidence and self-knowledge. An increase in libido, due to hormone therapy, was seen to increase risky sex acts for some individuals.
Researchers Fornander et al. (2024), interested in sexual behaviors of transgender adolescents, conducted a retrospective chart review of 323 youth, aged 13-18, who were patients at a gender clinic. They determined that rates of dating and rates of sexual behavior were lower in transgender teens than national norms.
Gil-Llario et al. (2021) examined sexual behavior, before treatment, of 260 trans individuals from a transgender health clinic in Spain. These researchers inquired about incest, sexual abuse, rape, masturbation, fantasies, orgasm, frequency of intercourse, and who initiates sex. They found “lower sexual desire, sexual arousal without orgasm, and overall sexual health in trans women” (Gil-Llario et al., 2021, p. 304).
In Boston, researchers Hereth and colleagues (2020) interviewed 18 young (aged 18-29) transgender men who had sex with cisgender men, with the initial intent to determine the feasibility of an HIV-prevention program aimed at transgender men who have sex with men. Participants spoke of their search of finding labels for their gender identity and/or sexual orientation. These participants also addressed the issue of “losing” their community or not fitting in: formerly a member of the lesbian community; now after medically or socially transitioning, not able to return to that community. Another theme discussed was the idea of “coming out” twice or multiple times: first as a transgender man, then as a queer or gay transgender man.
Holmberg et al. (2019) write about the biopsychosocial model of sexual response and its components of hormonal control of sexuality and function, pretreatment sexuality in trans persons, sexuality and gender-affirming treatment, post-treatment sexuality, supporting sexuality in transgender persons, and psychotherapy and psychoeducation. Hormones and surgery are discussed under the heading of gender-affirming treatments, with diagrams of vaginoplasty, phalloplasty, and metoidoplasty techniques diagrammed. Post-treatment sexuality includes discussion of desire, sexual arousal, orgasm, pain during sexual activity, and sexual satisfaction. These authors assert that “gender-affirming surgery can improve body satisfaction and ease gender dysphoria” (Holmberg et al., 2019, p. 121) but caution that surgery can be associated with pain or psychological difficulties.
Kennis, Duecker, et al. (2023) evaluated the daily journals of 47 transgender and 52 cisgender adults (aged 18-65) who reported on their sexual behavior (sexual activity, intimacy, masturbation, and sexual openness), sexual esteem, and body image. They found that while transgender individuals had lower sexual esteem and body image scores, sexual behavior scores were the same between groups.
Kennis, Kreukels, and Dewitte (2023) note that sexuality in transgender individuals, as addressed in medical literature, focuses a great deal on negative experiences such as sexual violence and sexually-transmitted infections. These authors encourage future researchers to focus instead on sexual pleasure, and address the psychological and social aspects of sexual wellbeing.
Researchers Ozer and colleagues (2023) interviewed 15 transgender adults, half of whom were over the age of 50. They concluded that “positive experiences, feeling comfortable with body/self, intimacy,” and acceptance and communication with one’s partner were helpful in experiencing sexual wellbeing (Ozer et al., 2023, p. 608).
Dutch researchers Ozer et al. (2022) reviewed 172 studies on trans individuals, looking for themes or topics of sexual wellbeing. Four themes emerged from their review: genital function, sexual pleasure, quality of sex life, and sexual satisfaction. They note that a recent shift from disease/dysfunction to positive sexuality, encompassing sexual pleasure and quality of sex life, is a healthy change in attitude.
Twenty-one transgender participants were interviewed by Ross et al. (2024) regarding sexuality and gender-affirming treatments. They determined that the ability to re-define “sex” and affirming one’s gender identity correlated with a satisfactory sex life; another contributing factor was emotional connection with one’s partner.
Sexuality as Plural, Playful, Flexible, and Fluid
Atlanta marriage and family therapist Chapman (2024) interviewed 30 transgender adults with a goal of determining how sexual satisfaction is defined by transgender individuals. Three themes evolved: definitions of sex, partner selection, and mitigating gender dysphoria.
Anzani et al. (2025) interviewed 115 transgender and nonbinary individuals in order to better understand the use and role of sex toys. Their research showed that “sex toys can be empowering tools that help individuals explore their identities” as well as for pleasure (Anzani et al., 2025, p. 128).
Researchers Gieles et al. (2023) queried 325 transgender individuals by way of the Amsterdam Sexual Pleasure Index (ASPI), looking to validate this instrument as well as compare scores to cisgender individuals. The ASPI is a 44-item questionnaire which assesses an individual’s tendency to experience sexual pleasure. These authors found that transgender persons had significantly lower ASPI scores than their cisgender peers.
Gieles et al. (2024) interviewed 13 mental healthcare professionals, and determined that most of those interviewed felt that care to transgender and cisgender patients was not different. The authors stress that healthcare providers must be cognizant of societal and identity-related factors which may contribute to sexual problems.
Researchers Lindley and colleagues (2021), dissatisfied with previous quantitative studies which focused more on trans feminine individuals, investigated sexual satisfaction in trans masculine and nonbinary persons. After interviewing 358 participants, these researchers uncovered two categories: universal (such as frequency of orgasm and partner dynamics) and trans-related. The authors suggest that general aspects of sexual satisfaction discussed were more similar than dissimilar to cisgender individuals.
Lindley et al. (2022) interviewed 44 individuals (22 nonbinary; 22 cisgender men and women) regarding sexual fantasy. These researchers found that among nonbinary individuals, sexual fantasies were more likely to reference non-normative genitals, and less likely to refer to themselves as desirable. The authors stress that, given the scarcity of research on sexual experiences of transgender persons, this leads to a shortage in sex education [for transgender persons] and therapy for transgender persons to understand their sexuality.
Mangas and Sierra (2025) conducted a review of 333 articles in 147 journals, to determine the frequency with which sexual satisfaction among the gender-diverse is discussed. They noticed a rise in frequency starting in 2005, peaking in 2023. They also noted multiple research groups with no collaboration between them.
Ward et al. (2024) interviewed 12 trans women regarding their experiences of sexuality during gender transition. Two themes emerged: increased confidence and comfort in exploring sexuality, and new/different aspects of sexuality as a result of transitioning.
Sexuality and Monogamy as Cultural Compulsions
Psychologists Hammack and Manago (2025) suggest five principles for research and clinical practice regarding sexual and gender diversity. They suggest grounded psychological science and practice in lived experience; challenging normative thinking; practice of affirmation; centering the phenomenon of diversity; and embracing fluid and nonlinear narratives.
Researchers Warwick and colleagues (2022) interviewed 30 transgender adolescents (aged 15-20) at a gender services clinic on the topic of sexual health and education. Libido, family and school-based sex education, and counseling were discussed. One-third of the participants came from families who did not discuss sex. Participants thought that school-based sex education was useful only for their cisgendered classmates. These participants trusted the counseling provided by their gender-affirming providers, but found their other healthcare providers lacking training.
Anzani et al. (2023) investigated stereotypes associated with trans individual’s sexuality. Interviews of nearly 300 (n = 297) transmasculine and nonbinary individuals uncovered four themes: deviance, discomfort with sexuality, stereotypes based on gender, and absence of stereotyping. These authors suggest inclusivity and community welfare be promoted by confronting stereotypes in social environments.
Intersectionality as Central to the Experience of Sexuality and Gender
Mattawanon and colleagues (2021) conducted a review of 44 studies (most of which were retrospective) which addressed sexual satisfaction and sexual function. Other topics examined were sexual desire, arousal, sexual behavior, and orgasm. They found that transgender women tended to have more sexual dysfunction that transgender men, and that gender-affirming therapies and surgery improved the sexual satisfaction of transgender individuals, male and female. These authors suggest that more research be directed at including nonbinary individuals, and note that sexuality is determined by hormonal, surgical, physiologic, psychological, and social factors.
Pipkin et al. (2024) conducted a meta-ethnographic review of 16 studies. A meta-ethnographic review is “a systematic approach which synthesizes data from multiple studies to enable new insights into patients’ and healthcare professionals’ experiences and perspectives” (Sattar et al., 2021, para. 1). Their work uncovered the need for re-writing labels: labeling gender and sexuality, re-labeling body parts, and labels for relationships.
The definition of sexuality can include how individuals understand and experience their sexual feelings, thoughts, attractions, and behaviors towards others, as well as how one identifies, the nature of sexual and romantic attraction, and preferences in relationships. Puckett et al. (2021) conducted a systematic review of 179 journal articles that examined what aspect of sexuality – behaviors, attraction, or identity – was measured. They found that very few studies reported two or more dimensions of sexuality. Writers Ollen and Vencill (2021), reviewing Puckett’s work, note the distinction between sexuality/sexual orientation and gender identity/expression, and provide a list of resources for providers.
Sexual orientation in transgender adults was the subject of study by Reisner and colleagues (2023), who surveyed 1436 American adults, roughly 20 percent of whom identified as transgender. Ten percent of the cisgender participants identified as a sexual minority; 82 percent of the transgender participants identified in this manner. Nearly 20 percent of the cisgender respondents and nearly 30 percent of the transgender respondents did not have sex in the five years prior to the survey. Six percent of cisgender participants and 64 percent of transgender participants reported being attracted to more than three partner genders. These authors suggest that, in order to emphasize the diversity of transgender persons, researchers use the terms sexual identities, behaviors, and attractions – the plural, rather than the singular.
Whitney et al. (2022) write on the lack of a scientific definition of sexual function and an accompanying measurement tool for transgender persons, noting that such has been developed for cisgender individuals. These authors also caution against the pathologization of low sexual desire or asexuality altogether.
Kennis et al. (2024) write about the need for a diagnosis of gender dysphoria before gender-affirming treatment (hormones or surgery) is approved or accessible, as well as the ethical questions of performing MRIs to determine the difference between the transgender and cisgender brain. These authors suggest establishment of an advisory board, using multidisciplinary research teams, prioritization of helpful research, and rethinking how ethical approval is obtained.
References
Anzani, A., Siboni, L., Lindley, L., Galupo, M. P., & Prunas, A. (2023). From abstinence to deviance: Sexual stereotypes associated with transgender and nonbinary individuals. Sexuality Research and Social Policy, 21, 27-43. https://doi.org/10.1007.s13178-023-00842-y
Burns, J. A., Beischel, W. J., & van Anders, S. M. (2024). Hormone therapy and trans sexuality: A review. Psychology of Sexual Orientation and Gender Diversity, 11(1), 17-30. https://doi.org/10.1037/sgd0000588
Chapman, K. (2024). Pathways to pleasure: Understanding sexual experiences and satisfaction in transgender individuals. [Unpublished doctoral dissertation]. Widener University.
Cilveti-Lapeira, M., Rodríguez-Molina, J. M., & López-Trenado, E. (2024). Key aspects in the development of gender identity and sexual orientation according to trans and gender diverse people: a qualitative approach. Culture, Health & Sexuality, 1-15. Advance online publication. https://doi.org/10.1080/13691058.2024.2416541
Fornander, M. J., (2024). Self-reported sexual behavior of transgender youth. Journal of Pediatric and Adolescent Gynecology, 37(3), 336-341. https://doi.org/10.1016/j.jpag.2023.12.003
Gieles, N. C., Gerritse, K., Zandbergen, E., & Both, S. (2024). “Sex is not just an act but also a place to be human, to be authentic.”: A qualitative interview study on practices of healthcare professionals in sexological care for transgender and non-binary people. International Journal of Transgender Health. https://doi.org/10.1080/26895269.2024.2307359
Gieles, N. C., van de Frift, T. C., Elaut, E., Heylens, G., Becker-Hebly, I., Nieder, T. O., Laan, E.T. M., Kreukels, B. P. C. (2023). Pleasure please! Sexual pleasure and influencing factors in transgender persons: A ENIGI follow-up study. International Journal of Transgender Health, 24(2), 212-224. https://doi.org/10.1080/26895269.2022.2028693
Gil-Llario, M. D., Gil-Jilia, B., Gimenez-Garcia, C., Bergero-Miguel, T., & Ballester-Arnal, R. (2021). Sexual behavior and sexual health of transgender women and men before treatment: Similarities and differences. International Journal of Transgender Health, 22(3), 304-315. https://doi.org/10.1080/26895269.2020.1838386
Hammack, P. L. & Manago, A. M. (2025). The psychology of sexual and gender diversity in the 21st Century: Social technologies and stories of authenticity. American Psychologist, 80(3), 375-388. https://doi.org/10.1037/amp0001366
Hereth, J., Pardee, D. J., & Reisner, S. L. (2020). Gender identity and sexual orientation development among young adult transgender sexually active with cisgender men: ‘I had completely ignored my sexuality … that’s for a different time to figure out.’ Culture, Health & Sexuality, 22(S1), 31-47. https://doi.org/10.1080/13691058.2019.1636290
Holmberg, M., Arver, S., & Dhejne, C. (2019). Supporting sexuality and improving sexual function in transgender persons. Nature Reviews Urology, 16, 121-139. https://doi.org/10.1038/s41585-018-0108-8
Kennis, M., Duecker, F., Elaut, E., T’Sjoen, G., Loeys, T., & Sack, A. T. (2023). Daily sexual behavior, sexual esteem, and body image in transgender and cisgender individuals. The Journal of Sex Research, 60(6), 859-867. https://doi.org/10.1080/00224499.2022.2158172
Kennis, M., Staicu, R., Dewitte, M., T’Sjoen, G., Sack, A. T., & Duecker, F. (2024). Heed lessons from past studies involving transgender people: First, do no harm. Nature 629, 998-1000. https://doi.org/10.1038/d41586-024-01521-7
Kennis, M., Kreukels, B. P. C., & Dewitte, M. (2023). Sex & relationships in trans people. Best Practice & Research Clinical Obstetrics and Gynaecology, 86, 102294. https://doi.org/10.1016/j.bpobgyn.2022.102294
Lindley, L., Anzani, A., Prunas, A., & Galupo. M. P. (2021). Sexual satisfaction in trans masculine and nonbinary individuals: A qualitative investigation. The Journal of Sex Research, 58(2), 222-234. https://doi.org/10.1080/00224499.2020.1799317
Mangas, P., Sierra, J. C. (2025). Sexual satisfaction in people and couples belonging to sexual orientation and gender diversities: A bibliometric analysis. Sexual Medicine Reviews, 00(00), 1-11. https://doi.org/10.1093/sxmrev/qeaf019
Mattawanon, N., Charoenkwan, K. & Tangpricha, V. (2021). Sexual dysfunction in transgender people: A systematic review. Urologic Clinics of North America, 48(4), 437. https://doi.org/ 10.1016/j.ucl.2021.06.004
Ollen, E. W. & Vencill, J. A. (2021). Measurement of sexuality for trans and gender diverse populations: Application of the 2021 APA Guidelines for Psychological Practice with Sexual Minority Persons. Psychology of Sexual Orientation and Gender Diversity, 8(3), 378-379. https://doi.org/10.1037/sgd0000529
Özer, M., Poor, T. S., Gijs, L., Kreukels, B. P. C., & Mullender, M. G. (2022). The assessment of sexual wellbeing in treatment-seeking transgender individuals: A systematic review of the medical literature. International Journal of Impotence Research, 35(2), 121-131. https://doi.org/ 10.1038/s41443-022-00529-9
Özer, M., de Kruif, A. J. T. C. M., Gijs, L. A. C. L., Kreukels, B. P. C., & Mullender, M. G. (2023). Sexual wellbeing according to transgender individuals. International Journal of Transgender Health, 35(4), 608-624. https://doi.org/10.1080/19317611.2023.2227172
Pipkin, A., Ward, L., Cotton, S., & Shearn, C. (2024). The experience of navigating sexuality for transgender and gender non-conforming people: A meta-ethnographic review. International Journal of Transgender Health, 25(4), 634-652. https://doi.org/ 10.1080/26895269.2023.2260795
Puckett, J. A., Glozier, K., Kimball, D., & Giffel, R. (2021). A systematic review of sexuality measurement in transgender and gender diverse populations. Psychology of Sexual Orientation and Gender Diversity, 8(3), 276-291. https://doi.org/10.1037/sgd0000523
Reisner, S. L., Choi, S. K., Herman, J. L., Bockting, W., Krueger, E. A. & Meyer, I. H. (2023). Sexual orientation in transgender adults in the United States. BMC Public Health, 23, 1799.
Ross, M., Roijer, P., Mullender, M., & van de Grift, T. (2024). Trans, gender non-conforming and non-binary individuals’ perspectives on experienced sexuality during medical transition. Journal of Sex & Marital Therapy, 50(3), 379-394. https://doi.org/10.1080/0092623X.2023.2300828
Sattar, R., Lawton, R., Panagioti, M., & Johnson, J. (2021). Meta-ethnography in healthcare research: A guide to using a meta-ethnographic approach for literature synthesis. BMC Health Services Research, 21(50). https://doi.org/10.1186/s12913-020-06049-w
Ward, L., Pipkin, A., Frary, G., & Kempinska, C. (2024). “Rediscovering what I need to do to give myself pleasure.” Trans women’s experiences of their sexualities during gender transition: An interpretative phenomenological analysis. Psychology of Sexual Orientation and Gender Diversity. Advance online publication. https://dx.doi.org/10.1037/sgd0000728
Warwick, R. M., Araya, A. C., Shumer, D. E., & Selkie, E. M. (2022). Transgender youths’ sexual health and education: A qualitative analysis. Journal of Pediatric and Adolescent Gynecology, 35(2), 138-146. https://doi.org/10.1016/j.jpag.2021.09.011
Whitney, N., Samuel, A., Douglass, L., Strand, N. K., & Jahromi, A. H. (2022). Avoiding assumptions: Sexual function in transgender and non-binary individuals. The Journal of Sexual Medicine, 19(6), 1032-1034. https://doi.org/10.1016/j.jsxm.2022.03.214
Key Literature References
(Notable) *** Sexual satisfaction in people and couples belonging to sexual orientation and gender diversities: a bibliometric analysis (2025), by Pablo Mangas & Juan Carlos Sierra, published in Sexual Medicine Reviews
(Notable) *** The Psychology of Sexual and Gender Diversity in the 21st Century: Social Technologies and Stories of Authenticity (2025), by PL Hammack, et al., published in American Psychologist
(Notable) *** The experience of navigating sexuality for transgender and gender non-conforming people: a meta-ethnographic review (2024), by Alastair Pipkin, et al., published in the International Journal of Transgender Health
(Notable) *** Hormone therapy and trans sexuality: A review (2024), by Jason A. Burns, et al., published in the journal Psychology of Sexual Orientation and Gender Diversity
(Notable) *** From Abstinence to Deviance: Sexual Stereotypes Associated With Transgender and Nonbinary Individuals (2024), by Annalisa Anzani, et al., published in the journal Sexuality Research & Public Policy
(Notable) *** “Rediscovering What I Need to Do to Give Myself Pleasure.” Trans Women’s Experiences of Their Sexualities During Gender Transition: An Interpretative Phenomenological Analysis (2024), by Luke Ward, et al., published in the journal Psychology of Sexual Orientation and Gender Diversity
(Notable) *** “Sex is not just an act but also a place to be human, to be authentic.” A qualitative interview study on practices of healthcare professionals in sexological care for transgender and non-binary people (2024), by Noor C. Gieles, published in International Journal of Transgender Health
(Notable) *** Self-Reported Sexual Behavior of Transgender Youth (2024), by Mirae J. Fornander, et al., published in Journal of Pediatric and Adolescent Gynecology
*** Trans, gender non-conforming and non-binary individuals’ perspectives on experienced sexuality during medical transition (2024), by Maeghan Ross, et al., published in Journal of Sex & Marital Therapy
*** Pathways to Pleasure: Understanding Sexual Experiences and Satisfaction in Transgender Individuals (2024), by Kristin Chapman, unpublished PhD Dissertation, Widener University
(Notable) *** The assessment of sexual wellbeing in treatment-seeking transgender individuals: a systematic review of the medical literature (2023), by M. Özer, et al., published in the International Journal of Impotence Research
(Notable) *** Pleasure please! Sexual pleasure and influencing factors in transgender persons: An ENIGI follow-up study (2023), by Noor C. Gieles, et al., published in the International Journal of Transgender Health
(Notable) *** Daily Sexual Behavior, Sexual Esteem, and Body Image in Transgender and Cisgender Individuals (2023), by Mathilde Kennis, et al., published in The Journal of Sex Research
(Notable) *** Sex & relationships in trans people (2023), by Mathilde Kennis, et al., published in Best Practice & Research Clinical Obstetrics & Gynaecology
(Notable) *** Sexual Wellbeing according to Transgender Individuals (2023), by Mujde € Ozer, et al., published in International Journal of Transgender Health
*** The use of sex toys in trans and nonbinary individuals’ sexuality (2023), by Annalisa Anzani, et al., published in Sexual and Relationship Therapy
*** Sexual Functioning of Transgender Females Post-Vaginoplasty: Evaluation, Outcomes and Treatment Strategies for Sexual Dysfunction (2022), by Jessica N. Schardein, MD & Dmitriy Nikolavsky, MD, published in Sexual Medicine Reviews
(Notable) *** A Systematic Review of Sexuality Measurement in Transgender and Gender Diverse Populations (2021), by J. A. Puckett, et. al, published in the journal Psychology of Sexual Orientation and Gender Diversity
*** Sexual Satisfaction in Trans Masculine and Nonbinary Individuals: A Qualitative Investigation (2021), by Louis Lindley, et al., published in The Journal of Sex Research
(Notable) *** Sexual behavior and sexual health of transgender women and men before treatment: Similarities and differences (2021), by María Dolores Gil-Llario, et al., published in International Journal of Transgender Health
*** Measurement of Sexuality for Trans and Gender Diverse Populations: Application of the 2021 APA Guidelines for Psychological Practice with Sexual Minority Persons (2021), by Elizabeth W. Ollen and Jennifer A. Vencill, published in Psychology of Sexual Orientation and Gender Diversity
(Notable) *** Sexual Dysfunction in Transgender People: A Systematic Review (2021), by Natnita Mattawanon, et al., published in Urologic Clinics of North America
*** Transgender Youths’ Sexual Health and Education: A Qualitative Analysis (2021), by Rebecca M. Warwick, et al., published in Journal of Pediatric and Adolescent Gynecology
(Notable) *** Supporting Sexuality and Improving Sexual Function in Transgender Persons (2019), by Mats Holmberg, Stefan Arver & Cecilia Dhejne, published in Nature Reviews Urology
>> (Chapter 20) What research has investigated sexual function/dysfunction among transgender and gender diverse individuals?
Overview, by Scott Kerlin
Sexual Dysfunction, Wellbeing, and Gender Identity/Transgender
In 2021, Natnita Mattawanon, et al, published a comprehensive review of sexual dysfunction in transgender people, reporting that sexual dysfunction is common in transgender people. They summarized that (1) Gender-affirming hormone therapy decreases sexual desire and activity in transwomen but increases sexual desire and activity in transmen; (2) Gender-affirming surgery helps to improve sexual satisfaction in both transmen and transwomen; (3) Differences in hormone regimens and surgeries may impact sexual function; and (4) There is a need for validated tools to assess sexual function and satisfaction in the transgender population.
In a 2019 study, “Prevalence of Sexual Dysfunctions in Transgender Persons”, Kerckhof and colleagues observed, “The most frequent sexual dysfunctions experienced by trans women and trans men were difficulties
initiating and seeking sexual contact (26% and 32%, respectively) and difficulties achieving an orgasm (29% and15%, respectively). Compared with trans women after hormone treatment and non-genital surgery, trans women
after vaginoplasty less often experienced arousal difficulties, sexual aversion, and low sexual desire. Compared with trans men without medical treatment, trans men after a phalloplasty experienced sexual aversion and low
sexual desire less often. No significant differences were found between participants with or without further genital treatment intentions.
Clinical implications: Clinicians should consider sexual counseling after medical treatments, paying particular attention to potential social and psychological barriers to the sexual health of their patients.”
Ozer, et al., 2022 assessed “sexual well-being” in treatment-seeking transgender individuals and concluded, “at present no suitable measures exist to comprehensively assess or evaluate sexual wellbeing in transgender
individuals. Although a broad range of themes in relation to sexual health have been studied in transgender individuals, used measures are not validated and study quality is generally low. To move forward in this field, better designs and first and foremost a better understanding of the concept sexual wellbeing in
transgender individuals is needed. For this, we propose to take an emic perspective, by studying what sexual wellbeing means for transgender individuals and combining this knowledge with a more general theoretical framework of the concept of sexual wellbeing, which has yet to be developed further as well. Furthermore, development of a comprehensive tool for measuring sexual wellbeing in transgender individuals is also much needed.”
Holmberg, et al., 2019 report that “In general, evidence suggests that medical treatment improves most dimensions of sexual function in transgender men and women who have undergone gender affirming treatment. Whether this improvement results in a satisfying sexual life is less certain. Research into
this topic is subject to numerous methodological disparities and, therefore, results should be interpreted with caution. Many studies in transgender persons show better results in sexual variables than among cisgender persons, indicating that there might be a tendency to overestimate results, probably due to selection biases. In addition, many transgender persons report that they do not engage in sex at all after gender- affirming treatment. Historically, transgender persons have been viewed as being hyposexual. However, this situation is not the case and it raises the question of whether low sexual activity might be a result of insufficient care or the transgender experience itself — all humans need to develop a healthy relationship with their own body during childhood, a process that can be severely hampered by the presence of gender dysphoria.”
Whitney, et al., 2022 report in The Journal of Medicine that “As the definition of health has grown to include sexual function, the responsibility of the physician has evolved to include the treatment of sexual dysfunction as well. Without the imminent establishment of a scientific definition of sexual function with an accompanying measurement tool, this lack of understanding continues a precedent that may further stigmatize and distance this population from healthcare. Although this challenge may seem daunting, it should be noted that this has been accomplished for both cis-gender heterosexual men and women. This failure to scrupulously address the needs of the TGNB community directly contradicts the medical profession’s revered values of equity and compassion. This branch of sexual medicine and gender-affirming care is critical for maximizing the quality of life as well as equity of the TGNB community to their cis-gender, heteronormative counterparts.”
(References to be added)
>> (Chapter 21) What research has investigated connections between exposure to endocrine disruptors (EDCs, including DES) and transgender/gender variations in humans?
Overview: Ian Cameron
From: Early Female Transgender Identity after Prenatal Exposure to Diethylstilbestrol: Report from a French National Diethylstilbestrol (DES) Cohort. Gaspari L, Kerlin S et al. 2024. Journal of Xenobiotics.
Diagnostic of transsexualism and gender incongruence are terms to describe individuals whose self-identity does not match their sex assignment at birth. A transgender woman is an individual assigned male at birth (AMAB) on the basis of the external or internal genitalia who identifies and lives as a woman. In recent decades, a significant increase in the number of transgender people has been reported. Although, its etiology is unknown, biological, anatomical, genetic, environmental and cultural factors have been suggested to contribute to gender variation.
In XY animals, it has been shown that environmental endocrine disruptors, through their anti-androgenic activity, induce a female identity. In this work, we described four XY individuals who were exposed in utero to the xenoestrogen diethylstilbesterol (DES) and were part of the French HHORAGES cohort. They all reported a female transgender identity starting from childhood and adolescence. This high prevalence of male to female transgenderism (1.58%) in our cohort of 253 DES sons suggests that exposure to chemicals with xenoestrogen activity during fetal life may affect the male sex identity and behaviour.
From: Recognizing, Evaluating, and Prioritizing the Fundamental Factors Influencing the Growing Prevalence of Transgender and Non-Binary Gender Identity in the Pediatric Population. Kerna N et al. 2024. European Journal Of Medical and Health Research.
This review observes the growing demographic of individuals identifying as transgender or non-binary, which currently represents approximately 1.3% (depending on the source) of the U.S. population. This population is shown to skew younger.
Environmental xenobiotics, particularly those containing endocrine-disrupting chemicals (EDCs), are scrutinized for their role in affecting hormonal regulation crucial for gender identity differentiation. The research also highlights how exposure to pharmaceuticals with endocrine-disrupting properties may induce atypical patterns in gender identity development, suggesting that a variety of exogenous elements could impact neuroendocrine sexual differentiation.
Medical disorders associated with altered androgen levels, such as congenital adrenal hyperplasia (CAH) and androgen insensitivity syndrome (AIS), are considered for their potential influence on gender identity from a biological perspective. Moreover, the role of diet and nutrition, particularly plant-based diets rich in phytoestrogens and conditions linked to obesity and metabolic syndrome, are explored for their effects on hormonal balance and, consequently, gender identity expression.
This review acknowledges the significant impact of media representation and societal norms on shaping attitudes concerning gender expression and identity.
The article points to psychological assessments and somatic markers as tools to explore prenatal hormone influences on gender identity, though emphasizing that they are not definitive. Furthermore, genetic and epigenetic findings offer a more in-depth understanding but lack diagnostic application. The identification and recognition of transgender and non-binary individuals continue to be self-determined processes that defy objective measurement by current medical standards.
From: Environmental contaminants, endocrine disruption, and transgender: Can “born that way” in some cases be toxicologically real? Holladay S et al. 2013. Human and Experimental Toxicology.
Gender is viewed by many as strictly binary based on a collection of body traits typical of a female or male phenotype, presence of a genotype that includes at least one copy of a Y chromosome, or ability to produce either egg or sperm cells. A growing non-binary view is that these descriptors, while compelling, may nonetheless fail to accurately capture an individual’s true gender. The position of the American Psychological Association (APA) agrees with this view and is that transgender people are a defendable and real part of the human population. The considerable diversity of transgender expression then argues against any unitary or simple explanations, however, prenatal hormone levels, genetic influences, and early and later life experiences have been suggested as playing roles in development of transgender identities. The present review considers existing and emerging toxicologic data that may also support an environmental chemical contribution to some transgender identities, and suggest the possibility of a growing nonbinary brain gender continuum in the human population.
Humans have synthesized multiple millions of tons of toxic chemicals and then distributed these onto the surface of the land, for control of insects, weeds and other life forms. Classes of these chemicals have included persistent organochlorines, mercury- and arsenic-based compounds, organophosphates, carbamates, pyrethroids, and diverse others. Some of these agents have been in existence for well over 100 years, for instance, the organochlorine insecticide dichlorodiphenyltrichloroethane (DDT) was first synthesized in 1884. In addition to being nearly colourless and odourless, and highly effective for killing insects, DDT also proved to be an endocrine disrupting compound, meaning it can interfere with natural hormones when it enters animal bodies. A well-known consequence of spraying large quantities of DDT into the environment for insect control was wildlife reproductive disturbance, including thinning of the eggshells of bald eagles and other carrion- and fish-eating birds. Such eggshell thinning activity of DDT has been verified by studies in domestic birds including chickens, and shown to be a consequence of disrupted prostaglandin synthesis in the uterus of the birds.
Insecticides and other chemicals like DDT wash from the land surface during rains and widely distribute via waterways. When surface soils become dry, applied chemicals are also subject to mobilization into the atmosphere with soil dusts, to be distributed by winds. The atmosphere then carries the land-applied chemicals to remote locations and redeposits them with rain or snowfall. In this manner, DDT and other pesticides and pollutants have become ubiquitously distributed, such that the entire globe is contaminated, with inhabitant life forms subject to a growing list of recognized hormone mimicking properties.
DDT would generally be detectable in human tissues as well, which is in fact the case. Furthermore, hormonal disruption by DDT has been linked to enhanced risk of disease in humans, for instance, higher levels of DDT associating with increased incidence of breast cancer in women. DDT, then, is only one of numerous chemicals typically detected in wildlife and humans during such analyses, with others including additional persistent organohalogen pesticides and non-pesticide.
A hypothesis was put forth in 1991, that widely distributed pesticides and related chemicals on the earth have the potential to subtly and broadly disrupt hormonal systems in wildlife. This hypothesis came to be known as the Endocrine-Disrupting Contaminants Hypothesis and has been proven valid by a significant body of scientific research. Observations in wildlife have included disruption of normal estrogenic, androgenic, brain neurochemical, thyroid, and other hormone activities by these environmental chemicals.
Such hormone-mimicking or inhibiting effects of pollutants have been documented in wildlife species that include land and sea mammals, fish, amphibians, reptiles, birds, and diverse invertebrates and have been found to include changes in sex differentiation before and after birth, intersex animals that show features of both sexes, sex reversal, altered sex ratios, skewed steroid production by gonads, altered penile density, reproductive impairment, altered thyroid function, behavioural changes, shifts in brain neuroendocrine hormones, changed brain synaptic density in steroid-sensitive nuclei, and other endocrine system-related changes.
The demonstration of pollutant-induced hormone disruption in diverse wildlife species raises important questions about possible similar effects these chemicals may be having in some members of the human population. A landmark textbook published in 1996, titled Our Stolen Future, addressed this concern by exploring ways environmental contaminants may be interfering with the hormonal control of development in both animals and humans.
It is well-recognized that post-pubertal human female and male bodies on average display sex hormone-driven differences that include average height and weight, percent body fat, proportionate muscle and bone mass, pelvis width and roundness of pelvic inlet, extent and distribution of body hair, size and development of the larynx, and thickness and collagen content of skin. Early years in neuroscience research similarly identified differences in the brain portion of the human body between females and males, and viewed these as largely limited to hypothalamic-related gonadal hormone effects that underlie dimorphic sex behaviours. More recent neuroscience research has demonstrated microanatomic and neurochemical brain differences by sex that influence brain function at multiple and diverse levels. These differences include regional neurotransmitter levels and cortical volumes, cortical neuron and synaptic density, enzymatic pathways, regional complexity of dendritic arbors and density of dendritic spines, and locally synthesized neurohormones not regulated by gonadal hormones.
Roles of maternal- and fetal-derived sex steroid hormones in brain feminization or masculinization have long been recognized. During gestation of mammals, a timed testosterone surge initiates masculinization of the developing brain, while absence of such a surge begins the pathway to a female brain that continues into the prepubertal period. These hormones profoundly affect sexual function and differentiation of neural circuits that control female and male behaviour. The past few generations of humans have seen a dramatic increase in environmental contaminants that possess hormone mimicking properties, which may suggest the possibility of subtle modulation of normal brain sex differentiation in some portion of the human population. These chemicals include the already-discussed ubiquitous DDT that is detectable in most humans, other high-production pesticides and herbicides, and plastics production molecules such as the highly-studied estrogenic and antiandrogenic bisphenols. Bisphenol A (BPA) in particular has been among the most heavily synthesized chemicals over the past 3 decades as use of plastics has increased, with annual production reaching millions of tons. Because of growing endocrine disrupting concerns, BPA is more recently being replaced by other bisphenols in plastics production including bisphenol S and bisphenol F, for which there is less available toxicity data.
The number of environmental contaminants like DDT and BPA that have achieved ubiquitous ranking has again been growing over the past few generations, meaning increasing numbers of global contaminates. Human-introduced chemicals now considered as ubiquitous include (this list is not exhaustive) numerous pesticides and herbicides used in agriculture, different classes of flame retardants including per- and polyfluoroalkyl agents (PFAS), pharmaceutical personal care products (PPCP) including birth control pills that generate large quantities of urine-carried hormones and hormonal metabolites in waste waters, solvents such as trichloroethylene used industrially for degreasing machine parts and for dry cleaning of clothing, plastics and microplastics, toxic metals that have recently come to include lithium from increased use of lithium batteries, and vast quantities of the already-mentioned plasticizers. Of growing concern, many of these chemical contaminants that have achieved global environmental distribution have been found to possess endocrine modulating activity in animals and humans, and in humans have been linked to disrupted endocrine signaling, altered reproductive rhythms, reduced male fertility, neurologic damage, increased risk of autism, ADHD and learning disorders, reduced IQ and additional effects that are in part believed to derive from changes in brain development.
Counselors and therapists have identified societal and environmental contributions to sexual identities including transgender identity, which may occur over varying numbers of years after the birth of a person. Among these for some transgender individuals are adverse childhood events including the experiencing of childhood sexual abuse from siblings or adult family or non-family members. For studies of a genetic component of same sex orientation (SSO) in humans, identical twin studies have been widely used and have shown high levels of twin non-concordance (meaning, the identical twin of a SSO person in most cases does not identify as SSO themselves). This co-presence of identical DNA with opposite self-identified sexual orientations in the majority of twin pairs has been viewed as compelling evidence that the DNA base pair sequence does not include coding for SSO genes.
As with SSO, identical twin studies have found a high level of non-concordance for transgender identity, with 80% of transgender twins having a non-transgender twin counterpart. This outcome provides additional evidence that factors outside the DNA base pair sequence underlie development of some transgender identities, and might be used to argue that “born transgender” is an inaccurate conclusion. Newer data, however, suggest the possibility of a DNA-related developmental basis for some transgender identities, and imply that science-based calls to abandon the potential reality of being born transgender may be premature.
Epigenetic changes including DNA methylation and histone modification are part of normal fetal and early postnatal programming and development, including fetal neuro-hormonal regulation for establishing typical patterns of differential brain development between females and males. Alterations in normal epigenetic control of fetal brain development have been linked to neurologic, psychiatric, and developmental disorders, suggesting importance of normal occurrence of these modifications. Gonadal hormone-driven epigenetic modification differences in brain development have also been shown to have regulatory roles in sexual differentiation of the brain. A growing number of environmental chemicals, including the already described DDT, BPA and DEHP, have become recognized for ability to cause epigenetic modifications that include histone modification, DNA methylation, and expression of non-coding RNAs.
re-birth epigenetic modifications of DNA have been related to fetal androgen signaling patterns regulating brain sex development. Specifically, these authors showed decreased androgen sensitivity in human XX fetuses and increased androgen sensitivity in XY fetuses as a consequence of epigenetic modifications. Such fetal androgen signaling strongly influences brain sex development, which led the authors to hypothesize that inappropriate epigenetic modifications can masculinize the brains of human females during fetal development, and feminize the brains of developing males.
Brain development can be changed through additional pathways that may be subject to modulation by environmental chemicals. The microglia are an immune cell type located throughout the brain and spinal cord, that regionally account for 5-15% of brain cells. During development, these cells play critical roles in synaptic organization, or “wiring” of the brain. This brain organization is different by sex (female vs. male) in steroid-sensitive regions that are responsible for sociosexual and mood-related behaviours, suggesting potential for vulnerability to endocrine disruption.
Contamination of the environment with such chemicals has been associated with hormone-related changes in diverse wildlife species, particularly when the exposures occurred during sensitive stages of development. A natural concern is that some of the humans, both cis- and transgender, who coinhabit a globally-contaminated planet may also be subtly affected, including in the development of steroid-sensitive brain regions that regulate brain sex establishment.
Clearly, transgender humans long predate modern endocrine disrupting environmental chemicals and have throughout history been a portion of the human population. In a world that has gained ubiquitous contamination with endocrine disrupting chemicals, an environmental component to some human phenotypic males (humans born with male genitalia and other typical male physical traits) who are also genotypically male (possess XY chromosomes), but whose brains strongly assure them they are female (transgender) may be supported by the chemical and animal data reviewed in this report. The same is of course true for some transgender individuals who phenotypically and genotypically present as female, but whose brains tell them they are male.
Regarding transgender, the available literature supports the possibility that non-genetic but DNA-carried, environmentally-induced epigenetic modifications, in some individuals, may influence adulthood gender identities. Based on this growing database, the possibility should not be dismissed that some humans can be born with brain microanatomic and neurochemical architecture that underlies identifying as the sex trans to their body phenotype and genotype. The recognizing of scientific support for this possibility may be of value to humans who very strongly perceive their gender identity to be a hard-wired reality present since time of birth (i.e., “born that way”), rather than a choice made by them. The position of gender binary (only 2 genders, female or male) is then strongly supported by human macroscopic anatomic phenotypes and the typical XX or XY genomes (these being the factors most commonly used to deny the reality of transgender people). However, data surveyed in this review also lend support to the possibility of some level of a nonbinary brain gender continuum in the human population due to ubiquitous endocrine modulating environmental chemicals. A relevant question then becomes, when designating individuals as female or male, which basis may be more appropriate; body phenotype and genotype, or brain microanatomy and neurochemistry?
From: Gender Identity and Sexual Orientation Identity in Women and Men Prenatally Exposed to Diethylstilbestrol. Troisi R et al. 2020. Archives of Sexual behaviour.
The associations of prenatal diethylstilbestrol (DES) exposure, a potent oestrogen, with sexual orientation and gender identity in 3306 women and 1848 men who participated in a study of prenatal DES exposure were assessed. Odds ratios (OR) and 95% confidence intervals (CI) were derived from logistic regression models adjusted for birth year, study cohort, and education. Among women, the OR for DES in relation to reporting sexual orientation identity as nonheterosexual was 0.61 (95% CI 0.40–0.92) primarily due to a strong inverse association with a lesbian identity (OR 0.44, 95% CI 0.25–0.76). Among men, the OR for DES in relation to reporting a nonheterosexual sexual orientation identity was 1.4 (95% CI 0.82–2.4), and ORs were similar for having a gay identity (1.4, 95% CI 0.72–2.85) and bisexual identity (1.4, 95% CI 0.57–3.5). Only five individuals reported a gender identity not conforming to that assigned at birth, preventing meaningful analysis. Women who were prenatally exposed to DES were less likely to have a lesbian or bisexual orientation, while DES-exposed men were somewhat more likely to report being gay or bisexual, but estimates were imprecise.
Research on the biological foundations of sexual orientation, an enduring pattern of emotional, romantic, and/or sexual attractions to men, women, or both sexes (American Psychological Association) supports roles for genetics, epigenetics, and prenatal hormonal exposure, in particular testosterone (Berenbaum & Beltz; Hines; Fisher, Ristori, Morelli, & Maggi). The origins of gender identity, a person’s concept of self as female, male, or other, may be more complex regarding the relative contributions of social and biological influences and the role of early testosterone exposure (Berenbaum & Beltz; Hines).
Direct data in humans on sexual orientation are based on studies of rare conditions associated with an altered hormonal milieu in utero. The use of diethylstilbestrol, a synthetic nonsteroidal oestrogen, during pregnancy, provides another test of the influence of prenatal hormonal exposure on sexual orientation. Based on the animal paradigm and human evidence indicating that prenatal testosterone exposure influences male-type development, DES could influence nonheterosexual orientation in women by increasing testosterone production, a phenomenon that has been observed in female mice exposed in utero to DES (Haney et al). Alternatively, rapid metabolism of testosterone to estradiol in normal human pregnancy may protect the female fetus from androgen effects. In males, high doses of DES could affect nonheterosexual orientation by decreasing testosterone production and/or androgen receptor expression.
The NCI combined cohorts of women and men represent one of the only human studies allowing evaluation of the influence of a potent synthetic oestrogen on early fetal development in a population with documented DES exposure status. Brain organization that occurs in the prenatal period may influence an individual’s sexual and gender identities, with one hypothesis that variance in exposure to gonadal hormones may mediate this influence, along with genes and maternal factors (Fisher et al; Roselli), including maternal immune response (Bogaert et al).
We found that women exposed in utero to DES were significantly less likely to report being gay/lesbian, but DES exposure was not associated with bisexuality. The association with gay/lesbian orientation was strongest for exposure to a low cumulative dose of DES. We observed no consistent patterns of association between timing of first gestational DES exposure and sexual orientation identity among exposed women. The current results agree with those from our earlier study (Titus-Ernstoff et al), which indicated that prenatally DES-exposed women were slightly more likely than unexposed women to have ever married and were less likely to report sexual partners of the same sex.
In contrast to the findings for women, DES-exposed men were more likely to report being gay or bisexual; however, this estimate was imprecise likely owing to the men’s cohort being smaller than the women’s cohort. The findings in men agree with our previous study of sexual partners, in which the OR was elevated for same-sex partners, but confidence limits included 1.0 (Titus-Ernstoff et al). In one earlier report on prenatal DES exposure, exposed men were less likely than unexposed men to be married or living as married (Beral & Colwell), while two larger studies, including an analysis of 494 men in the Dieckmann randomized trial cohort, found no significant association between DES and ever having been married (Vessey, Fairweather, Norman-Smith, & Buckley; Wilcox, Baird, Weinberg, Hornsby, & Herbst). Taken together, our findings for the relation between prenatal DES exposure and sexual orientation identity in women and men are consistent with DES not acting as a masculinizing agent.
In summary, the findings showed that women who were prenatally exposed to DES were significantly less likely to report being lesbian or bisexual. In contrast, while men who were prenatally exposed to DES were somewhat more likely to report being gay or bisexual, the estimate was very imprecise and compatible with chance. Finally, very few individuals reported currently thinking of themselves as a gender different from that assigned at birth in either the exposed or unexposed group.
From: Transgender Associations and Possible Etiology: A Literature Review. Saleem F and Rizvi S. 2017. Cureus.
Transgender or gender dysphoria has been defined in the fifth edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM-5), as distress resulting from the incongruence between one’s experienced gender and one’s assigned gender, along with a persistent and strong desire to be of another gender, and accompanied by clinically significant distress. Adolescents referred for evaluation often want hormonal therapy and several among them also express a desire for gender reassignment surgery. Furthermore, evidence shows that adolescents and adults with gender dysphoria without a sex development disorder, before gender reassignments, are at increased risk for suicide. For this review, a search of the English language scientific literature was conducted using the PubMed database. This summary discusses the associations and comorbidities of gender dysphoria and reiterates the evidence that its etiology is multifactorial. Transsexualism involves prenatal neuroanatomical changes, has a psychiatric association, and is found to be more prevalent in conjunction with schizophrenia and autism spectrum disorders. Childhood adversities and neglect are also linked to having a transgender identity. Moreover, the evidence favours a genetic predisposition. Likewise, there seems to be a growing concern with regards to the relationship between endocrine disruptors and transsexuals as well as other gender minority populations. More research needs to be done to understand the exact pathways.
Transgender or gender dysphoria (GD) has been defined as clinically significant distress resulting from the incongruence between one’s experienced gender, and one’s assigned gender, along with a persistent and strong desire to be of another gender. Adolescents referred for evaluation often request hormone therapy (HT) and many also express a desire for sex reassignment surgery (SRS). Evidence shows that adolescents and adults with GD without a sex development disorder before SRS are at increased risk for suicide. However, after SRS, the adjustment may vary, and suicide risk may persist. GD has replaced the term gender identity disorder (GID) in the 2013 edition of the diagnostic and statistical manual of mental disorders, fifth edition (DSM-5), which itself has replaced “transsexualism”.
The transgender community suffers from a lot of discrimination. In a survey in the United States, 19% of transgender people reported being denied medical care. Nearly half of those surveyed reported having to teach their medical providers how to care for the transgender persons [3]. It is imperative to perform more research regarding transgender status and associations in order to reveal the complex multifactorial etiology, improve the understanding among clinicians, and lead to better wellbeing for transgender individuals. GD involves neurodevelopmental changes and has psychiatric association including schizophrenia and autism. Childhood adversities are also associated with being transgender. Moreover, the evidence favours a genetic predisposition. A link with endocrine disrupting chemicals has also been suggested.
There are several transgender variants that exist historically in different cultures of the world. They do not fit in the conventional definition of male or female; rather, they move between the two or are a combination of both genders. Vulnerable and insecure transgender individuals have been disregarded and marginalized by the mainstream society.
Differences in the brain structures and brain functions that are related to gender and sexual orientation have been found to be associated with the pathoetiology of gender dysmorphic disorder. Sexual differentiation of the genitals takes places in the first trimester of pregnancy, and sexual differentiation of the brain starts during the second half of pregnancy. Therefore, it has been hypothesized that these two processes may play roles independently of each other that predispose an individual to transsexuality. One working hypothesis behind GD is that the neuronal differentiation in the hypothalamic networks is altered. Magnetic resonance imaging (MRI) of male-to-female transsexual conversion has shown a female-like putamen; this means that the transgender putamen has a volume that is larger than normal males but within the normal female range. Combined positron emission tomography and MRI experiments have shown sexual dimorphism in hemispheric ratios and the pattern of amygdala connectivity. Sex reversal of the INAH3, a subnucleus of the hypothalamic uncinate nucleus in transsexual people, is a probable marker of an early atypical sexual differentiation of the brain. Changes in INAH3 and the bed nucleus of the stria terminalis (BNST) may belong to a complex network that may structurally and functionally be related to normal sex differentiation.
Autism spectrum disorder (ASD) is more prevalent in GD than in the general population. Evidence suggests a link between GD and ASD. To study further, additional studies with larger sample size are needed. Evidence shows that 5.5% of the GD patients showed ASD traits as compared to the general population. The literature evidence as regards to the co-occurrence of ASD and GD is limited. This is important as paying attention to the development of gender identity formation in individuals with ASD from an early age may be helpful. Doctors should also help individual to explore his or her own gender narrative, rather than merely focusing on medical intervention.
A growing body of evidence reports the association between childhood maltreatment and adult dissociative psychopathology. In a study performed in Florence, 109 patients meeting the criteria for male-to-female GD were interviewed for childhood maltreatment with regards to emotional abuse, neglect, physical abuse, and sexual abuse. A high proportion of transsexual subjects reported childhood maltreatment. Maltreated subjects also reported higher body dissatisfaction and showed a worse lifetime mental health. Nevertheless, approaching the issue of childhood neglect and maltreatment thoroughly can enable the patients to reflect on its impact on their lives and, eventually, its relevance on treatment decisions.
Another working hypothesis involves the role of endocrine disruptors in transgender etiology. In a letter to the editor, Bejerot, et al. suggested a hypothetical link between endocrine disrupting chemicals and transgenders. They hypothesized a role for endocrine disruptors, especially phthalates. Phthalates are present in some plastics, and there has been an increased concentration in the environment in recent years. Bejerot, et al. suggested that endocrine disruptors may be the cause of high fetal testosterone exposure leading to increased risk of ASD as well as GD. More systematic investigations are required that may also elaborate mechanisms involved in brain development and sexual differentiation.
Likewise, a genetic association has been proposed. Heritability of GD is suggested by evidence that has shown the familiality of transsexualism among non-twin siblings, and an increased concordance for transsexualism in monozygotic as compared with dizygotic same-sex twins [1]. In addition, research supports CYP17 as a candidate gene for female-to-male transsexualism and shows that loss of a female-specific CYP17 T-34C allele distribution pattern is linked with female-to-male transsexualism.
The literature on transgender people during the last decade provides a framework for the associations and comorbidities associated with transgender or GD. The research draws links between transgender people and changes in prenatal neuroanatomy. There is an association with psychiatric disorders, schizophrenia, and ASD. Transsexualism is linked to childhood maltreatment and adversities. Evidence also leads some to speculate that there are genetic predispositions. Furthermore, a working hypothesis exists with regards to possible association of endocrine disrupting chemicals and transgender identity or other gender-related issues. The evidence until today shows that transsexualism has a complex biopsychosocial etiology. There is a need for additional research to explore the myths and mysteries behind transgender identity to improve the understanding among clinicians, social activists and policy makers leading to better transgender health.
From: Are EDCs Blurring Issues of Gender? Hood E. 2005. Environmental Health Perspectives.
Although scientists have postulated a wide range of adverse human health effects of exposure to endocrine-disrupting chemicals (EDCs), the nexus of the debate is the concern that prenatal and childhood exposure to EDCs may be responsible for a variety of abnormalities in human sexuality, gender development and behaviours, reproductive capabilities, and sex ratios. Scientists today are asking hard questions about potential human effects: Do EDC exposures impair fertility in men or women? Can they cause sexual organ malformations, stunted reproductive development, or testicular or breast cancer? Do fetal exposures to EDCs alter sex phenotypes? Do they change later gender-related neurobiological characteristics and behaviours such as play activity and spatial ability? Could such exposures even be involved in the etiology of children born with ambiguous gender?
In many well-documented cases of high-level fetal exposures to known EDCs such as DES, certain PCBs, and DDT, the answer to the question of whether exposure is associated with gender-related effects is clearly yes. he endocrine system, comprising the hypothalamus, pituitary, testes, ovaries, thyroid, adrenals, and pancreas, is one of the body’s key communications networks. It regulates the function of specific tissues and organs by secreting hormones that act as precise chemical messengers. Development and regulation of the reproductive system is one of the major functions of the endocrine system.
Sex determination and development begin early in gestation, with the differentiation of the embryonic gonad into either testes or ovaries. If the Sry gene is present on the Y chromosome, it will, when activated, trigger a complex cascade of hormonal events that ultimately results in the birth of a baby boy with all of the requisite male equipment in place and functioning properly. In the absence of the Sry gene, the end product of the process will be a baby girl. The female phenotype is considered to be the “default” pathway for mammalian reproductive development.
Differentiation and development of the sexual organs continues throughout gestation under the guidance of the various sex hormones (such as estrogen and testosterone) produced by the endocrine system. For males and females alike, the entire process of reproductive development is exquisitely sensitive to minute changes in levels of the sex hormones, particularly during certain critical windows of development.
Such a delicately timed and precisely controlled process presents a myriad of opportunities for perturbation from exposure to EDCs. These chemicals mimic hormones, and can disrupt differentiation and development in a wide variety of ways, by duplicating, exaggerating, blocking, or altering hormonal responses. The developing fetus and early neonate may lack the protective metabolic mechanisms present in adults that help detoxify and break down chemicals, maintaining homeostasis in the system. Also, tissues are rapidly dividing and differentiating in the fetus, and such a high level of cell activity is vulnerable to disruption of normal development. With such small body mass in the fetus and child compared to an adult, exposure levels may be amplified in terms of relative dosages reaching target tissues. And sometimes, exogenous EDCs may show very low binding to plasma hormone-binding proteins and thus roam the body in an unbound state, with unknown effects.
Reproductive and developmental abnormalities linked to EDC exposures have now been documented in birds, frogs, seals, polar bears, marine mollusks, and dozens of other wildlife species. For example, alligators in Lake Apopka—one of Florida’s most polluted lakes due to extensive farming activities around the lake, the presence of a sewage treatment facility, and a major 1980 spill of pesticides including DDT and DDE—have been shown to have been “feminized.” That is, zoologist Louis J. Guillette, Jr., and colleagues first reported in the August 1994 EHP, the males have shortened penises and low levels of testosterone, while the females have excessive levels of estrogens. Sex reversal (in which an animal of one sex matures with the reproductive organs and capabilities of the other sex) and skewed sex ratios (in which there is an unusually greater proportion of one sex than the other) have been seen in several fish populations, particularly colonies living in close proximity to pulp and paper mills and sewage treatment plants. Other reports have shown reproductive effects among wildlife resulting from exposure to EDCs excreted into the water supply by women taking birth control pills.
According to a report on EDCs published in volume 75, issue 11/12 (2003) of Pure and Applied Chemistry by the Scientific Committee on Problems of the Environment/International Union of Pure and Applied Chemistry (SCOPE/IUPAC), more than 200 animal species are either known or suspected to have been affected by these chemicals. “The weight of evidence for endocrine disruption in wildlife is really overwhelming,” says Joanna Burger, a professor of cell biology and neuroscience at Rutgers University who cochaired the SCOPE/IUPAC project.
The report further notes, however, that “[c]hemical interferences with steroid biosynthesis and metabolism can produce adverse health effects, even though the inducing agent would not be detected as an [EDC] using receptor-based test systems. This is an important area of study because some examples of [endocrine disruption] occurring in animals derive from exposure to inhibitors of steroidogenic enzymes such as 5α-reductase and aromatase.
The DES situation could be seen as a worst-case scenario for prenatal EDC exposure—the deliberate delivery of a potent estrogenic chemical in high doses. Viewed another way, it has provided researchers a rare opportunity to study the effects of prenatal EDC exposure in a relatively controlled fashion, with a well-defined population and well-characterized exposure to a single potent agent.
It’s premature to call it a theory; at this point, it barely qualifies as a hypothesis: some observers are putting forth the proposition that prenatal EDC exposures may affect gender identity—how a person identifies him- or herself, regardless of physical characteristics. This idea presupposes two basic concepts: first, that transgenderism (in which a person experiences “gender dysphoria,” a strong feeling of having been born the wrong sex) is physiological in origin, most likely due to events during prenatal neurological development; second, that intrauterine EDC exposures can and do disrupt prenatal neurological development.
Scott Kerlin is a Ph.D. social scientist at the University of British Columbia. He devotes considerable time to monitoring the international scientific literature on DES and other EDCs as well as to researching and writing about the long-term health effects of pre-natal DES exposure on males. He is himself the son of a woman given DES in pregnancy.
Kerlin recently conducted a survey study of 500 members of the DES Sons International Network, an online resource for men who know or strongly suspect they were exposed to DES in utero. In a paper presented in August 2005 at the International Behavioural Development Symposium in Minot, North Dakota, he reports that more than 150 respondents identified themselves as having any of a variety of gender-related disorders. Kerlin does not claim that DES causes these gender disorders, but feels that his results indicate that such outcomes should be included in research related to the potential effects of prenatal EDC exposures.
It’s going to be very difficult to ever conclusively answer the basic question of whether low-level EDC exposures during development are causing deleterious reproductive or gender-related outcomes in humans. Scientists agree that one of the major challenges is to address the issue of mixtures. Typically, researchers look at the impact of one chemical at a time, but environmental exposures regularly involve an unpredictable mix of chemicals, with exposures varying widely in dose and duration. It is unlikely there will ever be a comprehensive understanding of how the many EDCs in mixtures interact with each other and with human physiology.
From: Prenatal exposure to diethylstilbestrol (des) in males and gender-related disorders: results from a 5-year study. Kerlin S. 2005. Researchgate.
For many years, researchers and public health specialists have been assessing the human health impact of prenatal exposure to the estrogenic anti-miscarriage drug, diethylstilbestrol (commonly known as DES or “stilbestrol”). The scope of adverse effects in females exposed to DES (often called “DES daughters”) has been more substantially documented than the effects in males (“DES sons”). This paper contributes three areas of important research on DES exposure in males: (1) an overview of published literature discussing the confirmed and suspected adverse effects of prenatal exposure in DES sons; (2) preliminary results from a 5-year online study of DES sons involving 500 individuals with confirmed (60% of sample) and suspected prenatal DES exposure; (3) documentation of the presence of gender identity disorders and male-to-female transsexualism reported by more than 100 participants in the study.
During the 1970s and 1980s an increased amount of public and scientific attention was paid to the health and medical problems of individuals whose mothers were prescribed diethylstilbestrol (DES). A potent synthetic nonsteroidal estrogen, DES was first developed in1938 and initially became available in the U.S. for treating a range of gynecologic conditions in1941 (Apfel and Fisher, 1984). A few years later its approval by the FDA was broadened to include treatment of pregnant women for the purpose of preventing miscarriages. Though its efficacy had long been questioned by some in the medical community (Bambigboye and Morris,2003; Dieckmann, 1953), DES remained popular with doctors until discovery in the early 1970s of an apparent association between prenatal exposure to DES and a rare form of vaginal cancer in females whose mothers used DES (Heinonen, 1973; Herbst and Bern, 1981).Subsequent research confirmed the transplacental mechanism of DES transmission (Maydl, et al., 1983) and classified DES as a carcinogen and teratogen (Mittendorf, 1995) as well as a mutagen (Roy and Liehr, 1999; Stopper et al., 2005).
While DES usage with pregnant women was banned by the FDA in 1971, the drug continued to be used in several European countries into the early 1980s (Schrager and Potter, 2004). DES remained a popular option for treatment of advanced prostate cancer in aging males due to its ability to inhibit luteinizing hormone secretion by the pituitary and thus inhibit testosterone secretion (Scherr and Pitts, 2003; Whitesel, 2003), despite reports that adverse effects from this treatment could include feminization in males (B. C. Cancer Agency, 2005). Through the 1970s DES was also prescribed as an estrogen supplement for treatment of male-to-female transsexuals (Kwan, 1985; Ober, 1976).
It has been estimated that as many as four to five million American women were prescribed DES during pregnancy. Estimates of the numbers of “DES daughters” and “DES sons” born in the U.S. are between one million and three million each (Edelman, 1986). Hundreds of thousands of DES sons and daughters were also born in Canada, Europe and Australia between the 1940s and 1980s. Efforts to determine exact numbers of prenatally exposed individuals, and the dosage and exposure patterns, particularly during the years of prime DES popularity, 1947-55 in the U.S., have been largely unsuccessful (Duke, et al., 2000; Heinonen, 1973). Because DES proved popular as a growth-stimulant in the cattle industry (Raun and Preston, 2002) for more than forty years (McLachlan, 2001), many consumers have also been exposed to unknown amounts of DES as it entered the food chain through beef consumption.
Following the FDA restrictions on DES prescriptions in the U.S. in 1971, researchers began to document a range of confirmed and suspected adverse effects of prenatal DES exposure in females and males (Edelman, 1986). Compared with the volume of published research on adverse effects in DES daughters, however, relatively few primary studies of DES sons have been published. The scope of known and suspected health effects among DES sons discussed in literature published since the 1950s includes (1) reproductive tract abnormalities; (2) infertility; (3) testicular cancer; (4) prostatic hyperplasia and cancer; (5) psychosexual effects; (6) psychiatric effects; and (7) effects on hemispheric laterality and spatial ability (Giusti et al., 1995; Pillard, et al., 1993; Reinisch and Sanders, 1992; Verdoux 2004.
4In 1959, a single case study of pseudohermaphrodism in a male with prenatal DES exposure was reported (Kaplan, 1959). Reports of urogenital abnormalities in DES sons first appeared inthe medical literature during the 1970s (Andonian and Kessler, 1979; Bibbo et al., 1977;Cosgrove et al., 1977; Gill et al., 1979; Gill, et al., 1988; Henderson et al., 1976), consistent with results of experiments with prenatal DES exposure in male mice reported by McLachlan etal. (1975) and Newbold et al. (1987). These effects include epididymal (benign) cysts, hypoplastic or undescended testes (chryptorchidism), microphallus or underdeveloped penis, and hypospadias. Using data from DES sons participating in the DES cohort studies funded bythe National Cancer Institute (NCI), researchers have examined possible links between prenatal DES exposure and greater risk of male infertility but have reached inconclusive findings (Wilcox et al., 1995). Although heightened testicular cancer risk has long been associated with prenatal DES exposure in males, researchers using the NCI cohorts to track cancer outcomes among DES sons claim to have measured no statistically significant increases in testicular or other forms of cancer (Strohsnitter, et al. 2001).
John McLachlan (2001), a pioneering DES researcher whose studies have assessed the effects of DES exposure in laboratory animals and mechanisms of DES toxicity for the past three decades, was among the first researchers to classify DES within a broader family of chemical compounds called “environmental estrogens”, “xenoestrogens”, or “endocrine disrupting chemicals” because of their common ability to mimic and interfere with normal hormonal processes associated with reproductive development.
5several environmental xenoestrogens play a role unless exposures are extremely high(which is not expected), the dose–response relation is U-shaped or mixtures of xenoestrogens have synergistic actions. Low exposure levels for xenoestrogens may, however, operate by means of other toxicological mechanisms (Storgaard, et al.,2005).It has been hypothesized that prenatal DES exposure may also have led to behavioural effects in humans (Meyer-Bahlburg and Erhardt, 1986; Meyer-Bahlburg, et al., 1995). Primary studies exploring possible behavioural and psychiatric effects of prenatal DES exposure in males first appeared in the literature during the 1970s. DES exposure has been associated with increased potential for major depressive disorders and other psychiatric effects in males (Katz,et al., 1987; Meyer-Bahlburg et al., 1985; Pillard et al., 1993; Saunders, 1988; Vessey et al.,1983). Recent discussions of potential psychiatric effects of prenatal DES exposure, including gender-related effects and schizophrenia, have been presented by Verdoux (2000; 2004) and Boog (2004).
Among the possible effects associated with prenatal DES exposure that have been discussed in the literature is impact on psychosexual development (Giusti et al., 1995). Research investigating possible psychosexual impact in human males was first published in the 1970s(Yalom, Green, and Fisk, 1973). Studies by Kester et al. (1980), Reinisch and Sanders (1984;1992) and Reinisch, et al., (1991) attempted to assess various dimensions of “masculine” and “feminine” behaviour and spatial ability among DES sons. In their meta-analysis of 19 studies on the behavioural effects of prenatal exposure to hormones administered for the treatment of at-risk human pregnancy (including the Yalom et al., 1973 and Kester et al., 1980 studies of-DES exposed males), Reinisch et al. (1991) concluded:
The data on prenatal exposure to synthetic oestrogen derive primarily from subjects exposed to diethylstilbestrol (DES). DES-exposed male subjects appeared to be feminized and/or demasculinized, and there is some evidence that DES-exposed female subjects were masculinized.
In July 1999, the U.S. National Cancer Institute, National Institute of Environmental Health Sciences, Office of Research on Women’s Health and the Centers for Disease Control jointly sponsored a two-day conference, “DES Research Update 1999: Current Knowledge, Future Directions” (NCI, 1999). The event brought together leading DES research scientists, public health specialists, and DES-exposed advocacy group representatives for an evaluation of what was known and what still needed further investigation in the realm of human health effects of DES exposure. Among the notable conclusions of this conference was that DES sons had been insufficiently studied, and that more studies were needed to document the full range of adverse health consequences in DES sons.
The revelation in the early 1970s of heightened cancer risk among DES daughters led to a public advocacy movement among DES daughters and their mothers for increased research on DES and women’s reproductive health concerns along with greater accountability among the drug companies (Seaman, 2003). However, DES sons have historically remained relatively isolated from one another and their health concerns have been largely unknown to the public. Among the activities of the DES Sons International Network was to document the most common patterns by which DES sons learned of their prenatal exposure. Researchers had long recognized that among DES daughters, the most common form of notification regarding DES exposure was from mothers (Apfel and Fischer, 1984; Seaman, 2003). Less has been known about communications and relationships between DES sons and their mothers although it is believed that lower percentages of DES sons than DES daughters have been informed of their exposure (NCI, 1999).
Core Health Concerns of DES Sons:
Based on preliminary analysis of critical health issues reported by individual DES sons in the network, the three topics most frequently listed among the sample of 500 individuals with confirmed or suspected prenatal DES exposure are (a) gender identity concerns (at least 150 reports); (b) psychological/mental health issues, especially depression and anxiety disorders (at least 100 reports); and (c) hormonal/endocrine health issues (at least 75 reports)
Additional Reported Adverse Health Effects:
Though identified less frequently in overall health reports provided by study participants, several participants listed histories of infertility, reproductive tract abnormalities (including reports of ambiguous or underdeveloped genitalia), epididymal cysts, cryptorchidism, hypospadias, gynecomastia, and erectile dysfunction. Statistics on the full extent of reporting of these concerns are still undergoing analysis.
Prevalence of Male-to-Female Transsexual, Transgender, and Intersex Individuals More than 150 network members with “confirmed” or “strongly suspected” prenatal DES exposure identified as either “transsexual, pre- or post-operative,” (90 members), “transgender” (48 members), “gender dysphoric” (17 members), or “intersex” (3 members). These statistics are taken from self-report terms provided by individual participants in their health histories.
Among the most significant findings from this study is the high prevalence of individuals with confirmed or strongly suspected prenatal DES exposure who self-identify as male-to female transsexual or transgender, and individuals who have reported experiencing difficulties with gender dysphoria.
In this study, more than 150 individuals with confirmed or suspected prenatal DES exposure reported moderate to severe feelings of gender dysphoria across the lifespan. For most, these feelings had apparently been present since early childhood. The prevalence of a significant number of self-identified male-to-female transsexuals and transgendered individuals as well as some individuals who identify as intersex, androgynous, gay or bisexual males has inspired fresh investigation of historic theories about a possible biological/endocrine basis for psychosexual development in humans, including sexual orientation, core gender identity, and sexual identity (Benjamin, 1973; Cohen-Kettenis and Gooren, 1999; Diamond, 1965, 1996; Michel et al, 2001; Swaab, 2004).
Mental health and psychiatric issues (including depression and anxiety disorders) are relatively significant among the population of DES sons participating in this research.
Endocrine system disorders such as hypogonadotropic hypogonadism in DES sons have been among the more common reported adverse health effects in this research study. Although the prevalence of endocrine system disorders among DES sons has not been discussed in any of the existing published epidemiological research on DES-exposed populations, both the Endocrine Society and the American Association of Clinical Endocrinologists (2002) have recognized prenatal DES exposure as a risk factor for endocrine disorders including hypogonadism. This study confirms that this issue needs further attention in future studies of DES sons.
The term “gender-bending chemicals” has become relatively popular with the news media in their latest reports on the toxic effects of endocrine disrupting chemicals such as phthalates on male reproductive development (Sample, 2005; Swan et al., 2005). Scarcely more than a decade ago, the concept was almost unheard of. Its introduction into early news stories describing documented and suspected but unconfirmed effects of endocrine disrupting chemicals (EDCs) no doubt provoked both amusement and angst in the public imagination (see “Gender-Bending Pollution”, 1995). By the time the World Health Organization’s International Programme on Chemical Safety had released its “Global Assessment of the State-of-the Science of Endocrine Disruptors” (IPCS, 2002), the story of DES had become part of the story of an entire group of environmentally-present toxic chemicals thought capable of creating a variety of reproductive abnormalities in humans as well as animal populations (“Alarm at Gender-Bending Chemicals”, 2002). In that same year, Dutch researchers studying male and female children’s play behaviour documented apparent “feminizing” effects in boys resulting from perinatal exposure to PCBs and dioxins (Vreugdenhil, et al., 2002). Undoubtedly, the issue of endocrine disruption and potential impact on gender identity and sexual development is an issue that merits wider investigation in the future (Johnson, 2004).
If the results of this current study have pointed out anything significant, it is that we cannot relegate DES to the dustbin of “cancer-causing drugs no longer being used and therefore unworthy of continued investigation.” And we cannot afford to limit the scope of our vigilance and public health information regarding long term effects of DES to cancer outcomes (Schrager and Potter, 2004).
Key Literature References
(Notable) *** Gender Identity Disorders: A Legacy of Fetal Exposition to Diethylstilbestrol, an Endocrine Disruptor Chemical (2025), by Marie-Odile Soyer-Gobillard, Laura Gaspari, & Charles Sultan, published in The European Society of Medicine Medical Research Archives
(Notable) *** Early Female Transgender Identity after Prenatal Exposure to Diethylstilbestrol: Report from a French National Diethylstilbestrol (DES) Cohort (2024), by Laura Gaspari, Scott Kerlin, et al., published in the Journal of Xenobiotics
(Notable) *** Recognizing, Evaluating, and Prioritizing the Fundamental Factors Influencing the Growing Prevalence of Transgender and Non-Binary Gender Identity in the Pediatric Population (2024), by Nicholas A. Kerna, et al., published in European Journal of Medical and Health Research
*** Enhanced identification of endocrine disruptors through integration of science-based regulatory practices and innovative methodologies: The MERLON Project (2024), by Terje Svingen, et al., published in Open Research Europe
*** Endocrine disruption and male reproductive disorders: unanswered questions (2024), by Richard M. Sharpe, published in the journal Human Reproduction
(Notable) *** Environmental contaminants, endocrine disruption, and transgender: Can “born that way” in some cases be toxicologically real? (2023), by Steven David Holladay, et al., published in Human & Experimental Toxicology
*** Environmental Impact on Sexual Response (2023), by Carlotta Cocchetti, et al., published in Environmental Endocrinology and Endocrine Disruptors: Endocrine and Endocrine-targeted Actions and Related Human Diseases
*** Sexual Differentiation of the Human Brain in Relation to Gender-Identity, Sexual Orientation, and Neuropsychiatric Disorders (2022), by Dick Swaab, et al., published in Neuroscience in the 21st Century: From Basic to Clinical
*** Chapter 31 – Sexual differentiation of the human hypothalamus: Relationship to gender identity and sexual orientation (2021), by Dick Swaab, et al., published in Handbook of Clinical Neurology
(Notable) *** Gender Identity and Sexual Orientation Identity in Women and Men Prenatally Exposed to Diethylstilbestrol (2020), by Rebecca Troisi, et al., published in Archives of Sexual Behavior
*** Aspects of growth and development: endocrine and nonendocrine paradigms (2018), by Levitsky, Lynne L., published in Current Opinion in Endocrinology & Diabetes and Obesity
(Notable) *** Transgender Associations and Possible Etiology: A Literature Review (2017), by Fatima Saleem & Syed W Rizvi, published in the journal Cureus
*** The Increasing Prevalence in Intersex Variation from Toxicological Dysregulation in Fetal Reproductive Tissue Differentiation and Development by Endocrine-Disrupting Chemicals (2016), by Alisa L. Rich, et al., published in Environmental Health Insights
*** (Historical/Notable) Are EDCs Blurring Issues of Gender? (2005), by Ernie Hood, published in Environmental Health Perspectives
*** (Historical/Notable) Prenatal Exposure to Diethylstilbestrol (DES) in Males and Gender-Related Disorders: Results from a 5-Year Study (2005), by Scott Kerlin, published in Researchgate
>> (Chapter 22) What are some of the leading references focusing on broadening the research agenda on transgender identity, health, and support?
Selected Overview, by Ian Cameron
From: Recognizing and responding to misleading trans health research. Skinner S R et al [2023] International Journal of Transgender Health.
Public discourse, care options and research standards for trans young people (inclusive of trans young people with a binary gender, gender-expansive young people, and non-binary young people) have changed substantially in recent years. Over the past two decades, trans people across the globe have seen rising acknowledgement, visibility, and acceptance, accompanied by tenuously obtained legal protections and increasing access to gender affirming care. In older, outdated scientific and medical literature, being trans was considered a mental disorder best treated through eliminating gender non-conforming behaviour or even removing gender non-conforming youth from supportive families. Ethical standards and recommendations for engaging in research with transgender people have also emerged to prevent harm to this marginalized community.
Despite these changes, trans people in general and trans young people in particular remain heavily stigmatized and marginalized, contributing to a disproportionate burden of mental health concerns. Hate crimes against trans people have sharply risen in the U.S. and the U.K., and even these sharp increases are likely underestimates. Anti-transgender rhetoric is pervasive in British and American news media. The existing literature also suggests that adolescents treated with gender-affirming hormones (i.e. testosterone, oestrogen) experience improvements such as reduced anxiety and/or depression, reduced suicidality, improved body image, and other indicators of improved psychological well-being.
The exact meanings of “desistance” and “detransition” in relation to youth with gender dysphoria is conceptually unclear. The term desistance originates from criminology, where it denotes the cessation of criminal behaviours, and was intended to represent gender non-conforming children re-identifying with their assigned sex at birth. However, its operationalization within the scientific literature varies widely. Some studies define desistance as re-identification with one’s assigned sex at birth. Others classify anyone who ceases GAMT as desisting, even if they continue to identify as trans.
Clinicians providing care for trans young people should understand that human gender identity is naturally diverse and that trans children, adolescents and adults have always existed in different cultures and geographical regions throughout human history. Person-cantered and family-cantered assessment and treatment models that support each individual’s path are essential for good care.
From: On, With, By—Advancing Transgender Health Research and Clinical Practice. Streed C et al [2023] Health Equity.
To advance the fields of transgender health research and clinical care and centre trans-led scholarship, there must be an acknowledgment of the consolidated power in cisgender hands and the subsequent need to redistribute such power to trans experts and burgeoning trans leaders. To redress the social structures that cause harm and limit opportunities for trans persons to lead, current cisgender leaders can take actions including deferring opportunities to trans persons to ensure a redistribution of power and resources to trans experts.
Trans scholars represent a diverse, resilient, and vibrant population that is forced to overcome extensive systemic stigma and discrimination to exist in society, let alone thrive in academia. Despite numerous barriers to academic success and career advancement, ∼1.2% of matriculating allopathic medical students in 2021 were trans according to the Association of American Medical Colleges, up from 0.7% in 2018. This does not take into account health researchers and other health care professions. Despite increasing numbers of trans experts in health research and the clinical care of trans populations, these fields remain dominated and dictated by cisgender persons and cis-centric perspectives of health and well-being.
Calls to share resources, center trans-led scholarship, and redistribute power that is often acquired and maintained by cis-privilege have been met with cisgender fragility, a tendency to engage in defensive posturing and outright denial, minimizing concerns raised by trans communities while overemphasizing good intentions. To advance the fields of trans health research and clinical care, there must be an acknowledgment of the power consolidated in cisgender hands, an ongoing multipronged approach to training and elevating trans persons in the fields of health care and health research, and the subsequent redistribution of power to trans experts and burgeoning trans leaders.
To ensure a redistribution of power and resources in the hands of cisgender researchers and clinician leaders to trans experts, cisgender persons can take necessary steps to recruit, collaborate, and elevate trans experts. The underlying assumption is one that is common among many health equity scholars18 and research paradigms;19 specifically, that members of oppressed and excluded groups have experiential knowledge and insider perspective that is vital for achieving (health) equity for that group. Put another way, the lived experiences of trans scholars are part of their “training” in transgender health equity.
However, to achieve more robust incorporation of trans perspectives in trans clinical care and research, cisgender clinicians and researchers can start by active self-reflective practices to recognize and evaluate the power they have in the field. This involves acknowledging their cisgender privilege is rooted in being raised, trained, and supported without gender-identity-specific stressors and subsequently rewarded for their perceived objectivity in entering trans fields. To ensure trans trainees are supported in their endeavours to pursue careers in health research and clinical care, cisgender leaders should develop and support a pipeline of trans experts, especially those from historically and contemporarily excluded ethnoracial groups.
Although there are an increasing number of trans clinicians and researchers, the small ranks of trans experts likely reflects the ways in which gatekeeping and gender-identity-specific stressors from youth through adulthood have impacted trans enrolment in and completion of graduate studies in relevant fields.
Ultimately, cisgender leadership can recognize their consolidated power and take steps to redistribute it. Cisgender leaders should prepare timelines for stepping down from positions of power, including editorial boards, advisory committees, and leadership roles in various organizations related to trans health and clinical care and play more supportive, advisory, and mentorship roles. These steps will result in the cantering and elevation of trans experts in their respective fields and strengthen opportunities for all persons dedicated to advancing the health and well-being of trans persons and communities.
From: Considerations for transgender population health research based on US national surveys. Lette E and Everhart A [2022] Annals of Epidemiology. Science Direct.
Transgender identities and health are highly politicized in the United States leading to restrictions on relevant data collection in national health surveillance systems. This has serious implications on transgender population health research; an urgent area of study given the systemic discrimination faced by transgender individuals and the resultant social and health inequities. In this precarious political climate, obtaining high-quality data for research is challenging and in recent years, two data sources have formed the foundation of transgender health research in the United States, namely the 2015 United States Transgender Study and the Behavioural Risk Factor Surveillance System after the launch of the optional Sexual Orientation and Gender Identity Module in 2014.
While useful, there are serious challenges to using these data to study transgender health, specifically related to survey weighting methodologies, ascertainment of gender identity, and study design. In this article, we detail these challenges and discuss the strengths and weaknesses of various methodological approaches that have been implemented as well as clarify several common errors that exist in the literature. We feel that this contribution is necessary to provide accurate interpretation of the evidence that currently informs policy and priority setting for transgender population health and will provide vital insights for future studies with these now ubiquitous sources of data in the field.
One of the challenges to studying transgender population health in the United States is that transgender identity is not ascertained in the Census or most national health surveys. There have been several studies with the goal of developing survey items that reliably identify transgender individuals. One difficulty of asking this question relates to the diversity of transgender identities a well as the acceptability of asking questions related to gender identity.
To date, three approaches have been implemented for analysis focused on transgender health in the Behavioural Risk Factor Surveillance System Survey [BRFSS]
(1) The most common approach is to conduct design-weighted analysis using the survey weights provided with the data.
(2) Another approach is to exclude the survey weights and only account for strata and clustering in the sampling schema of the survey.
(3) The last approach has been applied for comparisons of transgender groups to cisgender groups and involves using matching.
From: The Erasure of Intersex, Transgender, Nonbinary, and Agender Experiences Through Misuse of Sex and Gender in Health Research. Morrison T, Dinno A and Salmon T [2021] American Journal of Epidemiology. Oxford Academic.
Conflation of the terms and concepts of “sex” and “gender” continues to perpetuate the invisibility of sex and gender minorities and obscure information about the ways in which biological sex and gender affect health. The misuse of sex and gender terms and the sex and gender binaries can yield inaccurate results but also, more importantly, contributes to the erasure of intersex, transgender, nonbinary, and agender health experiences. In this article, we discuss ways in which public health researchers can use sex and gender terms correctly and centre the health experiences of intersex, transgender, nonbinary, and agender individuals. This includes promoting sensitivity in approaching sex and gender minority communities, improving survey questions, and collaborating with GSM communities to improve research quality and participant experiences. Improving our standards for the quality of sex and gender term usage and cantering sex and gender minorities in public health research are imperative to addressing the health inequalities faced by sex and gender minorities.
Genotypic sex and phenotypic sex overlap but are not equivalent. Not only can people have multiple combinations and duplications of X and Y genes, but imprinting and exogenous and endogenous changes to gene expression also complicate the use of sex as a binary measure. Hormonal sex also does not fit well into a binary categorization. All humans have testosterone, oestrogens, and progesterone, which have stereotyped patterns relating to genotype, with notable changes resulting from patterns across one’s life span (e.g., puberty, aging, menopause, pregnancy), use of hormone replacement or suppression therapy, adverse effects from medications, and hormonal effects of disease courses (e.g., polycystic ovarian syndrome). Organ inventories based upon self-report may describe sex, although there is a diversity of sexual organs possible for any person related to genetically driven differences in what internal and external organs people have, which they may or may not be aware of without having had diagnostic imaging, biopsy, or endoscopy. Additionally, sex organs can be altered by surgical procedures for the purposes of gender affirmation, tumour removal, or cancer risk reduction, or at birth (for intersex babies) to ascribe phenotypic sex.
The gender binary is built on the foundation of the medicalized sex binary, where cultural roles, social hierarchies, and political power were drawn from observed differences in reproductive physiology. Gender has long since been recognized as something that can change over one’s lifetime. Gender expression is not linear but a continuum wherein individuals may express themselves as more than 1 gender or as androgynous. An individual’s gender identity may not align with their gender assigned at birth; otherwise these individuals are characterized as “cisgender.” However, gender continues to be used socially and in research as a static binary measure, even when it is not conflated with binary sex.
There are several consequences for public health when sex and gender terms are misused. First, when sex and gender are conflated or falsely combined into sex/gender, our research lacks validity in describing health experiences. Sex, described phenotypically or genotypically, is generally more appropriate for questions of physiology, while the social constructs of gender and transgender are generally more appropriate for questions implicating social structures. These terms are related because both are inhabited at once by every person, but the terms are not interchangeable, and conceptually and methodologically both, neither, or either may be relevant to a specific health question.
Second, by accepting binary gender or sex methodologies, we erase GSM experiences. Asking questions about GSM status requires sensitivity to the collective and individual traumas experienced by minorities within health care and research.
The goal of this article was to address the misuse of sex and gender terms and their binaries and discuss how this affects communities of GSM people. Not only is the conflation and reduction of sex and gender terms harmful to the validity of public health research, it also erases GSM experiences of medical discrimination and increased prevalence of physical and mental health conditions. To adequately serve the GSM community, public health researchers need to conduct research with methodological integrity. This includes careful consideration, planning, and defence of using appropriate sex and gender lenses for medical and social public health research, as well as using the right survey tools to accurately and sensitively assess GSM status. For these changes to occur, we need to adequately train health-care professionals and researchers to use these tools, agree on research standards for methodologically and conceptually separating sex and gender, and involve the GSM community as knowledgeable partners in this change.
From: “Focus more on what’s right instead of what’s wrong:” research priorities identified by a sample of transgender and gender diverse community health centre patients. LeBlanc M et al {2022] BMC Public Health.
Transgender and gender diverse (TGD) people are individuals whose gender identity differs from their sex assigned at birth. While research demonstrates that TGD communities are subject to disparate health outcomes compared to their cisgender peers, health research regarding the TGD community remains limited and researchers rarely centre TGD voices and perspectives in their projects. Conducting TGD research without the inclusion of TGD community input can contribute to disenfranchising the population, ignoring community needs, and causing investigators to miss key topics most influential to TGD population health.
Current research and literature regarding TGD health and public health consist of topics including gender-affirming hormones and surgical procedures, mental health, HIV prevention and treatment, and sexual health. Clinical trials involving trans people are most often in the HIV domain, with less investigation of other health burdens faced by TGD patients.
The stress experienced from interpersonal social stigma and its effect on health was identified as a main research priority in the FGs. Participants shared that their experiences of street harassment and harmful interactions with others were stressors that impact their health and well-being. TGD individuals face a high level of adversity and are subject to oppressive systemic structures and yet subsequently embody resilience. The concept of embodiment reflects that we are simultaneously social and biological organisms whose lived experiences cannot be separated from social context.
Findings highlight the need for investigators to:
1) intentionally represent and investigate the embodiment of complex and heterogenous TGD identities in studying health,
2) consider the role of structural and interpersonal stigma on health, including applying a social determinants of health framework to assess the lived experiences unique to TGD people, and
3) assess the exceptional resiliency encompassed by the TGD community and include health-promoting factors in research.
Given findings from this sample of TGD patients, it is important for research investigators to further explore the social influences on health and well-being. Centreing TGD people throughout the entire research process by designing equitable partnerships, from design to dissemination, will ensure impactful and relevant research that incorporates health outcomes and life experiences unique to TGD communities.
Key Literature References
(Notable) *** Recognizing and Responding to Misleading Trans Health Research (2024), by S. Rachel Skinner, et al., published in the International Journal of Transgender Health
*** Ensuring an inclusive, trans-led future for the field of trans health (2024), by Damien Riggs, et al., published in the International Journal of Transgender Health
(Notable) *** On, With, By–Advancing Transgender Health Research and Clinical Practice (2023), by Carl G. Streed, et. al, published in the journal Health Equity
*** Setting a research agenda in trans health: An expert assessment of priorities and issues by trans and nonbinary researchers (2022), by Jaimie F. Veale, et al., published in the International Journal of Transgender Health
(Notable) *** Considerations for transgender population health research based on US national surveys (2022), by Elle Lett & Avery Everhart, published in Annals of Epidemiology
*** Review on the Transgender Literature: Where are we Now and a Step Beyond the Current Practice? (2022), by Dilini Abeyratne, et. al, published in the journal Endocrines
*** The Erasure of Intersex, Transgender, Nonbinary, and Agender Experiences Through Misuse of Sex and Gender in Health Research (2021), by Tessalyn Morrison, Alexis Dinno & Taurica Salmon, published in the American Journal of Epidemiology
*** Gender-Inclusive and Gender-Specific Approaches in Trans Health Research (2021), by Arjee Restar, et. al, published in the journal Transgender Health
(Notable) *** “Focus more on what’s right instead of what’s wrong:” research priorities identified by a sample of transgender and gender diverse community health center patients (2020), by Merrily Leblanc, et al., published in BMC Public Health
*** Expanding Women’s Health Practitioners and Researchers’ Understanding of Transgender/Nonbinary Health Issues (2020), by Shanna K. Kattari et. al, published in the journal Women’s Health Issues
>> (Chapter 23) What research has been conducted focusing on Disorders/Differences of Sexual Development (DSD) and related topics?
Overview, by Ian Cameron
Introduction
This topic has turned out to be extensive, and as such the studies have been split into different sections. Section A will contain the physiological aspects, section B will contain the psychological aspects, and section C will contain descriptions of Intersex/DSD conditions that are associated with Gender Dysphoria.
It must be emphasized the evidence suggest that by no means all people who are intersex/DSD have Gender Dysphoria, but it is likely that many who do have GD also have an intersex condition. This begs the question is Gender Dysphoria an intersex condition in its own right?
SECTION A PHYSIOLOGICAL
Androgen Insensitivity Syndrome is a comparatively rare intersex/DSD condition, about every 1 in 10,000, is well researched but merits a section of itself.
From: Androgen Insensitivity Syndrome Synonym: Testicular Feminization. Gottlieb B and Trifiro M [2017] National Library of Medicine
Clinical characteristics. Androgen insensitivity syndrome (AIS) is typically characterized by evidence of feminization (i.e., undermasculinization) of the external genitalia at birth, abnormal secondary sexual development in puberty, and infertility in individuals with a 46,XY karyotype. AIS represents a spectrum of defects in androgen action and can be subdivided into three broad phenotypes:
- Complete androgen insensitivity syndrome (CAIS), with typical female external genitalia
- Partial androgen insensitivity syndrome (PAIS) with predominantly female, predominantly male, or ambiguous external genitalia
- Mild androgen insensitivity syndrome (MAIS) with typical male external genitalia
Diagnosis/testing. The diagnosis of AIS is established in an individual with a 46,XY karyotype who has: undermasculinization of the external genitalia, impaired spermatogenesis with otherwise normal testes, absent or rudimentary müllerian structures, evidence of normal or increased synthesis of testosterone and its normal conversion to dihydrotestosterone, and normal or increased luteinizing hormone (LH) production by the pituitary gland; AND/OR hemizygous a pathogenic variant in AR identified by molecular genetic testing.
Management. hemizygous Treatment of manifestations: To prevent testicular malignancy, treatment of CAIS may include either removal of the testes after puberty when feminization is complete or prepubertal gonadectomy accompanied by estrogen replacement therapy.
Androgen insensitivity syndrome (AIS) should be suspected in an individual with the following clinical, family history, radiologic, and supportive laboratory findings.
Clinical features:
- Absence of extragenital abnormalities
- Two nondysplastic testes
- Absent or rudimentary müllerian structures (i.e., fallopian tubes, uterus, and cervix) and the presence of a short vagina
- Undermasculinization of the external genitalia at birth
- Impaired spermatogenesis and/or somatic virilization (some degree of impaired virilization at puberty)
Complete androgen insensitivity syndrome (CAIS). Individuals with CAIS have normal female external genitalia with absence of female internal genitalia. They typically present either before puberty with masses in the inguinal canal that are subsequently identified as testes or at puberty with primary amenorrhea and sparse to absent pubic or axillary hair. Breasts and female adiposity develop normally. Sexual identity and orientation are typically female and heterosexual. In the case of ambiguous individuals, could also present microphallus, undescended testes and hypospadias.
Partial AIS with ambiguous genitalia or predominantly male genitalia (PAIS, Reifenstein syndrome). Determining the sex of rearing may be an issue for children with frank genital ambiguity. Individuals with PAIS and predominantly male genitalia are raised as males. Gynecomastia at puberty and impaired spermatogenesis occur in all individuals with PAIS. Pubic hair is usually moderate; facial, body, and axillary hair are often reduced.
Mild AIS (MAIS, undervirilized male syndrome). The external genitalia of affected individuals are unambiguously male. They usually present with gynecomastia at puberty. They may have undermasculinization that includes sparse facial and body hair and small penis. Impotence may be a complaint. Spermatogenesis may or may not be impaired.
Differential Diagnosis
Mayer-Rokitansky-Kuster-Hauser (MRKH) syndrome (OMIM 277000) is diagnosed in phenotypic females who exhibit amenorrhea and have a partial or complete absence of the cervix, uterus, and vagina. Individuals with MRKH can be distinguished from those with CAIS by confirmation of a 46,XX karyotype.
Hypospadias resulting from an AR pathogenic variant (and thus a part of the spectrum of PAIS) cannot be distinguished from hypospadias resulting from other (largely undefined) causes by the examination of the genitalia alone. AR variants associated with hypospadias are likely rare.
MAIS caused by single-nucleotide variants of AR may be clinically indistinguishable from MAIS caused by expansion of the polymorphic CAG repeat in AR. Pathogenic expansion of this triplet repeat is the cause of spinal and bulbar muscular atrophy (SBMA), also known as Kennedy disease).
Undermasculinization of the external genitalia and pubertal undervirilization are components of many different syndromes that have no etiologic relation to AR. They may or may not have a pathogenic relation to the androgen receptor protein. The one exception is a contiguous gene deletion syndrome that includes the AR locus and results in intellectual disability and genital abnormalities
46,XY infants born small for gestational age may have clinical features of PAIS with no identifiable AR pathogenic variant. It has been suggested that this association be termed “XY DSD with fetal growth restriction, as yet unexplained” [ Lek et al 2014]. A survey of the Androgen Receptor Gene Mutations Database suggests that AIS may be attributable to factors other than the presence of AR variants.
Assignment of sex of rearing.
The issue of sex assignment in infancy when the child is being evaluated for ambiguous genitalia is paramount. It requires informed decision making by parents and health care personnel and should be resolved as early as possible, after a multidisciplinary evaluation has been completed.
Even in CAIS this may not always be easy. Psychological counselling and use of support groups can be of benefit. Gender identity has become a topic of increasing importance due to the possibility of changes in sex assignment over time. Issues of sexual orientation regardless of gender phenotype have also become increasingly important to explore and discuss.
A common practice is to remove the testes after puberty when feminization of the affected individual is complete, since feminization occurs partly by testicular oestrogen and partly by peripheral conversion of androgen to oestrogen.
The rationale for postpubertal gonadectomy is that testicular malignancy, which develops at the usual rate for cryptorchid testes, seldom occurs before puberty. Prepubertal gonadectomy is now only considered if inguinal testes are physically or aesthetically uncomfortable, and if inguinal herniorrhaphy is necessary. In this event, oestrogen replacement therapy is necessary to initiate puberty, maintain feminization, and avoid osteoporosis.
The assignment of sex in an infant with ambiguous genitalia is a complex process that requires timely assessment by a multidisciplinary team in consultation with the family and should be resolved as early as possible. Aside from purely anatomic and surgical considerations, the choice of a male sex-of-rearing demands a therapeutic trial with pharmacologic doses of androgen to try to predict potential androgen responsiveness at puberty. Furthermore, appreciable phallic growth in response to administered androgen facilitates reconstructive surgery.
Gender Identity: In a long-term outcome study of DSDs that included CAIS, it was noted that while many affected individuals fare well, dissatisfaction with original sex assignment has been underestimated and gender and sexual counseling should be part of the multidisciplinary service available to individuals with DSDs.
From: Androgen insensitivity syndrome. Hughes I et al [2012] The Lancet.
Androgen insensitivity syndrome in its complete form is a disorder of hormone resistance characterised by a female phenotype in an individual with an XY karyotype and testes producing age-appropriate normal concentrations of androgens. Pathogenesis is the result of mutations in the X-linked androgen receptor gene, which encodes for the ligand-activated androgen receptor—a transcription factor and member of the nuclear receptor superfamily.
Several clinical disorders arise because of complete or partial resistance to the action of hormones. Examples include diabetes due to insulin resistance and reproductive disorders caused by resistance to gonadotropin and steroid hormones. Male development during foetal life occurs only when an XY zygote directs the bipotential gonad to become a testis (sex determination), which in turn secretes sufficient amounts of active androgen to produce the male phenotype (sex differentiation)
Diagnosis of complete androgen insensitivity syndrome can happen by chance. The sex of a foetus is now increasingly known before birth through analysis of karyotypes, chorionic villi, amniotic fluid samples, or maternal circulating free foetal DNA,11 and use of three dimensional ultrasonography. Complete androgen insensitivity syndrome can therefore some times be diagnosed as a result of mismatch between the prenatal sex prediction and the phenotype at birth In infancy, complete androgen insensitivity syndrome presents as an inguinal hernia or labial swelling containing a testis in an apparently female infant. Bilateral inguinal herniae are rare in female infants—the incidence of complete androgen insensitivity syndrome in such patients is 1–2% during infancy.
Low testosterone concentrations in infants with complete androgen insensitivity syndrome are not fully understood but might suggest that androgens need to act prenatally on the hypothalamic–pituitary axis to prime the LH surge after birth.
The clinical presentation of partial androgen insensitivity syndrome depends on the degree of responsiveness of the external genitalia to androgens. The typical pheno type is micropenis, severe hypospadias (perineo scrotal), and a bifi d scrotum that might contain gonads. Occasionally, the appearance of the genitalia is more consistent with complete androgen insensitivity syndrome, apart from the degree of clitoromegaly. This presentation is referred to as severe partial androgen insensitivity syndrome, and sex assignment is generally female.
Defects in androgen production:
• Partial gonadal dysgenesis
• Mutations in SRY, NR5A1, WT1
• Mutations of the luteinising hormone receptor
• Biosynthetic enzyme deficiencies
• 17,20-lyase deficiency
• P450 oxidoreductase deficiency
• 17β-hydroxysteroid dehydrogenase deficiency type 3
• 5α-reductase deficiency type 2
Genetic Effects:
• Klinefelter’s syndrome
• Smith-Lemli-Opitz syndrome
• Denys-Drash syndrome
• Frasier’s syndrome
PAIS (Partial Androgen Insensitivity Syndrome)
• Mutations of the androgen receptor gene
• Normal androgen receptor gene with foetal growth restriction
Management of androgen insensitivity syndrome should address functional, sexual, and psychological issues such as disclosure, gonadectomy and subsequent hormone replacement, creation of a functional vagina, and provision of genetic advice. Care needs to be individualised, flexible, and holistic. Management is dependent wholly on a multidisciplinary team.
Classification of Causes of Disorders of Sex Development
Sex chromosome anomalies
• 45X/46,XY (mixed gonadal dysgenesis)
• 46,XX/46,XY (chimerism) • 47,XXY (Klinefelter’s syndrome) 46,XX
• Disorder of gonad development—eg, gonadal dysgenesis, ovotesticular disorders of sex development
• Foetal androgen excess—eg, congenital adrenal hyperplasia, aromatase deficiency, P450 oxidoreductase deficiency
• Maternal androgen excess—eg, luteoma of pregnancy 46,XY
• Disorder of gonad development—eg, gonadal dysgenesis, ovotesticular disorders of sex development
• Disorder of androgen production—eg, mutation of the luteinising hormone receptor, 17β-hydroxysteroid dehydrogenase deficiency type 3, 5α-reductase defi ciency type 2
• Disorder of androgen action—eg, complete, partial, and mild androgen insensitivity syndromes.
Psychosocial support is central to the multidisciplinary approach to management of complete androgen insensitivity syndrome.89 Presenting adolescents and parents of children with the disorder will have to make important decisions at diagnosis about treatments and the timing and extent of any surgical interventions. Concerns should focus on assimilation of the disconnect between chromosomal, gonadal, and phenotypic sex and its implications. Most centres caring for patients with disorders of sex development provide specialist psycho logical support.
Disclosure must be done carefully, especially for children with complete androgen insensitivity syndrome as they approach pubertal age. Issues to address include implications of an XY karyotype, the presence of testes, absence of a uterus, infertility, and sexual function. Such information should be shared with parents initially, with age-appropriate disclosure as the child grows up. Long-term psychosexual outcome in complete androgen insensitivity syndrome suggests a trajectory of female-typical development, with the assimilation of a female identity and female-typical behaviour, and psychological wellbeing similar to that of other women. Altered gender-related self-concept can be problematic but might respond to psychological intervention.
From: The epidemiology of disorders of sex development. Berglund et al. [2025]. Best Practice and Research Clinical Endocrinology and Metabolism
During recent years the epidemiology of disorders of sex development (DSD) has been more clearly delineated. Disorders of sex development (DSD) encompass a broad and heterogeneous group of congenital conditions where sex, from a biomedical perspective, is atypical at either the chromosomal, gonadal, genital, and/or hormonal levels. DSD is therefore an umbrella term for a range of very different conditions. Atypical genitalia are part of the phenotypic spectrum of most DSD conditions, and a few epidemiological studies have addressed atypical genitalia as a broader category. The complexity of DSD, as encompassing many different conditions with highly variable phenotypes that may present at different stages of life, poses significant challenges in obtaining reliable estimates in most cases.
Turner Syndrome
TS is associated with a significant comorbidity burden, in particular a high risk of cardiovascular malformations, high cardiovascular disease risk and a proneness to pro-inflammatory conditions with an increased risk of most autoimmune diseases, contributing to the reduced life-span in TS. The increased comorbidity is believed in part to be related to hypogonadism, but certainly specific genetic mechanisms related to the karyotype are contributing directly to the clinical phenotype.
Klinefelter Syndrome
A typical presentation of KS is due to prolonged exposure to male hypogonadism. Similar to TS, specific genetic modifications brought on by the presence of an extra X chromosome seem to also play a significant direct role beyond the effects of hypogonadism.
One of the more intriguing findings from recent epidemiological studies on KS revolves around the undiagnosed phenotype. Based on genetic data from the UK Biobank it has recently been demonstrated that men with KS, who at the time of assessment were not clinically diagnosed with KS, present with a pattern of increased comorbidities and poor overall health.
However, today, most men with Klinefelter are never diagnosed, with also substantial diagnostic delay in those obtaining diagnosis. KS is associated with increased risk of several autoimmune diseases, including Addison’s disease, type 1 diabetes mellitus, multiple sclerosis, acquired hypothyroidism, rheumatoid arthritis, Sjogren’s syndrome and systemic lupus erythematosus. Interestingly prostrate cancer is lower than the background population. Significantly increased occurrence of schizophrenia, bipolar disorder, depression, ADHD, and neurodevelopmental disorders, herein autism spectrum disorder, increased risk of anxiety and panic disorders, depression,
47,XYY
Similar to 47,XXX syndrome, the first reports of 47,XYY date back more than 60 years. It is associated with an increased occurrence of developmental delay, learning difficulties, and social- and behavioural disorders. Little is, however, known about associated comorbidities. There is a significantly increased occurrence of schizophrenia, bipolar disorder, anxiety, depression, ADHD, and neurodevelopmental disorders, herein autism spectrum disorder.
45,X/46,XY DSD
45,X/46,XY DSD is associated with a broad spectrum of genital phenotypes, ranging from typical female genitalia to varying degrees of genital ambiguity and, in some cases, slightly under virilized or typical male genitalia. While individuals with female genitalia fall under the TS diagnosis, those with ambiguous or male genitalia do not.
46,XX DSD. XX Males
The classic XX male present with complete male genitalia and the majority are diagnosed as part of diagnostic work-up for infertility [105]. Some degree of genital variability however exists, especially in those without presence of the SRY gene, and include under virilized traits like maldescended testis but also more ambiguous traits like hypospadias and micropenis.
46,XY DSDXY Females
Women with 46,XY are a mixed group with different genetic background and since they are all rare it is difficult to get sound epidemiological data.
Epidemiological studies have greatly improved our understanding of DSD through recent years, have led to reasonably sound estimates of prevalence for the most frequent diagnoses, have detailed morbidity and mortality patterns and have for some conditions also clarified the impact on socio-economic achievements. Emerging data suggest that hormone replacement therapy improves aspects of morbidity and mortality in Turner and Klinefelter syndrome, however, there is a need for more data on this issue, detailing advantages and possible drawbacks to such treatment. There is a need for more information concerning the socio-economic impact of DSD, with current data showing a rather profound effect of sex chromosome DSD, while more discrete effects are present among 46,XY and 46,XX DSD. Not much is known concerning the socio-economic impact on CAH. DSD’s appear to have many comorbidities in common.
From: Hypogonadism and Cryptorchidism. Rodprasert et al. [2020]. Frontiers In Endocrinology.
An endocrine-disrupting chemical (EDC) is an exogenous substance or mixture that modifies function(s) of the endocrine system and consequently causes adverse health effects in an intact organism, or its progeny, or (sub) populations. Some EDCs show anti-androgenic or estrogenic effect, or affect androgen or INSL3 levels or action during foetal development in animal studies. Animal studies have demonstrated that exposure to anti-androgen or oestrogen during a critical period of male reproductive organ development during embryonic days 13.5–17.5 in rats (equivalent to GW 7–15 in humans) is related to the occurrence of cryptorchidism. In humans, boys with a history of in utero exposure to diethylstilbesterol, a synthetic non-steroidal oestrogen, have been shown to have a two-fold increased risk of cryptorchidism. Association between EDCs, such as dioxins, polybrominated flame retardants and pesticides, and cryptorchidism, has also been identified.
The cause of isolated cryptorchidism is still not fully understood, and therefore more studies investigating the mechanisms of cryptorchidism are still needed. The studies on hormonal treatment during mini-puberty in CHH boys showed promising results on testicular descent, however, the treatment outcomes were observed without randomization of the subjects. Additionally, long-term outcomes are still largely unknown. Therefore, randomized, multi-centre studies that explore the role of gonadotropin or GnRH treatment in mini-puberty and peri-puberty in CHH patients with cryptorchidism are necessary to gain more knowledge on the effects of this treatment.
From: Disorders of Sex Development: Classification, Review, and Impact on Fertility. Acien M and Acien P. [2020] Journal Of Clinical Medicine.
The phenotypic sex of a person depends on the type of gonad that develops in the embryo, a process that in itself is determined by the constitution or genetic inheritance of the individual, although the development of the gonads is different from that of any other organ, since they have the potential to differentiate into two functionally distinct organs, i.e., testes or ovaries. However, there are many more elements that determine the sex of an individual; additionally, a person’s sexual identity includes any behaviours with sexual overtones, such as characteristic gestures and habits, ways of speaking, preferences about leisure, and the content of dreams. Indeed, hormonal influences not only affect internal and external genital development and differentiation; the embryo’s brain has also been shown to differentiate sexually, perhaps through control mechanisms similar to those developed by the external genitalia. On the other hand, it is also possible that the induction of the central nervous system(CNS)by hormones affects the patterns of hormonal secretion and consequently, sexual behaviour in adults. Thus, the sex of an individual and their sexual expression, i.e., homo or heterosexual, must be considered the result of all influences that the individual receives, both before and after birth.
From: Ambiguous Genitalia and Disorders of Sexual Differentiation. Mehmood K and Rentea R [2023] National Institute of Health.
The birth of an infant with ambiguous genitalia generates difficult multiple medical, surgical, ethical, psychosocial, and physical issues for patients and their parents. Phenotypic sex results from the differentiation of internal ducts and external genitalia under the influence of hormones and other additional factors. When discordance occurs among three processes (chromosomal, gonadal, phenotypic sex determination), a DSD is the result.
Normal sexual development in utero is dependent upon a precise and coordinated spatiotemporal sequence of various activating and repressing factors. Any deviations from the usual pattern of differentiation can present as DSDs. Two distinct processes occur in normal sexual development. The first of which is sex determination, in which the bi-potential gonads are induced to form either the male testes or the female ovaries. Secondarily, the newly formed gonads secrete hormones to modulate the formation of internal and external genitalia. The phenotypic manifestation of DSDs are diverse and can include; bilateral undescended testes, severe hypospadias (scrotal or perineal), clitoromegaly, a fusion of posterior labial folds, female external genitalia with palpable gonad, discordant genitalia, and sex chromosomes. Regardless of presentation or severity, individuals require an interprofessional approach that is warranted to improve the quality of life and achieve the best possible outcomes.
A multitude of genes plays an important role in orchestrating this complex sequence of events. An overview of the most important genetic factors is provided below.
1. SRY gene: the sex-determining region of the Y chromosome is the chief regulator of male sex differentiation; expression causes translation of SRY protein, which mediated testicular development.
2.SOX9 gene: expression of this gene follows the SRY gene and is responsible for the differentiation of Sertoli cells.
3. NR5A1/SF-1: The steroidogenic factor gene codes an important transcription factor involved in male development and steroid biosynthesis. [
4. DHH gene: The desert hedgehog gene plays a role in testicular differentiation.
5. DAX/NROB1: Considered as an antitestis factor up-regulated in the ovary.
6.WT1: Codes a transcription factor involved in renal and gonadal development, mutation results in various congenital syndromes of abnormal genitourinary development.
7. Wnt4 and Wnt 7a: Wnt 4 suppresses male sexual differentiation and ovarian androgen production.
A mutation in any of these above genes may lead to the development of DSD. A loss of genes involved in male sexual development can lead to an undervirilized male or 46 XY with a female phenotype.
The male external genitalia requires the presence of dihydrotestosterone for normal phenotypic development. The deficiency of this hormone or resistance may lead to undervirilized genitalia.
The incidence of a child with a disorder of sexual development (DSD) is approximately 1 in 1000 to 4500 live births. The most frequently occurring etiology was congenital adrenal hyperplasia (CAH), followed by androgen insensitivity and mixed gonadal dysgenesis. Psychosexual development is dependent on factors such as societal and cultural norms, in utero exposure to androgen, genetic differences, and familial dynamics. A need to move away from physician-directed early gender assignment surgeries is warranted because of poor long-term outcomes. The management should be focused on three main domains; initial stabilization, accurate diagnosis, and decisions on the gender of rearing and planning of surgical intervention and hormonal treatment.
The decision for gender assignment should be made upon the best available evidence and considerations of such as type of DSD, prenatal androgen exposure, the possibility of fertility and sexual functionality, and psychosocial factors. There are strongly differing viewpoints regarding the timing of gender assignment. The first is to assign complete genital reconstruction after birth to avoid internal conflicts with the patient or external societal conflicts as the child develops. The opposing viewpoint is that gender assignment is a shared decision that the affected individual participates in during puberty- essentially, physicians and family cannot predict future gender identity or sexual orientation. Three considerations in the discussion of gender assignment include the functional and anatomic ability of the genitalia (size of the phallus or vagina, fertility potential), the cause of the DSD, and the values and desires of the family. The basic principles of surgery are to ensure the best cosmetic results, preserve sexual functioning, preserve fertility if possible, and decrease the risk of malignancy in the dysgenetic gonad. Deferring surgery is often advocated until the child is old enough to confirm their gender identity.
From: Ambiguous Genitalia in the Newborn. Fluck C and Guran T [2023]. NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
Ambiguous genitalia in a newborn are the clinical sign of atypical sexual development of the external genitalia in utero. This condition is rare and can result from various underlying factors, including certain disorders with potentially severe consequences, such as cortisol deficiency due to congenital adrenal hyperplasia. Therefore, it is crucial to promptly determine etiology when ambiguity is observed. The formation of typical male or female external genitalia is a complex process involving a cascade of genetic and physiological events that begin with sex determination and progress through the differentiation of internal and external reproductive structures. When this process is disrupted and does not occur in the typical manner, it is referred to as a difference or disorder of sex development (DSD). Not all DSD cases present with ambiguous genitalia at birth; for example, complete androgen insensitivity syndrome does not, but all cases of ambiguous genitalia are the result of a DSD.
Typical male and female development commences with the presence of the typical 46,XY or 46,XX chromosomes, which play a pivotal role in determining the indifferent gonads. Around the 6th week of gestation, these gonads follow pathways to develop into male-typical or female typical gonads. This gonadal determination is intricately regulated by a complex interplay of multiple genes, which guide the male gonads to become testes and the female gonads to become ovaries. The development of external genitalia begins with a neutral anlage, including a genital tubercule, genital folds, and a urogenital sinus. These structures are subsequently differentiated into typical male external genitalia under the influence of androgens, particularly dihydrotestosterone (DHT). Conversely, for the development of typical female external genitalia, the absence of androgens is crucial to prevent virilization. Therefore, ambiguous genitalia at birth can arise from either an excessive or insufficient androgen effect on the neutral external genital anlage in males or females.
The reported incidence of ambiguous genitalia in newborns is approximately one in 4,500, although due to under reporting that figure could be more common. It is essential that a newborn with ambiguous genitalia and their parents are promptly referred to a specialized centre for evaluation. This evaluation should be carried out by a multi-disciplinary team specializing in DSD in accordance with international recommendations on diagnostic and therapeutic strategies. This team should provide holistic care and treatment guidance, collaborating closely with relevant subspecialists and peer support groups.
The discordance between genetic, gonadal, or anatomic sex is commonly referred to as DSD. In addition to candidate gene testing, the new era of molecular diagnostic tools, including whole exome/genome sequencing has uncovered numerous novel molecular etiologies in recent years. Accurate molecular diagnosis aids in managing affected individuals and provides families with information concerning prognosis and the risk of recurrence.
The etiology of genital ambiguity in newborns is diverse and can have significant implications for management. Therefore, obtaining an accurate diagnosis through a medical workup is crucial. Some investigations are urgent, such as ruling out or confirming and treating potentially life threatening adrenal insufficiency with mineralocorticoid and glucocorticoid replacement therapy in children with underlying CAH.
Assigning or registering the sex of a newborn with atypical external genitalia is a complex and important decision that requires careful consideration, consultation, and a patient-centered approach. The parents and DSD network team should not rush but take the time needed to come to a consensus in the best interest of the child in its environment. Not knowing whether the newborn is a girl or boy causes mostly a lot of distress and one is tempted to call it an emergency, but if there are no medical reasons to make it an emergency (like e.g., suspected adrenal insufficiency or additional organ anomalies), it is important to declare it accordingly and inform that the newborn is not at risk and actually does not care whether it is a male or female or intersex person at this moment. Thus, the stress of ambiguity of the newborn is actually at this moment “only” an issue of the parents and the care team who mostly wish to know ASAP whether the child can be assigned/registered a “correct” sex that might also fit later in life. A god reason why Intersex/DSD should be recognised.
Generally, people believe that the sex chromosomes indicate a person’s “true sex” and laws exist supporting this idea, to the detriment of some individuals affected by DSD. Scientifically speaking, it is clear that the majority of genes on the X chromosome do not influence sex development and differentiation, although the AR gene is necessary for phenotypic masculinization. Concerning the Y chromosome, only the SRY gene contributes to testicular formation. In fact, most of the genes required for sex development and differentiation are found on the autosomes. Therefore, chromosomes do not dictate the sex of rearing in newborns affected by a DSD and are only one piece of a big puzzle.
Only recently has the understanding of, and reaction to, having a child with ambiguous genitalia received systematic study. For some parents and caregivers, feelings of isolation and concern over what the future may hold for their affected child in terms of stigmatization and sexual dysfunction are paramount. The importance of a multidisciplinary and compassionate approach to the care of newborns with ambiguous genitalia, acknowledging the complex medical, psychological, and emotional aspects involved in such cases, is essential. The critical role of specialized teams and support in ensuring the well-being of both the child and his/her family, is similarly essential.
SECTION B PSYCHOLOGICAL
From: Differences/Disorders of Sex Development: Medical Conditions at the Intersection of Sex and Gender. Sandberg and Gardner. [2022] Annual Review of Clinical Psychology
Defined as congenital conditions in which development of chromosomal, gonadal, or anatomic sex is atypical, differences or disorders of sex development (DSDs) comprise many discrete diagnoses ranging from those associated with few phenotypic differences between affected and unaffected individuals to those where questions arise regarding gender of rearing, gonadal tumour risk, genital surgery, and fertility. Controversies exist in numerous areas including how DSDs are conceptualized, how to refer to the set of conditions and those affected by them, and aspects of clinical management that extend from social media to legislative bodies, courts of law, medicine, clinical practice, and scholarly research in psychology and sociology.
Variations in genetic or hormonal determinants of somatic sex development can result in a newborn with characteristics that do not fit neatly into either the male or female category
Some people with DSDs adopt intersex as an identity rather than as a term for a medical condition. Others prefer not to be defined by their biology or want to distance themselves (or their children) from words that may imply atypical gender or sexuality. Although those born with DSDs may identify with lesbian, gay, bisexual, and transgender (LGBT) or other gender-nonconforming communities, many view themselves as cisgender (i.e., accepting the boy/man or girl/woman category in which they were reared).
Parents are often unaware DSDs exist until they receive their child’s diagnosis. Conflicting clinical management strategies contribute to and complicate information-collecting and promote parental distress.
Having a child born with atypical genitalia is often perceived as problematic and brings about changes in parental roles, responsibilities, goals, and social status. Parents worry sharing information about their child’s condition will lead to rumours, gossip, and teasing, resulting in isolation and withdrawal from usual support systems. A major issue in the clinical management of DSDs involves elective genital or gonadal surgery. In 2018, the American Academy of Paediatrics reaffirmed its endorsement of “patient- and family-cantered care”—core principles include shared decision making (SDM) involving the family and child
Many studies have reported sexual discomfort and dysfunction accompanying DSDs, Insofar as early genital surgery has been a feature of standards of care in DSDs, participants in long-term follow-up studies have generally received surgery.
Unlike atypical gender-role behaviour or a non heterosexual orientation, which are not targets of clinical care, there are good reasons for wanting to avoid rearing in a gender that increases the likelihood that the person will experience gender dysphoria. In DSDs, the most common finding is that gender identity follows the gender of rearing regardless of sex chromosome complement or prenatal androgen exposure.
Given these principles, patient- and family-cantered care is recommended in the management of DSDs. As applied to DSDs, patient-centred care includes the following:
1. Provide medical and surgical care when real and present threats exist to patient physical well-being
2. Recognize that what is typical/acceptable for one individual may not be for another; providers should not force patients into a social norm.
3. Minimize potential for patients and families to feel ashamed, stigmatized, or overly fixated on genital appearance; and promote openness.
4. Ask oneself, when elective surgical or hormonal treatments are considered, whether they are needed for the child’s benefit versus to allay parental distress.
5. Respect parents by addressing their concerns and distress empathetically, honestly, and directly and helping them obtain behavioural health care
6. Directly address children’s psychosocial distress through psychosocial interventions and peer support
7. Speak the truth to the family and the child, answering questions promptly and honestly—including the patient’s medical history.
Issues commonly affecting the DSD community include information about specific conditions and/or aspects of care that are lacking, conflicted, or anxiety-provoking; parental stress; stigma, shame, and secrecy; legal and ethical questions in paediatric care surrounding consent, assent, child rights, and parental responsibilities, largely in regard to surgical procedures; influence of religion and culture; and nosocomial trauma.
From: Management of 46,XY Differences/Disorders of Sex Development (DSD) Throughout Life. Wisniewski A et al. [2019] Endocrine Reviews
Decisions regarding sex of rearing in newborns with DSD are complex and can be especially challenging for those with a 46,XY karyotype and severe undervirilization of the genitalia. Such decisions are based on the understanding that gender identity, or the gender a person identifies with, does not always align with a person’s genetic, gonadal, or anatomic sex. Sexual attraction toward males, females, or both is likewise difficult to predict according to a person’s biological sex.
Psychological support is a keystone for interdisciplinary management, and every parent caring for an affected child should be offered counselling by an experienced mental health specialist. Distress about the general health of their child, coupled with the fear of stigma surrounding their child’s diagnosis, is often reported by parents.
Stigma, compromised self-esteem, negative body image, social anxieties, and traumatic sexual experiences contribute to dissatisfaction when it exists as do suboptimal mental health, endocrine, and surgical interventions. Historically, both patients and parents were either totally uninformed or inadequately informed about DSD and related treatment options. More recently, patients and parents report increased knowledge in these areas; however, there remains room for improvement. A key principle of family-centred care is the ongoing provision of complete and unbiased information to patients and families.
From: Psychosocial and psychosexual aspects of disorders of sex development. Cohen-Kettenis [2010]. Best Practice and Research Clinical Endocrinology and Metabolism
The treatment of individuals with disorders of sex development (DSDs) requires the input of many disciplines. Although the psychological outcome of DSD is often satisfactory, medical and psychosocial factors may put the development of children with DSD in many ways at risk. Even in adulthood, certain aspects of life may remain challenging. Gender assignment or physician-imposed gender reassignment may result in the wish to change gender by the person involved; genital ambiguity may cause parental rejection; or genital surgery may create sexual dysfunctions, to name a few.
it’s possible to have multiple DSD conditions. This can occur when concurrent mutations in different genes, or when a person has a combination of genetic and hormonal influences, leading to a complex interplay of effects on sex development. For example, individuals with 46,XY DSD may have undervirilization due to mutations in genes like AKR1C4 and AKR1C2, which are involved in testosterone synthesis. Additionally, DSD conditions can involve abnormalities in multiple stages of development, such as gonad formation, development of reproductive organs, or hormone production.
From: Psychological Aspects of the Treatment of Patients with Disorders of Sex Development. Sandberg D, Gardner M and Cohen-Kettenis P [2012] National Institute of Health
Research on the psychological development of persons with Disorders of Sex Development (DSD) has focused on understanding the influence of atypical sex hormone exposure during steroid sensitive periods of prenatal brain development on the process of psychosexual differentiation (i.e., gender identity, gender role, and sexual orientation). In contrast, analysis of clinical management strategies has focused on gender assignment and the desirability and timing of genital surgery. This review focuses on the psychological issues that confront clinicians managing the care of persons born with DSD and their families. Particular attention is paid to processes and factors that potentially mediate or moderate psychosocial and psychosexual outcomes within and across developmental stages
In cases in which gender assignment is in question, or gender reassignment is under consideration, decision making needs to be informed by both developmental and clinical psychology. The necessity of psychological counselling also emerges in the context of decisions about the timing of interventions, education of the patient and others about medical history (i.e., disclosure), management of potential psychosocial or educational problems that emerge for the child, or when parents need support in understanding the etiology of the child’s condition and its implications. The importance of these aspects of care is reflected by the increasing participation of mental health professionals in multidisciplinary DSD teams.
An ethical question arises in that should an unborn infant is known to have a DSD should it be terminated, despite the fact the child can grow into an adult and led a productive life. Is it also ethical to surgically or pharmaceutically alter an infant that is different and does not conform to societal norms? Especially in the cases of some DSD’s where the adult gender identity cannot be predicted.
DSD that are a consequence of errors of androgen biosynthesis have historically been particularly challenging from the standpoint of gender assignment. In contrast to the common pattern of gender change from female to male in persons with 46, XY DSD secondary to errors in androgen biosynthesis, a recent report suggests a markedly different outcome.
Biology, however, also plays a role in the shaping of gender-role behaviour. There is substantial evidence from animal and human research that sex hormones, androgens in particular, play an important role in the differentiation of gender-role behaviour, gender-typed preferences, and even aspects of personality. Studies of sex-steroid levels in the blood or amniotic fluid of pregnant women and gender-related behaviours of their children have demonstrated positive associations between androgen exposure and male-typical behaviour in healthy girls. Timing, dose and type of androgen exposure seem to be important. Similarly, studies of gender-role behaviour in persons with DSD also suggest that sex hormone exposure during sensitive development periods play a role in the formation of behaviours exhibiting sex-related variability. The influence of early sex hormone exposure on the formation of gender identity is less clear.
Information management refers to two processes: first, the sharing of information about the DSD between clinicians, the parents and the child and second, the sharing of information about the condition by the child or family with the wider social environment
Major psychosocial and social-environmental aspects of DSD and its management, identified in earlier developmental stages, can re-emerge during childhood. Gender assignment and possible early reassignment will have taken place previously; however, parental questions and uncertainties may emerge if they observe their child engaging in gender-atypical play (e.g., boys playing with baby dolls or girls rough-housing).
The age that healthcare provider/parent-imposed gender reassignment can take place without harming the child’s gender and general psychological development remains an open question. Although it is clear from developmental psychology studies in normative samples that the person’s ability to cognitively identify one’s gender occurs around 30 months of age, it is not precisely known when affective aspects of gender identity develop and until what age do they remain flexible. The process of gender development in children with DSD may follow a different pathway than in children without a DSD.
Children will require explanations for multiple aspects of the DSD and associated clinical management. For instance, they may wonder why they need medication in childhood or hormone replacement at the beginning of puberty; why they have scars in their genital area; or why they have to visit the clinic and receive physical examinations more frequently than peers. If the child has not been adequately and timely informed, atypical gender-role behaviour or sexual feelings (e.g., sexual attraction to same-gender peers) may create anxieties.
In transgender (i.e., physically typical at birth) adolescents and adults experiencing gender dysphoria, the gender reassignment decision is taken in phases. In the first, diagnostic phase, it has to be established that the person fulfills DSM or ICD criteria for the diagnoses “gender identity disorder” or “transsexualism” and that the person is physically and psychologically ready to undergo gender reassignment. The next phase usually consists of receiving hormones of the desired gender and social transitioning. Undergoing surgery to change the genitals and sometimes other somatic sex characteristics is typically the last phase of the treatment.
A very useful part of the gender reassignment procedure is what was previously called the “real-life experience” phase. In this phase, one lives full-time in the desired gender role to tryout, on a daily basis, what it is like to live in the desired gender before one makes irreversible change.[64] In this phase the person’s feelings about the social transition, including coping with the responses of others, is a major focus of the discussions and counselling. In gender dysphoric adolescents without DSD, one option is to suppress puberty by using gonadotropin-releasing hormone analogues. This reversible treatment is meant to provide the adolescent time to consider gender reassignment without experiencing development of secondary sex characteristics. Feminizing/masculinizing hormone therapy (oestrogens/anti-androgens/progestins for male to-females, androgens for female-to-males) is considered only partially reversible, as some of the changes persist even if hormone therapy is discontinued.
The developmental pathway is a remarkably productive metaphor. … At its simplest, the idea of a pathway suggests a route that is travelled over time, in which there are constraints over the directions the traveller can take, and there is an ordered sequence of events or experiences… a traveller (walker) can take one of a number of possible pathways over a changing terrain, for example, encompassing relatively easy walking before climbing up steep mountain paths… If developmental pathways resemble such physical paths, we can make predictions, such as that there will be phases of the journey where the path taken by an individual is highly predictable but punctuated by points at which choices are made among different paths…. The pathway metaphor also provokes ideas regarding mechanisms in development. For example, there are multiple ways in which decisions regarding which path to take can be made. They can be based on an overview of the ultimate aim or destination of the journey…or they may be determined by immediate factors, such as whether the visible path looks easy or difficult. A path may be chosen because it is desirable, or because it is the only one remaining after others have been rejected.
The “pathway” metaphor can be as productive for studying the psychological development of persons with DSD as it has been in the much broader field of child development and developmental psychopathology. It is easy to imagine how decisions made by parents for or against early surgery, for example, might alter the path the person with a DSD takes on their personal journey. By studying a large number of people with DSD for whom different decisions were made, or who themselves made varying choices when older, it may be possible to create a “taxonomy of travellers.”
From: Psychosocial and psychosexual aspects of disorders of sex development. Cohen-Kettenis P. [2010] Best Practice and Research Clinical Endocrinology and Metabolism.
Psychosocial aspects of the treatment of gender assignment, disorders of sex development (DSDs) concern information management and communication, timing of medical interventions, consequences of surgery, and sexuality. Although outcome is often satisfactory, a variety of medical and psychosocial factors may jeopardise the psychological development of children with DSDs. This sometimes results in the desire to change gender later in life. The clinical management of gender dysphoria in individuals with DSD may profit from methods and insights that have been developed for gender dysphoric individuals without DSD. In DSD care, clinical decisions are often made with long-lasting effects on quality of life and should be based on empirical evidence. Yet, such evidence (e.g., regarding gender assignment, information management and timing of surgery) is largely non-existent.
In the field of DSD, it is important to make a distinction between the terms ‘gender identity’ and ‘gender role’. The concept of gender identity encompasses cognitive and affective components. Gender role refers to behaviours, attitudes and personality traits that a society, in a given culture and historical period, designates as masculine or feminine, that is, more typical of the male or female social role. In young children, gender role behaviour includes phenomena such as preference for same-sex versus other-sex peers, roles in fantasy play, toy interests, dress-up play and interest in rough-and-tumble play. In older children or adults, gender role is measured using personality attributes with stereotypic masculine or feminine connotations or with regard to recreational and occupational interests and aspirations.
The term transsexualism refers to a desire for complete gender reassignment originating from an experienced discrepancy between one’s gender of assignment, on the one hand, and one’s basic sense of self as a male or female, or indeterminate (gender identity), on the other. In 1973, Fisk proposed the term gender dysphoria syndrome. This term allows for the possibility that an atypical gender identity development does not always result in a complete cross-gender identity and wish for gender reassignment. Gender dysphoria is now often used to indicate the distress associated with conflicting gender identity and gender of assignment. A discrepancy between assigned gender and gender identity and/or role, however, does not always seem to be associated with distress. For this reason, more neutral terms such as gender (identity) variance, gender dissonance, gender incongruence or transgenderism are often used for the spectrum of atypical manifestations of gender identity and gender role phenomena.
From: Public understanding of intersex: an update on recent findings. Hegarty P and Smith A. [2023] International Journal of Impotence Research.
Surgical interventions on infants with intersex characteristics are considered justified by some on the grounds that they carry a high risk of intolerable stigma. However, public understanding of intersex and its medicalization are under-researched. Recent qualitative and quantitative studies of the understandings of intersex and its medicalization among people who have no particular professional or public experience of intersex have been reviewed. First, such laypeople reason about clinical dilemmas by drawing on values in similar ways as expert healthcare professionals do. Second, laypeople can over-estimate the utility of current ‘umbrella terms,’ including intersex, for people with direct familial experience of intersex. Third, beliefs about good and bad effects of medical intervention are affected by framing intersex as either a medical condition or the natural basis for a social identity. Fourth, sexual identity is the best evidenced predictor of opinions about early surgical intervention and its legal limitation on human rights grounds. Possible stigmatizing reactions from the public may not be a solid basis on which to justify early surgical intervention on intersex characteristics.
Stigma was framed as a central matter by intersex activists in the 1990s and disagreement as to whether surgical interventions deliver people with intersex variations any relief from stigma is longstanding. In 19th century medicine, a search for such patients’ “true sex” characterized clinical investigation, and determining “true sex” of an apparent “hermaphrodite” through medical interpretation carried moral implications for the person’s sexual relationships and marriage. This moralization intensified with the medicalization of sexuality at the end of the 19th century. Even as some 19th century medical professionals developed surgical interventions to “correct” intersex variations, others critiqued their colleagues’ claims that surgery delivered this benefit. In 19th century Europe, some adults with natural intersex variations were accepted by their families and communities, and their medical case histories imply fear about possible negative consequences of medical attention.
The boundary between beneficent and harmful medical intervention remains contested and morally drawn today. Whilst human rights statements assume a moral boundary between problematic interventions performed only for “cosmetic” or “normalizing” reasons, and those that are “medically essential” or “medically necessary,” contemporary healthcare professionals disagree amongst themselves about where to draw this such a moral line.
Clinicians can provide different answers to this question due to opposing psychosocial assumptions about the materiality of stigma in the lives of school-age boys, see also. Both of their answers stand on shaky ground, and either clinician could, in good faith, pass on their beliefs to parents who might reasonably interpret those beliefs as medical expertise. Whilst such parents bear the risks of stigma to their children in mind when making such decisions, neither clinician has the expertise in children’s social development to research what happens in situ at the urinal; training in paediatric urology does not provide this.
Since stigma was framed as a central matter by intersex activists in the 1990s, a number of researchers have investigated its effects in the lives of adults with intersex variations, finding that cultural norms of sexed embodiment and medically prescribed silence commonly impacted personal identity development by perpetuating shame.
Participants gave free associations to three umbrella terms, “hermaphrodite,” “intersex,” and “disorders of sex development (DSD),” and reported familiarity with those terms.
What general lessons can be drawn now?
First, lay people’s understandings of intersex and its medicalization can be researched using ordinary social science methods; focus groups, interviews, experiments, and surveys. In the course of this work, we heard experts express doubt that this work could be done ethically and with validity.
Second, is there a clear bioethical line between (good) medically necessary and (bad) cosmetic interventions on intersex variations? Laypeople, like health care professionals, can and do ground their bioethical reasoning about what is best to do when intersex variations are presented in clinical contexts in psychosocial concerns that are matters of debate and disagreement. A single essential clear line may be assumed to exist, but many such lines may be drawn in response to dilemmas.
Third, to whom—among the public–should a young person or their anxious parent turn for support? There are diverse views among the general public about whether surgical intervention on intersex characteristics and other social forms of support are good and viable things.
Fourth, can people with intersex variations hope to reduce stigmatization by sharing their personal narratives with others? Laypeople’s opinions about the medicalization of intersex, and surgical interventions on infants in particular, are not completely crystallized. Those opinions can be affected by framing intersex as either primarily a medical or psychosocial issue, with consequences for beliefs about whether genital surgery in infancy is benevolent or not. Sharing experiences may be a form of ‘contact’ that reduces prejudice toward intersex people as it reduces prejudice in many other areas.
Fifth, several intersex rights organizations who call for rights to self determination and so oppose early surgical interventions have described it as problematic that intersex and transgender groups are confused in the public mind. Whilst many laypeople do consider intersex and transgender to be analogous (or wrongly consider them identical), those laypeople who are most likely to support intersex human rights are also those who endorse the gender binary the least.
Members of the public may similarly be torn between two paradigms; traditional medical authority vs. openness to rethinking what is necessary given changing societal norms around sex characteristics and their relationship to gender norms. This vision of the public stands at odds to the traditional one in which naturally occurring intersex variations are assumed to inevitably invite unbearable stigma such that surgical intervention on those traits must be the most benevolent response to them.
SECTION C INTERSEX/DSD CONDITIONS ASSOCIATED WITH GENDER DYSPHORIA
From: Gender identity, gender assignment and reassignment in individuals with disorders of sex development: a major of dilemma. Fisher A et al. [2016] Italian Society of Endocrinology.
In many respects this research and paper acts as a baseline for the understanding of differences of Sexual Development and Gender dysphoria.
Disorders of Sex Development (DSD) are a wide range of congenital conditions characterized by an incongruence of components involved in sexual differentiation, including gender psychosexual development. The management of such disorders is complex, and one of the most crucial decision is represented by gender assignment. In fact, the primary goal in DSD is to have a gender assignment consistent with the underlying gender identity in order to prevent the distress related to a forthcoming Gen der Dysphoria. Historically, gender assignment was based essentially on surgical outcomes, assuming the neutrality of gender identity at birth. This policy has been challenged in the past decade refocusing on the importance of prenatal and postnatal hormonal and genetic influences on psychosexual development.
The normal pattern of human sexual development occurs in a highly regulated and dynamic process, dictated by intricate genetic activity, and executed by endocrine mediators in the form of steroid and peptide hormones. According to the pioneering Jost’s paradigm, the first sexual development step is constituted by the establishment of the chromosomal sex (i.e., the presence of a Y or X chromosome), at the time of fertilization. Then, the chromosomal sex influences the determination of the gonadal sex, in differentiating the bipotential gonadal ridge into either a testes or an ovary. The presence and expression of the testes-determining gene SRY, located on the distal part of the short arm of the Y chromosome (Yp), determines the gonadal sex of an embryo by directing the development of the bipotential embryonic gonad into testes, with formation of Sertoli and Leydig cells. The differentiation of male testes leads to the secretion of specific hormones responsible for translating gonadal sex into male internal and external genitalia (sex phenotype). In particular, the anti-mullerian hormone (AMH), produced by Sertoli cells, causes the regression of the Mullerian ducts and prevents the development of the uterus, fallopian tubes, and the distal portion of the vagina [5, 6]. Meanwhile, testosterone secretion from Leydig cells promotes the Wollfian duct differentiation into vasa deferentia, epididymis, and seminal vesicles.
The process of sexual differentia ion is not completed with the formation of genitalia, but also the brain, as the substrate of sexual and non-sexual behaviour, undergoes sexual differentiation consistent with the other characteristics of sex. The two crucial periods in human development when testosterone levels are known to be higher in male than in female individuals are mid-pregnancy and the first 3 months after birth. These two peaks of testosterone, together with functional changes in steroid receptors, are thought to fix (and “organize”) the structures and circuits in the brain for the rest of a person’s life. The rising testosterone levels during puberty activate and reorganize circuits that were built during development. Therefore, psychosexual development is a com plex and long-lasting process influenced by multiple factors, including brain structure, prenatal and postnatal hormonal and genetic influences, postnatal environmental and psychosocial experiences, and social and familiar circumstances, and is traditionally broken down into three domains: gender identity, gender role behaviour, and sexual orientation.
The assumption that GD could be considered a DSD is based on the demonstration in male to-female (MtF) and female-to-male (FtM) transsexuals of a sex reversal in terms of volume and cell number of sex dimorphic brain nuclei, such as the central portion of the bed nucleus of the striaterminalis (BNSTc) [38–40], the gray matter in the right putamen, and the interstitial nuclei 3 and 4 of the anterior hypothalamus (INHAH3 and INAH4). It has also been postulated that there may be genetically based systemic sex hormone abnormalities that do no cause abnormalities of the reproductive anatomy, but nevertheless influence brain and behaviour. Sexual orientation as well as gender-atypical behaviour do not affect the decision-making process in DSD gender assignment. This may explain the fact that studies addressing systematically the relationship between gender atypical behaviour and sexual orientation in DSD are missing, at the time of writing.
Interestingly, recent studies suggest that Gender Dysphoria (GD) could hypothetically be considered as a DSD limited to the central nervous system, without the involvement of the reproductive tract. GD, according to DSM-5 criteria, is a condition characterized by a marked incongruence between one’s experienced/expressed gender and the assigned one, associated with clinically significant distress or impairment in social, occupational, or other important areas of functioning. The assumption that GD could be considered a DSD is based on the demonstration in male to-female (MtF) and female-to-male (FtM) transsexuals of a sex reversal in terms of volume and cell number of sex dimorphic brain nuclei, such as the central portion of the bed nucleus of the striaterminalis (BNSTc)
Therefore, in a wider and more current perspective, DSD could be defined as all the conditions in which the chromosomal, gonadal, phenotypical or psychological (or rather gender identity) sex are incongruent [50]. Moreover, the overlap existing between DSD and GD is linked to the possibility in both conditions of discomfort or distress caused by a discrepancy between gender identity and gender assigned at birth [51, 52]. Furthermore, in both groups, such distress could lead to a possible gender reassignment request. In fact, in non-intersex persons, gender identity issues develop, even though all biological sex indicators are differentiated uniformly in the direction of one sex or of the other. These indicators include sex chromosomes, sex-determining genes, the gonads, the systemic sex hormone milieu during foetal development, puberty, and adulthood, and the secondary sex characteristics.
For many years, according to the “optimal gender policy” developed by Money, it was believed that gender identity should have been concordant with assigned sex, assuring that the child is raised unambiguously and that appropriate surgical “corrections” and hormone therapies are instituted in line with the gender chosen. This assumption was based on the belief of the neutrality of gender identity at birth, which develops its characterization on the basis of postnatal social and environment influences. This theory, assuming psychosexual neutrality at birth, has been challenged in the past decade by refocusing on the potential importance of prenatal (e.g., endocrine) and genetic influences on psychosexual development.
Theoretically, assignment should be made as quickly as a thorough diagnostic evaluation permits. Because DSD is an uncommon phenomenon, there has been limited data concerning the eventual outcomes regarding gender identity, gender role identification, or sexual orientation, and in many of these conditions, information about long-term gender development is unfortunately not syndrome-specific.
The issues that surround DSDs are multidimensional and require both an individualized and multidisciplinary approach to provide effective diagnosis, treatment, and support. The ultimate aim of treatment and care for patients with DSD are the physical, psychological, and sexual well-being within a “patient-centred” view and a continuous teamwork [93]. Considering the difference in physical appearance and the variation in developmental history, the basic processes of successful social and emotional development, as well as self-concept, may be more challenging for children and adolescents with DSD than for their peers.
Several factors related to hypospadias could expose the subject to an increased risk of psychosexual maladjustment: the stress related to a praecox genital surgery, the possible poor aesthetic and functional results of surgery procedures, and finally the abnormal prenatal androgen exposure and/or androgen receptor defects to which they have been possibly subject. It has been observed that a more pronounced masculine gender role behaviour was predicted by a younger age at final surgery. Vice versa, the number of surgeries has been found to be positively correlated with increased gender-atypical behaviour.
47,XXY Klinefelter syndrome and variants: Men with Klinefelter syndrome, which is one of the most common forms of sex chromosome aneuploidy, usually report a male gender identity. However, a recent Belgian study described a significantly higher prevalence of Klinefelter syndrome among male-to-female than expected, based on the population data. In addition, a recent study showed the presence of higher dysphoric symptoms in Klinefelter persons compared to a group of healthy controls. However, levels of GD observed were not at critical threshold to suggest a GD diagnosis and should be better considered in light of the dimensional construct of GD. Moreover, moderator analyses showed that gender dysphoric symptoms observed in Klinefelter population might be an epiphenomenon of the autistic traits. However, it should be recognized that GD in Klinefelter syndrome has not been systematically studied in large samples, and it is possible that not all karyotype variations have been reported by other gender teams, specifically in relation to the finding of Klinefelter syndrome.
The suggested strategy for gender assignment of a newborn with genital ambiguity should not be based only on the appearance of the genitalia at birth, as the degree of genitalia virilization does not necessary correlate with the degree of brain masculinization. In fact, there are temporal trends in gender assignment that are independent of this external appearance.
In conclusion, it should be taken into account that every DSD subject is unique and has to be treated with individualized care. Researches for further understanding of specific outcomes are needed. In this perspective, international registries (e.g., I-DSD Registry, DSD-Life, DSD-net, and DSD-TRN) are crucial to improve the understanding of these challenging conditions and clinical practice, in providing a better prediction of gender identity and common clinical procedures.
From: Differences/Disorders of Sex Development: Medical Conditions at the Intersection of Sex and Gender. Sandberg D and Gardner M [2022] Annual Review of Clinical Psychology.
Defined as congenital conditions in which development of chromosomal, gonadal, or anatomic sex is atypical, differences or disorders of sex development (DSDs) comprise many discrete diagnoses ranging from those associated with few phenotypic differences between affect ed and unaffected individuals to those where questions arise regarding gender of rearing, gonadal tumor risk, genital surgery, and fertility. Controversies exist in numerous areas including how DSDs are conceptualized, how to refer to the set of conditions and those affected by t hem, and aspects of clinical management that extend from social media to legislative bodies, courts of law, medicine, clinical practice, and scholarly research in psychology and sociology. In addition to these aspects, this review covers biological and social influences on psychosocial development and adjustment, the psychosocial and psychosexual adaptation of people born with DSDs, and roles for clinical psychologists in the clinical management of DSDs.
Medical conditions—or categories of them, as in the case of differences or disorders of sex development (DSDs) —are rarely the focus of topic reviews in the Annual Review of Clinical Psychology. Yet print, broadcast, and social media have raised public awareness of people identifying as intersex. What is the relationship between intersex and the medical conditions falling under the umbrella term DSD? What are the biological origins of DSDs? And how are DSDs specifically relevant to clinical psychology? Nonspecialist health care providers and the public are more likely to see and hear the terms intersex or LGBTI than DSD. Similarly, it is likely that people have heard of women Olympians with an XY karyotype who have been disqualified from competition because of “naturally elevated” testosterone.
There are also reports by international governmental and nongovernmental organizations challenging medical standards of care for people born with medical conditions that fall under the DSD umbrella; some of these standards have been equated to a form of torture according to the UN Human Rights Council. Finally, disputes regarding medical care received by individuals born with atypical sex anatomies have played out in courts of law Western societies demonstrate increasing acceptance of men and women who cross conventional gender and sexual expression boundaries. Yet, when it comes to biological sex, societies lack frameworks—legal or otherwise—to accommodate anatomies that challenge the male–female binary
Variations in genetic or hormonal determinants of somatic sex development can result in a newborn with characteristics that do not fit neatly into either the male or female category. It is frequently, but mistakenly, assumed that the term DSD necessarily implies ambiguity in external genital appearance. This is not a definitional requirement. DSDs can present with a wide range of genital phenotypes depending on the specific condition and its expression. Most children born with DSDs are identified soon after birth because of visible genital differences, health concerns [e.g., a positive newborn screening test for congenital adrenal hyperplasia (CAH)], or discordance between prenatal genetic testing, diagnostic ultrasound, and the newborn’s apparent sex. However, some DSDs may not be detected until later when an inguinal hernia is identified, a girl fails to ever menstruate (i.e., primary amenorrhea), or an adult experiences infertility. A commonly cited estimate of DSD incidence is 1:4,500 live births, but estimates as high as 1% are used when conditions considered borderline f or inclusion are counted.
Sex determination begins at 6 weeks: Sex chromosomes (XX or XY) guide bipotential gonads to develop into testes or ovaries. The SRY (sex-determining region Y) gene on the Y chromosome triggers a cascade of genetic signalling events resulting in development of the testes. Development of ovaries was once believed to be the default process [i.e., an ovary develops in the absence of a Y chromosome (and SRY)]; current understanding shows ovarian development is also an active process requiring activation of genes that promote ovarian, and interfere with testicular, development. A major consequence of deviation in typical sex determination includes development of atypic al sex anatomy.
Important distinctions between transsexualism/transgenderism and DSDs can become blurred in both popular and scientific literature. People who identify as transsexual or transgender are characteristically born with typical male or female sex chromosomes, go nads, and anatomy but experience a mismatch between their somatic sex and their experienced gender identity. In contrast, a DSD is a consequence of atypical development of sex chromosomes, gonads, or sex anatomy. Although individuals born with DSDs may share experiences with transgender individuals (e.g., gender dysphoria incidence is higher in individuals with DSDs than in the general population), DSD’s expose affected persons to saliently different life events. In other words, these are distinct populations; one should not simply apply lessons learned from research and clinical experience with the transgender population to the DSD population (or vice versa).
Sex hormones (e.g., androgens and oestrogens) influence behaviour via two routes: organizational and activational effects. Organizational effects occurring early in development cause permanent changes to brain structure and physiology that produce long-lasting changes to behaviour. Activational effects produce temporary changes to the brain, affecting behaviour only when sex hormones are present (Berenbaum & Meyer-Bahlburg 2015). A substantial experimental research literature in nonhuman animals demonstrates that sex hormones present during early development produce long-lasting effects on behaviours that exhibit sex differences—for instance, learning and memory, aggression, play, and sexual behaviour ( Berenbaum & Beltz 2011). Early programming influences of sex hormones occur during species-specific sensitive periods of prenatal or neonatal life; sex hormones do not have the same effect if exposure occurs before or after this period. There is strong evidence human behaviour is also influenced by hormones present during prenatal development, particularly androgens. Sex hormones continue to organize the brain well beyond the prenatal and early neonatal periods, with later periods of brain organization building upon and refining neural circuits established during earlier development.
Challenges germane (though not exclusive) to DSDs include accessing balanced and authoritative information, stress associated with the birth of a child for whom gender of rearing is not obvious, anticipated stigma, and evaluating what constitute the best interests of the child in the process of clinical decision making. Parents are often unaware DSDs exist until they receive their child’s diagnosis. Unfamiliarity with DSDs, lack of clear information, and cognitive confusion contribute to stress and feelings of isolation.
Prior to these legislative efforts, activists who equated genital surgery to torture worked with the United Nations (UN) High Commissioner for Human Rights and the UN Special Rapporteur on Torture and Other Cruel, Inhuman or Degrading Treatment or Punishment to “repeal any law allowing intrusive and irreversible treatments, including forced genital-normalizing surgery” When asked to “affirm that medically unnecessary surgeries in individuals born with differences of sex development are unethical and should be avoided until the patient can actively participate in decision-making” and to “oppose the assignment of gender binary sex to infants with differences in sex development through surgical intervention outside of the necessity of physical functioning for an infant and [recognize that] children should have meaningful input into any gender assignment surgery,” in 2019, the Council on Ethical and Judicial Affairs of the American Medical Association (AMA) declined to do either.
DSDs share several aspects with other conditions, including congenital conditions (generally) and chronic illnesses, as well as issues pertaining to LGBT communities; however, the issues are not one and the same and require careful thought regarding the application of lessons learned in these areas to DSDs. Issues commonly affecting the DSD community include information about specific conditions and/or aspects of care that are lacking, conflicted, or anxiety-provoking; parental stress; stigma, shame, and secrecy; legal and ethical questions in paediatric care surrounding consent, assent, child rights, and parental responsibilities, largely in regard to surgical procedures; influence of religion and culture; and nosocomial trauma. Psychosocial and psychosexual adaptation in DSDs can differ from that in unaffected persons regarding experienced stigma and shame, psychological and social problems, experiences and preferences regarding genital surgery, psychosexual milestones and sexual function, sexual orientation, and gender dysphoria. R
Roles and considerations for clinical psychologists within multispecialty team care include the following: integrate with other specialists caring for the patient/family; in clinical assessment and intervention, balance a noncategorical approach, which assumes that patients and families are influenced by a similar set of factors that affect adaptation in general, with condition-specific knowledge (e.g., needs for medication or regular screening for tumor risk) gleaned from the full range of specialty team providers; educate patients, families, and health care provider colleagues about the implications of medical conditions for quality of life and strategies to address quality of life concerns; within SDM, promote patient self-efficacy (in paediatrics, based on developmentally qualified understanding of one’s condition)—for instance, choosing how the person wants the genital exam to be performed; and promote psychologically informed research—both in its conduct and uptake to inform practice.
The Link With DSD’s and DES.
Disorders of Sex Development (DSDs) is a broad category of congenital conditions, whereas Diethylstilbestrol (DES) is a specific environmental factor—an endocrine-disrupting chemical—that can cause certain DSDs. In essence, DES exposure in the womb is a known cause of specific types of DSDs. Disorders of Sex Development refer to a range of medical conditions in which the development of chromosomal, gonadal, or anatomical sex is atypical. DSDs have various origins, including:
Genetic factors: These include gene mutations or changes in sex chromosomes.
Hormonal disruptions: These can result from enzymatic defects in hormone production or exposure to external chemicals.
Maternal factors: These can influence foetal development.
DES: A specific cause of DSDs: Diethylstilbestrol (DES) is a synthetic oestrogen that was widely prescribed to pregnant women from the 1940s to the 1970s to prevent miscarriages. Its use was discontinued after it was linked to severe reproductive problems in the offspring of those who took it, making it the first identified transplacental carcinogen in humans. Exposure to DES in utero acts as a potent endocrine disruptor, interfering with normal foetal sex differentiation and causing a range of DSDs.
The link between DES exposure and DSDs is seen in the different effects on “DES daughters” and “DES sons”.
In “DES daughters” (females exposed in utero):
Reproductive tract abnormalities: These include a T-shaped or hypoplastic uterus, cervical abnormalities, and vaginal adenosis. These structural differences are a specific manifestation of a DSD.
Fertility issues: The reproductive tract malformations and other functional problems can lead to an increased risk of infertility, ectopic pregnancy, and preterm delivery.
In “DES sons” (males exposed in utero):
Genital abnormalities: Abnormalities such as epididymal cysts, cryptorchidism (undescended testicles), and hypospadias (abnormal location of the urethral opening) are more common in DES-exposed males. These are considered forms of DSD.
Testicular inflammation/infection: Studies also show an increased risk of testicular inflammation and infection.
Hypogonadism: Some evidence suggests a link between prenatal DES exposure and hypogonadism, which is a condition involving low testosterone levels.
In summary, DSD is the broader medical classification for atypical sex development, while DES is a proven environmental trigger that can induce specific, identifiable forms of DSD by disrupting hormonal signalling during foetal development.
Additional sources:
Ambiguous Genitalia in the Newborn – Endotext – NCBI Bookshelf
Psychological aspects of the treatment of patients with disorders of sex development – PubMed
Androgen Insensitivity Syndrome – GeneReviews® – NCBI Bookshelf
Androgen insensitivity syndrome – The Lancet
Ambiguous Genitalia and Disorders of Sexual Differentiation – StatPearls – NCBI Bookshelf
Psychosocial and psychosexual aspects of disorders of sex development – ScienceDirect (Journal?)
Public understanding of intersex: an update on recent findings | International Journal of Impotence Research
Key References
{NEW} (Notable) *** The epidemiology of disorders of sex development
(2025), by Agnethe Berglund,et al., published in Best Practice & Research Clinical Endocrinology & Metabolism
*** Prevalence of disorders of sex development in patients with hypospadias and cryptorchidism (2025), by Callum Lavoie, et al., published in Journal of Pediatric Urology
*** (Notable) Disorders of Sex Development (DSD): A more than three Decades of Experience at a Major Teaching Hospital (2024), by Nasir A M Al-Jurayyan, et al., published in Journal of Clinical Endocrinology & Metabolism
*** The Development of Legal Rights for Intersex Persons: Part I: The Diversity of Intersex Conditions (2024), by Alan R. Felthous & Chanchal Kahlon, published in Behavioral Sciences and the Law
(Notable) *** Prevalence of Intersex/Differences in Sex Development and Primary Gonadal Insufficiency in a Pediatric Transgender Population
(2024), by Hari Randhawa, et al., published in Transgender Health
*** Ambiguous Genitalia in the Newborn (2023), by Christa E. Flück and Tülay Güran, published in Endotext
*** Androgen Insensitivity Syndrome: A Review (2023), by E. Delli Paoli, et al., published in Journal of Endocrinological Investigation
*** Sexuality and fertility desire in a large cohort of individuals with 46, XY differences in sex development (2023), by Rafael Loch Batista, published in the journal Clinics
(Notable) *** Differences/Disorders of Sex Development: Medical Conditions at the Intersection of Sex and Gender (2022), by David E. Sandberg and Melissa Gardner, published in Annual Review of Clinical Psychology
*** Hypospadias and Increased Risk for Psychiatric Symptoms in Both Childhood and Adolescence: A Literature Review (2022), by Tingting Jin, et al., published in Frontiers in Psychology
(Notable) *** 46,XY Differences of Sexual Development (2022), by Sorahia Domenice, et al., published in Endotext
*** Gender and Sexuality in Disorders/Differences of Sex Development (2022), by Baudewijntje P. C. Kreukels & Tim C. van de Grift, published in the book Gender and Sexuality Development: Contemporary Theory and Research
*** Sexual Self-Concept in Women with Disorders/Differences of Sex Development (2022), by Nita G. M. de Neve-Enthoven, et al., published in Archives of Sexual Behavior
*** Patients with Disorders of Sex Development (2021), by Renata Markosyan, published in Annals of Pediatric Endocrinology & Metabolism
*** The Challenges of Androgen Insensitivity Syndrome (2021), by Bratu Ovidiu, et al., published in Archives of Medical Science
*** Congenital Adrenal Hyperplasia—Current Insights in Pathophysiology, Diagnostics, and Management (2021), by Hedi L Claahsen – van der Grinten, et al., published in Endocrine Reviews
(Notable) *** Hypogonadism and Cryptorchidism (2020), by Wiwat Rodprasert, et al., published in Frontiers in Endocrinology
*** Disorders of Sex Development: Classification, Review, and Impact on Fertility (2020), by Pedro Arcien, published in Journal of Clinical Medicine
*** Puberty in individuals with a disorder of sex development (2020), by Anna Nordenström, published in Current Opinion in Endocrine and Metabolic Research
*** Disorders of Sexual Development in Newborns (2019), by Mabel Yau, et al., published in Endotext
(Notable) *** Management of 46,XY Differences/Disorders of Sex Development (DSD) Throughout Life (2019), by Amy B Wisniewski, et al., published in Endocrine Reviews
*** Psychosexual Aspects, Effects of Prenatal Androgen Exposure, and Gender Change in 46,XY Disorders of Sex Development (2019), by Rafael Loch Batista, et al., published in The Journal of Clinical Endocrinology & Metabolism
*** Mental Health Status of Individuals with Sexual Development Disorders: A Review (2019), by M. Bohet, et al., published in Journal of Pediatric Urology
*** Androgen Insensitivity Syndrome: A Review (2018), by Rafael Loch Batista, et al., published in Archives of Endocrinology & Metabolism
*** Caring for Individuals with a Difference of Sex Development (DSD):
A Consensus Statement (2018), by Martine Cools, et al., published in Nature.com
(Notable) *** Gender identity, gender assignment and reassignment in individuals with disorders of sex development: a major of dilemma (2016), by A. D. Fisher, et al., published in Journal of Endocrinological Investigation
*** Psychosexual Development in Adolescents and Adults with Disorders of Sex Development—Results from the German Clinical Evaluation Study (2013), by Martina Jürgensen, et al., published in The Journal of Sexual Medicine
(Notable) *** Psychological Aspects of the Treatment of Patients with
Disorders of Sex Development (2012), by David E. Sandberg, et al., published in Seminars in Reproductive Medicine
*** Male Gender Identity in Complete Androgen Insensitivity Syndrome (2011), by Guy T’Sjoen, et al., published in Archives of Sexual Behavior
*** Health-Related Quality of Life, Mental Health and Psychotherapeutic Considerations for Women Diagnosed with a Disorder of Sexual Development: Congenital Adrenal Hyperplasia (2010), by Matthew A. Malouf, et al., published in International Journal of Pediatric Endocrinology
(Notable) *** Psychosocial and psychosexual aspects of disorders of sex development (2010), by P.T. Cohen-Kettenis, published in Best Practice & Research Clinical Endocrinology & Metabolism
*** 46,XY disorders of sex development – the undermasculinised male with disorders of androgen action (2010), by Ralph Werner, et al., published in Best Practice & Research Clinical Endocrinology & Metabolism
*** Developmental endocrine influences on gender identity: implications for management of disorders of sex development (2006), by William Byne, published in Mt. Sini Journal of Medicine
*** Hypospadias: a transgenerational effect of diethylstilbestrol? (2006), by M.M. Brouwers, et al., published in Human Reproduction
(Notable) *** Hypospadias in sons of women exposed to diethylstilbestrol in utero: a cohort study (2002), by Helen Klip, et al., published in The Lancet
>> (Chapter 25) What are some examples of studies of personal narratives in the evolution of self-discovery about gender identity?
Overview by Ian Cameron
From: Coming Into Identity: How Gender Minorities Experience Identity Formation. Nordmarken S. [2023] Gender and Society. Sage Journals.
Previous studies have found that trans people claim to have consistent gender identities over their lifetimes. As a result, scholars know little about processes through which individuals come to identify differently from their gender assignment. In this article, I analyze how gender minorities in the United States come to identify with new labels, theorizing gender-identity formation as a social process. Despite pressure to present oneself as “trans enough” and despite many individuals’ claims to “always have been” the ways they
are, most research participants’ stories illustrate a process of gender-identity change—what I term coming into identity. Coming into identity is the process whereby individuals come to understand themselves in new ways despite living in epistemological systems and constructed realities where such ways of understanding oneself are not widely acknowledged. I find that participants’ coming-into-identity experiences involved self-reflection in relation to:
(1) exposure to new gender conceptualizations and models,
(2) gender experimentation,
(3) difficult experiences, and/or
(4) conversations with others.
The idea that identity is an innate essence is dominant in mainstream culture and prominent LGBTQ+ narratives. I term this idea the innate-essence identity model. This idea operates in the “coming out of the closet” metaphor, which presupposes that a person has always had the stigmatized identity they are disclosing. The metaphor does not address how one came to identify in such a way, despite the social construction of sexual and gender categories
and the social process of learning about them. The most common example is the “born in the wrong body” metaphor—what gender-minority communities call the “wrong body narrative.” Conceptualizations of trans identity that adhere to binary, “wrong body” thinking reflect transnormativity, a form of gender normativity. Trans people often hold themselves and each other accountable to transnormative standards. To be considered “trans enough,”
gender minorities attempt to conform to the transnormative narrative.
Despite being raised in the gender associated with their assigned sex, most participants recalled memories of childhood gender difference. More than two-fifths of participants claimed consistent feelings over time about their gendered selves. These patterns suggest that the innate-essence identity model persists, but the fact that a minority of participants claimed consistent feelings over time means that gender identity, for most, has changed.
Importantly, most participants discussed the circumstances under which they came into their gender identities. Regardless of whether they experienced childhood gender difference, almost all participants described a process of self-reflection whereby they gained an enhanced understanding of their gendered selves. Most also described one or more of four experiences, which co-occurred with and/or led to their self-reflection:
(1) exposure to gender minorities and/or information about them,
(2) gender experimentation,
(3) an emotionally difficult period or event, and
(4) conversations with others.
These patterns suggest that the expansive gender-identity discourse’s dissemination facilitated coming-into-identity experiences. The data also enhance our understanding of the expansive gender-identity discourse. In addition, coming-into-identity stories’ pervasiveness suggests that a distinct coming-into-identity narrative operates alongside the “wrong body” narrative. In the following pages, I present participants’ experiences of
coming into identity and the persistence and change I have observed in the innate-essence identity model, as represented in participants’ self-stories.
The innate-essence identity model structures the cisnormative epistemological environment in which gender minorities must attempt to attain social legitimacy. Because this environment privileges cisgender identities and assumes that sex equals gender, gender minorities constantly face the threat of a challenge to their identity, with potentially devastating consequences. Cisnormative perspectives, casting gender minorities as unnatural, deceitful, and dangerous, justify marginalization and violence against them. Medical and legal gatekeepers have established their authority to discredit nontransnormative narratives and withhold care and services. In this context, claiming “sameness” to social norms is a strategy for navigating social life and pursuing civil rights and medical care. Gender minorities’ innate identity claims can be understood as a deployment of dominant discourse and master story-patterns about gender and the self—cisnormative discursive and narrative structures—as resources to obtain legitimacy in a cisnormative society. The innate-essence identity model structures the cisnormative epistemological environment in which gender minorities must attempt to attain social legitimacy. Because this environment privileges cisgender identities and assumes that sex equals gender, gender minorities constantly face the threat of a challenge to their identity, with potentially devastating consequences. However, some individuals challenge the dominant gender discourse. Gender minorities in the 1990s began to contest the innate-essence identity model through political critique and by creating new, alternative ideas about gender and themselves, resisting both cisnormativity and transnormativity. They conceptualized gender without a binary structure
and consisting of many varied and fluid identities not tied to biology. Using primarily print media to circulate their ideas, these intellectual rebels pushed toward a new discourse that problematized existing gender conceptions and expanded possibilities for new gender conceptualizations, experiences, and identities to come into being. Midlife reckoning experiences also led to identity realizations. A traumatic event prompted self-reflection in half of participants who experienced midlife reckoning. With or without trauma, midlife reckoning involved realizing that an unsatisfactory aspect of one’s life was about gender. Decisions to initiate gender changes typically were made with a desire for
happiness and an awareness that time was limited, which spurred the decision.
Unlike the idea of coming out, the idea of coming into identity does not presuppose innate identities; instead, it challenges the innate-essence identity model. Coming into identity is a process of gender-identity change whereby individuals come to understand themselves in new ways, despite living in epistemological systems and constructed realities where such ways of understanding oneself are, for the most part, not acknowledged or understood, but are erased.
From: Creating gender: A thematic analysis of genderqueer narratives. Bradford N et al. [2020]. International Journal of Transgenderism.
Participants described “genderqueer” as a sufficiently broad category to capture their diverse experiences, and descriptions of genderqueer identities were heterogeneous, directly contradicting binary understandings of gender identity. A thematic analysis of interview transcripts resulted in three themes: intrapsychic experience, descriptions of master narratives about gender identity, and the co-construction of identities. Participants described navigating a series of master and alternative narratives, such that all
transgender people transgress a cisnormative master narrative, but genderqueer people further transgress normative understandings of a medicalized, binary transgender identity. The experience of co-creating identities was the process by which participants actively navigated constraints of the master narrative experience. Participants described the integral
role of language in crafting new narratives to legitimize genderqueer experiences, as well as the subsequent intragroup conflict resulting from conflicting relationships to narratives in the transgender community. This study highlights genderqueer identities as a source of strength and positivity, and the importance of expanding beyond the hegemonic gender
binary within research and clinical practice.
From: Non-Binary Gender Identities – The Language of Becoming. Cordoba S. [2022]. Routledge.
Non-Binary Gender Identities examines how non-binary people discover, adopt, and negotiate language in a variety of social settings, both offline and online. It considers how language, in the form of gender-neutral pronouns, names, and labels, is a central aspect of identity for many and has been the subject of much debate in recent years. Cordoba captures the psychological, social, and linguistic experiences of non-binary people by illustrating the multiple, complex, and evolving ways in which non-binary people use
language to express their gender identities, bodies, authenticity, and navigate social interactions – especially those where their identities are not affirmed. These findings shed light on the gender and linguistic becomings of non-binary people, a pioneering theoretical framework developed in the book, which reflects the dynamic realities of language, subjectivities, and the materiality of the body. Informed by these findings, the text offers recommendations for policy makers and practitioners, designed to facilitate gender-related
communication and decrease language-related distress on non-binary people, as well as the general population.
This important book advances our understanding of non-binary gender identities by employing innovative methodologies – including corpus-based research and network visualisation – furthering and developing theory, and yielding original insights. It is essential reading for students and academics in social psychology and gender studies, as well as anyone interested in furthering their understanding of non-binary gender identities. Gender and sex are different constructs within psychological re search and are unreservedly
more complex than the common conception. Gender has typically been understood as “a social and psychological construct used to describe one aspect of how we experience ourselves in a world where the category ‘gender’ is made to matter” whereas sex is typically “based on the presence of external genitalia”. Thus, one is abstract and socially constructed (gender) while the other one is physical and biological (sex). Within psychology, Stoller (1968) has been credited with distinguishing between sex and gender identity, arguing that the former is a product of nature while the latter one is a product of nurture. As such, Stroller introduced the term “gender identity,” which illustrated that “sex and gender are not inevitably bound … each may go in its quite independent way” and that one’s sense of gender identity may be different than one’s biology. Kessler and McKenna (1978), however, made the case that, while sex and gender are independent constructs, they relate to one
another as mind, society, language, and body are indeed all interrelated. While sex and gender typically correlate, both constructs are multidimensional and bimodal rather than linear and binary. Historically, sex has been understood as the biological components that make up maleness and femaleness, typically differentiated in terms of chromosomes, gonads, hormones, internal reproductive systems, external genitals and, according to some
research, brain.
The sex someone is assigned at birth based on their visible sex characteristics (i.e., having a penis or a vagina, and sometimes intersex) may not always “align” with their gender identity throughout their life, as is the case with trans people. Trans (the abbreviated form of the word transgender) is often used as an umbrella term for people who do not identity as the gender they were assigned at birth. While the focus of this book is on non-binary gender identities and the numerous and heterogenous ways in which gender can be experienced and articulated, it is important to illustrate some of the ways in which “sex” is also as diverse. The endosexist perspective of sex stipulates– and prioritises – sex as an immutable binary system. However, intersex
people demonstrate that sex is far from binary. Intersex refers to a wide range of biological sex variations that include chromosomes, hormones, primary or secondary sex characteristics, among others. According to Fausto-Sterling, some of the most common intersex conditions include, but are not limited to:
- Congenital Adrenal Hyperplasia: A genetically inherited malfunction which affects the production of steroids. It can cause masculinisation of genitalia in XX children.
- Androgen Insensitivity Syndrome: A genetically inherited malfunction which affects the reception of testosterone. XY children with this condition are typically born with highly feminised genitalia and develop a feminine body shape during puberty.
- Gonadal Dysgenesis: An umbrella term for a variety of conditions where gonads do not develop customarily, typically affecting XY people.
- Klinefelter Syndrome: A form of gonadal dysgenesis wherein males have an extra X chromosome (XXY). Adults are typically infertile and may develop breasts.
- Turner Syndrome: Another form of gonadal dysgenesis wherein females lack a second X chromosome (XO). As a result, children develop neither secondary sex characteristics nor ovaries. Intersex people and their sexed bodies do not entirely fit the constructed binary notions of
the body. For example, a male-identified intersex person might have a uterus and not a penis. While it is estimated that 1–2% of the population is intersex, these conditions might not be detected until later in life (when people try to become pregnant, for instance) or might not be detected at all.
Key Literature References
(Notable) *** Coming Into Identity: How Gender Minorities Experience Identity Formation (2023), by Sonny Nordmarken, published in Gender & Society
*** Discovering gender and coming out: The gender identity journeys and coming out stories of transgender and gender expansive youth (2022), by Michelle N. Saltis, published in Journal of LGBTQ Issues in Counseling
*** Non-Binary Gender Identities: The Language of Becoming (2022), edited by Sebastian Cordoba
(Notable) *** Creating gender: A thematic analysis of genderqueer narratives (2020), by Nova J. Bradford, et al., published in the International Journal of Transgenderism
*** What’s the Story? Exploring Online Narratives of Non-binary Gender Identities (2016), by Tracey Yeadon-Lee, published in The International Journal of Interdisciplinary Social and Community Studies
>> (Chapter 26) What published research has investigated possible association between autism and variations in gender identity?
Background, by Ian Cameron
Over the past twenty years, the literature has highlighted the frequency of the association of transidentities and autism, proposing numerous theories to explain this observation, describing the characteristics of transidentities in people with autism, studying their psychiatric co-occurrences and recommending specialised care. A growing number of studies are emerging, including meta-analysis affirming higher prevalence of this co-occurrence.
Nonetheless, studies about the specifics of this co-occurrence in terms of clinical and social consequences and the particularities of specialised care are sparse. No systematic review exists to propose an inventory of the existing knowledge. So it is contested.
Is being both autistic and transgeder an example of co-occurece, indicating a link, or can these conditions occur at the same time, and yet with no link? Could it be that autistic people are more prepared to question and explore their gender identity due to the fact they either question or don’t recognise the societal norms?
A study at Princeton found DNA glitches can determine subtypes before or after a child is born, and autism subtypes differ in the timing of genetic switches, which guide distinct stages of development.
Aviya Litman, a PhD student at Princeton University and co-lead author, said: ‘These findings are powerful because the classes represent different clinical presentations and outcomes, and critically, we were able to connect them to distinct underlying biology.’ Researchers have determined that common gene variants account for only around 20 percent of ASD diagnoses, leaving the remaining 80 percent to a complex interplay of environmental factors, modifications to DNA that regulate gene expression, and gene-environment interactions that scientists still don’t fully understand. Being Transgender also has genetic origins, is there a genetic link?
From: The Autistic Trans Guide To Life. Purkis Y and Lawson W. 2027. Jessica Kingsley Publishers.
This empowering guide supports autistic trans and non-binary adults with practical tools, personal stories, and evidence-based advice to navigate life with pride and authenticity. Covering topics like self-advocacy, mental health, masking, and transitioning, it promotes self-acceptance and resilience. Written by two autistic trans activists, it offers honest, affirming insights into living as one’s true self.
Blending personal accounts with evidence-based insights and up-to-date information, and written from a perspective of empowerment and self-acceptance, the book promotes pride, strength and authenticity, covering topics including self-advocacy, mental health and camouflaging and masking as well as key moments in life such as coming out or transitioning socially and/or physically.
From: Transidentities and autism spectrum disorder: A systematic review. Bouzy J et al. [2023]. Psychiatry Research Science Direct.
Transidentity and autism frequently co-occur. Previous reviews have focused mainly on frequencies. A systematic review was conducted to condense all the studies and themes on this co-occurrence and to offer a global view. 5 main themes were identified (sex ratio, theories, sexual orientation, clinical and social consequences, and care implications) in addition to frequencies. Many theories have been proposed to explain the co-occurrence. One posits that social difficulties related to autism would lead to less identification with gender norms and less pressure to conform to these norms, allowing for greater gender diversity in people with autism.
Given their difficulties with social interactions and communication, the announcement of one’s transidentity to one’s social group is often discredited, increasing the risk of suffering and delayed care. Many reports reaffirm the importance of providing specialised care for transgender people with autism. Autism is not a contraindication for gender-affirming treatment. However, some cognitive specificities can affect the planning of care, and transgender people with autism are at high risk of discrimination and harassment.
Transidentities refer to all gender identities that do not conform to the gender assigned at birth. According to the Diagnostic and Statistical Manual of Mental Disorders, 5th version (DSM-5) (American Psychiatric Association, 2013), gender dysphoria (GD) comprises the notion of perceived suffering or impairment in the social field experienced by a transgender person. In the International Classification of Diseases, 11th version (ICD-11) (World Health Organisation, 2020), transidentities are referred to as “gender incongruence” and are no longer considered a mental disorder but a sexual health condition. Indeed, transidentities are no longer seen as a medical condition but as a singular construction of identity within human diversity.
Autism is a neurodevelopmental disorder characterised by difficulties with social interactions and verbal and nonverbal communication, restricted and stereotyped activities and interests, and sensory features. In the DSM-5 (American Psychiatric Association, 2013) and ICD-11 (World Health Organisation, 2020), autism is referred to as “autism spectrum disorder” (ASD), which is defined by persistent deficits in initiating and maintaining reciprocal social communication and social interactions and restricted and repetitive patterns of behaviours, interests and sensory activities that are atypical or excessive for the individual’s age and/or sociocultural environment.
Regarding the frequencies of autism in trans populations and of transidentity in people with autism, the results are quite heterogeneous but show an overrepresentation of this cooccurrence.
From: Associations between autism, gender dysphoria and gender incongruence: insights from the Swedish Gender Dysphoria Study (SKDS) Ozel F et al [2025] Psychiatry Research Science Direct.
High levels of autistic traits have been reported among TGD people across age groups, using a variety of ASD screening tools (Huisman et al., 2024; Kung, 2020; Lehmann et al., 2020; van der Miesen et al., 2018a; Vermaat et al., 2018; Warrier et al., 2020). Studies using self-reported diagnoses and information from health records and registers have also demonstrated increased rates of ASD among TGD people in comparison to general or cisgender populations (David et al., 2025; Heylens et al., 2018; Mahfouda et al., 2019; Strauss et al., 2021).
When investigating the potential connection between TGD identities and ASD, focusing on people experiencing gender dysphoria is particularly important, as the co-occurrence with ASD may pose certain challenges, including difficulties in obtaining a diagnosis and accessing gender-affirming treatments (Strang et al., 2023)
The results support the previously proposed co-occurrence of ASD and gender dysphoria in the literature. There is no consensus regarding the underlying mechanisms of the high co-occurrence of ASD and gender dysphoria. Different factors, including biological, psychological, and social, have been proposed to explain this co-occurrence (van der Miesen et al., 2016). Among the biological hypotheses, the extreme male brain (EMB) theory has been frequently cited in previous studies (Wattel et al., 2024). According to the EMB theory, females tend to have a greater inclination toward empathizing, while males are generally more inclined toward systemizing, and autistic people show more male patterns (Baron Cohen, 2002). Additionally, higher prenatal testosterone levels were proposed to lead to autistic traits and gender dysphoria (Auyeung et al., 2009; Jones et al., 2012).
Apart from biological hypotheses, the literature has discussed differences in gender development between autistic and neurotypical people, obsessions originating from autistic traits and rigid thinking among individuals with gender dysphoria, and mentalizing impairments among autistic people leading to symptoms of gender dysphoria (Wattel et al., 2024).
The present study demonstrates that the prevalence rates of ASD diagnoses and autistic traits are higher among people with gender dysphoria compared to cisgender people.
From: Autism Spectrum Disorder and Gender Dysphoria/Incongruence. A systematic Literature Review and Meta-Analysis. Kallitsounaki A and Williams D [2022} Journal of Autism and Developmental Disorders.
The suggested overlap between autism spectrum disorder (ASD) and gender dysphoria/incongruence (GD/GI) has been much disputed. This review showed a relationship between ASD traits and GD feelings in the general population and a high prevalence of GD/GI in ASD. Meta-analyses revealed that the pooled estimate of the prevalence of ASD diagnoses in GD/GI people was 11% (p < .001) and the overall effect size of the difference in ASD traits between GD/GI and control people was significant (g = 0.67, p < .001). Heterogeneity was high in both meta-analyses. The chances that there is not a link between ASD and GD/GI are negligible, yet the size of it needs further investigation.
From the studies reviewed it was estimated that the positive rates for ASD caseness in GD/GI people range from 1.2 to 68% (e.g., Akgül et al., 2018; Vermaat et al., 2018). The prediction intervals of the prevalence estimate were very wide, indicating that not all GD/GI people are affected by ASD to the same degree. Based on the characteristics of the literature pertaining to the prevalence of ASD diagnoses/ASD traits in GD/GI individuals, as discussed hereunder, wide prediction intervals were expected.
Furthermore, the findings reviewed indicated that GD/GI children have higher ASD traits than control children (e.g., Akgül et al., 2018; Skagerberg et al., 2015). Yet, mixed evidence emerged about the difference in ASD traits between GD/GI adults and nonclinical/population-based control adults (e.g., Nobili et al., 2018; Stagg & Vincent, 2019; Warrier et al., 2020).
Taken together, results from the literature review and the meta-analyses indicate that the chances there is not a link between ASD and GD/GI are negligible, yet absolute conclusions about the size of the link cannot be drawn.
It is also important to note that the high co-occurrence between ASD and GD/GI is underrecognized among health care professionals (Murphy & Livesey, 2017). Evidence about a link between ASD and GD/GI might stimulate the development of appropriate trainings to raise their awareness (Strauss, et al., 2021), so that GD/GI people are screened for ASD and autistic people for gender related issues.
The findings of the current literature review and meta-analyses suggest that there is:
(a) a positive relationship between ASD traits and GD/GI feelings among people from the general population,
(b) an increased prevalence of GD/GI in the autistic population, and
(c) an increased prevalence of ASD diagnoses and ASD traits in the GD/GI population. Overall, these findings suggest the existence of a link between ASD and GD/GI that warrants the investigation of mechanisms that could explain that link and the intensification of clinical attention to autistic GD/GI individuals.
From: Gender Discomfort and Autism. Lawson W. [2023] Autism Research Institute.
Literature on the intersection of autism and GDC has increased substantially in the last seven years. Early studies revealed that autistic individuals report higher rates of gender diversity than the non-autistic population (Glidden et al., 2016; Van der Miesen et al., 2016; George & Stokes, 2017). Consequently, autistic individuals also experience lower identification and fewer positive feelings about assigned gender groups which can lead to GDC. This is especially true for those assigned female at birth (Cooper et al., 2018).
Research also suggests that this relationship is bidirectional, where the rate of autism in transgender individuals is between 6 – 26% compared to a 1.85% prevalence in the general population (Thrower et al., 2020; Maenner et al., 2020; Walsh et al., 2018). Although research on the co-occurrence of autism and GDC is widely available, much less is known about the underlying mechanisms of this association. Biological, psychological, and social explanations have been published.
Specific distresses experienced by autistic adults with GDC include social stigmas about gender- and neurodiversity, accessing gender affirming care, and managing the intersecting needs of autism and GDC – such as the tension between a need for undergoing physical gender changes versus the need for sameness and routine (Cooper et al., 2021). Autistic trans youth report distress from overwhelming negative feelings about gender incongruence, difficulty in accessing external support (e.g., gender-affirming care), and disparities in what needs they and their caretakers focus on (Cooper et al., 2022a). Some caretakers and clinicians working with young people worry that autism may impact one’s perception of gender and therefore focus on autism treatments instead of gender-based care.
It is critical to note that autistic children and youth are at higher risk of sexual victimization than the neurotypical population. Autistic individuals also experience a notably higher prevalence of mental health conditions than non-autistic individuals.
Despite the daily challenges faced by the autistic transgender community, their resilience shines through. Research indicates that transgender individuals with high self-esteem, assertiveness, and perceived social support from loved ones demonstrate greater resilience to psychiatric conditions than their counterparts (Hall et al., 2020). Further, a growing body of evidence reveals that trans autistic individuals experience significant reductions in poor mental health and suicidality when provided with gender affirming care. These improvements can be attributed to greater comfort within one’s body and the validation and hope that accompany acceptance and treatment.
Diagnosing GDC in autistic individuals, formal or otherwise, should be done carefully, taking into account the signs and outcomes related to autism and GDC. Autism traits like rigid thinking, sensory sensitivities, resistance to change, and social differences may compound GDC, making the diagnosis and treatment process more difficult.
Given our as-yet incomplete understanding of the co-occurrence of autism and GDC, treatment and care options must be developed based on the lived experiences of autistic individuals with GDC.
Because concepts of gender are very cultural, they can be difficult for autistic people to access, and many never assume the gender roles that society would have them accept. On a fundamental level, most autistic individuals experience and understand gender differently from, and often in contrast to, the wider population (Lawson & ARI, 2019).
Like autism, gender is experienced on a spectrum and is not confined to a binary or ternary lens. Without compassion, education, and understanding from broader society, autistic individuals experiencing GDC will continue to encounter discrimination and be underserved by the healthcare system. Compoundingly, if we do not actively listen to and adjust for the lived experiences of autistic people, humanity stands to lose an opportunity for deeper understanding and self-discovery. As we continue to build a society that recognizes the talents and strengths of autistic individuals, accepting gender fluidity is critical. With love, kindness, and acceptance, we can learn to understand gender the way autistic people do – as a characteristic of oneself that is not based upon outside forces trying to tell us what we are and how to act.
From: Autism and Gender Diversity. Dattaro L [2020] The Transmitter Neuroscience News and perspectives.
People who do not identify with the sex they were assigned at birth are three to six times as likely to be autistic as cisgender people are, according to the largest study yet to examine the connection . Gender-diverse people are also more likely to report autism traits and to suspect they have undiagnosed autism. Autistic people are more likely than neurotypical people to be gender diverse, several studies show, and gender-diverse people are more likely to have autism than are cisgender people.
Simon Baron-Cohen, professor of developmental psychopathology at the University of Cambridge and the new study’s lead investigator, led the collection of those data Gender-diverse people also report, on average, more traits associated with autism, such as sensory difficulties, pattern-recognition skills and lower rates of empathy — or accurately understanding and responding to another person’s emotional state. And they are five times as likely to suspect they have undiagnosed autism as cis people are, based on one dataset of 1,803 people whose survey included this question.
It also indicates a need for clinicians and educators to talk with autistic people about gender identity, and to be aware of potential mental health impacts that can result from ‘minority stress’ — or the difficulties associated with being part of a marginalized group. Being both autistic and gender diverse can intensify such stress . “Clinicians and practitioners in both fields — autism and gender identity — need to be aware of this association, and to factor it into how best to support the person’s mental health,” Baron-Cohen says. Nearly 70 percent of autistic gender-diverse adolescents say they need medical gender-related care, according to a small 2018 study, and 32 percent say their gender identity has been questioned because of their autism diagnosis . “It’s really, really distressing to read sometimes, where you have people who have very strong gender dysphoria and want to transition, and their therapist says, ‘Well, we need to first cure your autism before we transition,’ which is wrong on all levels,” This study demonstrates that both of these things can co-occur, and just because these things co-occur does not mean that one should be denied.” The findings also suggest that researchers should investigate how autism presents in gender-diverse people,
From: The Problem With Tethering Gender Dysphoria to Autism. Saleh N. [2025] Verywell Health.
Several hypotheses have been proposed to causally link autism to gender dysphoria, but there is no consensus regarding a clear link or a reason for a link. These hypotheses include:
- According to the extreme male brain theory, women are wired to think in more empathetic terms; whereas, men are more systematic in their thinking. According to this hypothesis, high levels of testosterone (a male hormone) in the womb result in an extreme male brain or male pattern of thought, which leads to both autism and gender dysphoria.
- Difficulty with social interactions has also been used to explain the development of gender dysphoria in autistic children. For instance, an autistic boy who is bullied by other boys might come to dislike other boys and identify with girls.
- Autistic people have difficulty communicating with others. This trait may contribute to others missing social cues about assigned gender which might increase the chance of developing gender dysphoria. Other people don’t pick up on cues of a child’s assigned gender, then the child isn’t treated in a fashion concordant with this assigned sex and may be more likely to go on to develop gender dysphoria.
- Gender dysphoria could be a manifestation of autism, and autistic-like traits could drive gender dysphoria. For instance, a child with a male-assigned gender and autism may become preoccupied with female clothes, toys, and activities. In fact, this apparent gender dysphoria may not be gender dysphoria at all but rather obsessive-compulsive disorder (OCD).
- Autistic children can demonstrate rigidity with respect to gender differences. They may have a hard time reconciling the difference between their assigned and experienced or desired gender. This increase in distress could possibly exacerbate gender dysphoria and make it harder for them to manage these feelings.
- Confusion in the development of gender identity or an altered pattern of gender identity development might contribute to gender dysphoria in children who have ASD.
- Limitations with imagination and empathy, common in autistic people, may make it hard for autistic people to recognize that they belong to a certain gender group.
No consensus on medical treatment could be drawn. Consenting to treatment may be difficult for autistic adolescents experiencing gender dysphoria because children may have difficulty understanding the long-term risks and irreversible effects of certain gender interventions. The clinician should develop a specialized consenting plan with risks and benefits presented in a concrete, step-wise, and accessible manner. Puberty suppression using hormones is a good option for adolescents who consent because it’s reversible.
There’s still much to learn about the co-occurrence of gender dysphoria and autism. Although rarely spoken about, gender is viewed as essential, unchangeable, and binary by all members of society, including experts doing studies and giving treatments. It’s possible that the distress that a trans child feels may stem from the universal expectation that gender is binary. Researchers continue to seek evidence-based approaches to treat people with both autism and gender dysphoria.
From: Theories on the Link Between Autism Spectrum Conditions and Trans Gender Modality: a Systematic Review. Watte L, Walsh R and Krabbendam L [2022] Review Journal of Autism and Developmental Disorders.
While research on the prevalence of co-occurring autism spectrum conditions (ASC) and trans gender modality (TGM) is available, less is known about the underlying mechanism of this association. Insight is needed to improve treatment of trans autistic people. This review provides an overview of theories on the ASC-TGM link and the available evidence for/against them published between January 2016 and October 2020. A systematic search was performed in PubMed, PsycINFO, Web of Science, and Scopus. This resulted in 36 studies, in which 15 theories were identified. Results indicate all theories lack substantial empirical support. Unlikely and promising theories were identified. The most promising theories were those on resistance to social norms and weakened sex differences.
Resistance to Social Norms: This theory proposes that TGM is more common amongst autistic people because they are less susceptible to societal prejudice/pressure than neurotypical people. In other words, this explanation entails that autistic people are free from normative influences when forming their gender identity, whereas neurotypical people are influenced by the gender binary norm. There were 18 mentions of this theory in the included papers. One study claimed evidence for, and no studies claimed evidence against the explanation. In an ASC population,
Weakened Sex Differences: According to this explanation, a high prevalence of TGM in autistic people is due to weakened sex differences (i.e., autistic men being less masculine/more feminine and autistic women being less feminine/more masculine). Weakened sex differences were mentioned as an explanation four times, with two papers claiming support for it and no papers claiming evidence against it. Vermaat et al. ( 2018) found that trans AFABs had similar AQ scores to neurotypical males and that trans AMABs had similar AQ scores to neurotypical females.
There are some noteworthy observations when looking closer at the biological explanations for the ASC-TGM link. One such observation is that no empirical evidence was provided for or against three out of four biological explanations (birth weight, genetic factors, and prenatal hormones).. Based on the evidence (i.e., 4 claims for and 3 against), the EMB theory could possibly be considered an explanatory factor for the ASC TGM link in AFABs. However, it cannot be the sole explanatory factor as it does not account for the co-occurrence of ASC and TGM in AMABs. The EMB theory additionally does not explain why there would be a sharp division in the mechanisms behind TGM between autistic AMABs and autistic AFABs. Consequently, the EMB theory may be considered an unlikely explanation for the ASC-TGM link.
When looking at all theories, there are potentially contradictory and complementary explanations to be found. For instance, the theories on minority stress and resistance to social norms are seemingly contradictory: while the theory on minority stress suggests that autistic people are marginalized and affected by social ostracism, the theory on resistance to social norms suggests that autistic people do not conform to social norms. However, these theories are not necessarily mutually exclusive: the fact that a person does not internalize social norms as their own does not mean that they are insensitive to negative reactions of their surroundings. A more substantial contradiction may be found between the theories on rigidity and sexual orientation, and the theories on weakened sex differences and resistance to social norms. While the former theories imply that autistic people have inflexible ideas about gender, the latter theories imply autistic people are less constrained by the gender-binary norm.
From: Sex/Gender Differences and Autism: Setting the Scene for Future Research. Lai M et al. [2015] Journal of the American Academy of Chid and Adolescent psychiatry. Science Direct.
The relationship between sex/gender differences and autism has attracted a variety of research ranging from clinical and neurobiological to etiological, stimulated by the male bias in autism prevalence. Findings are complex and do not always relate to each other in a straightforward manner. Distinct but interlinked questions on the relationship between sex/gender differences and autism remain underaddressed.
Recently, an increasing number of studies from different perspectives and methodologies have revisited how sex/gender differences are related to autism. Some have attempted to clarify how males and females with autism are similar or different in behavioral features via meta-analyses, multi-site large datasets, and by means of a male/female-balanced design. This has been extended to proteomics, anthropometrics, brain structure, and neural/somatic growth patterns On the other hand, studies of population genetics and genomics have revisited the sex/gender-differential liability hypotheses using well-powered datasets and advanced technology. The use of adequately powered datasets and statistical design as well as multi-level approaches offer promising avenues for advancing our understanding.
However, findings from different studies are complex and do not always relate to each other in a straightforward manner. This is because there are several different (but interlinked) questions embedded in the broad theme of the relationships between sex/gender differences and autism.
Using multivariate methodology, serum proteomic and transcriptomic studies also suggest that in high-functioning adults, females are different, rather than more severe, compared to males with autism. Anthropometric and neuroimaging studies show that high-functioning adult males and females with autism have different directions of shifts from same-sex/gender controls on the masculine–feminine dimension, that females are masculinized, yet males are feminized.
In light of the well-replicated, critical role of de novo mutations, which play a more substantial role in simplex than in multiplex autism, it is interesting that paternal age (which is associated with increased risk for de novo mutation in the gametes) correlates with the odds of simplex to multiplex autism in females but not in males. Corresponding to the predictions from the multi-factorial multi-threshold etiological model (level 3) that females with autism have a greater etiological/genetic load (reflecting a female-protective effect), data from the SSC show a trend toward more gene-rich de novo copy number variations (CNVs) in females than in males with autism, particularly microduplications, and in functional hub genes. This is also true for mutations indexed by single nucleotide variants and complete gene knock-out (in samples beyond SSC). Furthermore, females with autism are more likely to have highly penetrant pathogenic CNVs and are overrepresented among individuals carrying exonic deletions overlapping fragile X syndrome protein targets. An increased rate of mutation in females is also found in other neurodevelopmental disorders
An obvious genetic mechanism explaining sex/gender-differential liability are sex chromosomal genes, including male-specific risks by Y-chromosome genes such as SRY (and its downstream effects, including hormonal), and/or female-specific protections from the increased X-chromosome gene dosage in females (from genes that escape inactivation). Associated epigenetic mechanisms related to X-chromosome genes likely further contribute, including skewed X-inactivation, parent-of-origin allelic imprinting, and hypothetically, heterochromatin sink that results in sex-differential protein-mediated epigenetic effects on autosomes. Sex chromosome genes (and associated epigenetic effects) may account for only a portion of the etiological mechanisms, as autism risk genes largely involve autosomes.
Research into specific mechanisms has shown initial evidence in genetics, epigenetics, and the prenatal environment. Genetic and environmental effects are closely entwined through epigenetic and other regulatory mechanisms. Brain gene expression studies show that, although sex-differentially expressed genes do not overlap with autism candidate genes or genes aberrantly expressed in autistic brains, gene ontology enrichment analysis indicates that male-biased transcriptional modules are also implicated by the autism candidate genes. This suggests that it is downstream pathways that converge to show potential linkage between epigenetic (and genomic) sex differences and autism etiologies rather than individual genes per se. Early prenatal development is a critical period where pronounced sex-differential gene expression and exon use occurs, and where genetic and epigenetic mechanisms relevant to autism are placing potent permanent neurodevelopmental effects. Studies need to go beyond comparing groups at genetic or environmental levels alone, to investigate how their interplay has a role in producing potentially multiple “hits” in the emergence of autism.
Key References (to be continued)
(Notable) *** Associations between autism, gender dysphoria and gender incongruence: insights from the Swedish Gender Dysphoria Study (SKDS) (2025), by Fatih Özel, et al., published in Psychiatry Research
(Notable) *** Transidentities and autism spectrum disorder: A systematic review (2023), by Juliette Bouzy, et al., published in Psychiatry Research
(Notable) *** Sexuality and Gender Issues in Individuals with Autism Spectrum Disorder (2020), by Laura A. Pecora, et al., published in Child and Adolescent Psychiatric Clinics of North America
Chapter 26: What are the biochemical pathways that result in the Transgender Brain?
A review by Ian Cameron
Una is a professional science researcher and part-time university professor. The reader is encouraged to perform their own follow-up and fact-checking with the references listed below. Unintentional bias may exist in this article, as the author is herself an intersex transsexual woman. No personal, commercial, or academic conflict of interest exists between the author and any authors or institutions cited as references
It’s clear that a significant segment of human society has difficulty accepting that transsexuality is a real medical condition which is part of our inherited genetics. The common tactic of the blatant transphobe is to dismiss transgender people as freaks, psychopaths, or even monsters deserving of involuntary institutionalism. A transphobe, a person who does not accept anyone can be transgender, and state that being transgender is just not “common sense”.
“Common sense” is a meaningless phrase loaded with contrived meaning, almost always uncommon and insensible, the manifestation of the dogma of the day, and a lifetime’s accumulation of prejudice. If a more scientific approach is adopted towards understanding why people are transgender, the accumulated knowledge and experience need to be considered.
So why not dispense with “common sense”, and look at the facts, addressing the following points in order:
- How the genitals and brain develop their respective gendering, and significant cases of brain and genital misalignment resulting from endogenous or exogenous chemicals.
- Clues given to us from hereditary studies.
- Karyotype aberrations from the normal XX and XY chromosomes.
- Several significant differences from the average population which have been found in the brains of transsexuals.
- Contrary research which indicates there may be either a limited or no difference between the brains of transsexuals and the general population.
It should be considered that : “Transsexual” is used somewhat synonymously with “transgender”. The word “transsexual” will be the default term, as it typically is used in scientific literature, unless there is a specific need for the broader umbrella term “transgender.” Also note, “transwomen” refers to male-to-female transsexuals, and “transmen” refers to female-to-male transsexuals.
Brain Development
Gender identity was once thought of as being entirely a social construct, with most of our gender formation occurring between the ages of 1-4. (Bao, Gooren 2006) In the 21st century, the general thought is that gender identity is programmed at birth, although social factors can potentially overwhelm this programming. One tragic example is the “John-Joan-John” case, where a boy who lost his penis at 8 months was surgically turned into a girl, including the administration of estrogens and receiving psychological counseling. Although raised a girl all her life, she had the unshakeable feeling that she was in fact a boy. She transitioned back to male at age 14, and attempted to live as a male, but eventually, due to financial instability and a failing marriage, committed suicide. (Bao)
It’s common to hear the phrase “all babies start out female, and it’s only later that they become male,” and this is at least partially true. In fact, the influence of testosterone on a foetus has been described as a defeminization process, changing a foetus which was essentially predestined to be female into male. (Gooren, 2006) Testosterone production and the conversion of some testosterone to dihydrotestosterone between weeks 6 and 12 of pregnancy is critical for the initial development of male features, such as the penis, prostate gland, and scrotum. (Bao) In the absence of these male hormones, female genitalia develop instead. Brain development, however, does not occur in earnest until the second half of the pregnancy term, after the genitals have been developed, and the continued presence of male hormones results in a brain which has subtle, but critical physical differences from the female brain. (Bao)
The fact that the brain and the genitals develop at different times in the womb mean that a misalignment between the genitals and brain may develop, leading to either an intersex condition, or a transgender individual.
Example 1:Women with com plete androgen insensitivity syndrome (CAIS) develop bodies which are almost entirely female, and they tend to be sexually oriented towards men – despite having an XY karyotype. (Bao, Gooren 2006) Often, there is no indication the child is anything but female until surgery or an x-ray reveals the presence of undescended testes. (Gooren, 2006)
Example 2: Either a 5α-reductase-2 or a 17β-hydroxy-steroid dehydrogenase-3 deficiency will prevent the formation of testosterone into dihydrotestosterone, which will result in an XY karyotype baby girl with a large clitoris. However, when puberty arrives the girl will discover to her alarm that her clitoris grows significantly, her testes descend, and she will begin to take on masculine features. (Bao, Gooren 2006) Even though children with these birth defects are raised as girls, about 60% will become heterosexual males. (Bao) A Brazilian study found that of 25 5α-reductase-2 affected babies who were raised as girls, 13 changed their gender identity to male after puberty. (Gooren, 2006) Another study found that about 50% of 17β-hydroxy-steroid dehydrogenase-3 affected babies changed their gender identity back to male at puberty. (Gooren, 2006) What these results indicate to us is that testosterone likely more directly impacts the organization of the foetal brain than dihydrotestosterone. (Bao)
Example 3: Boys with an XY karyotype who are born with a cloacal exstrophy (where they are either partly or completely missing a penis) are typically changed surgically into “girls” just after birth, and are given female hormone therapy and counseling. However, about half of these new girls later determine that they are really boys, and change their social gender when they become teenagers or adults. (Bao, Gooren 2006)
Example 4: Girls with an XX karyotype born with congenital adrenal hyperplasia (CAH) (meaning they were exposed to high levels of testosterone in the womb) tend to develop male social tendencies and male personality features. (Hines, Zucker) They tend to be described by their parents as “tomboys”, with a high energy level. (Gooren, 2006) CAH girls are 100-300 times as likely to be transsexual, compared to the general female population, and 1 in 20 have serious gender identity problems. (Bao) One study found that 37% of CAH girls classified themselves as either lesbian or bisexual, a number far greater than the general population. (Gooren, 2006)
Example 5: Phenobarbital or diphantoin administered to pregnant women as anticonvulsants can increase the chance of giving birth to a transsexual child.(Bao, Dessens) The belief, not proven conclusively at this juncture, is that these chemicals disrupt the influence of testosterone on the brain in the womb. (Bao, Swaab) In other cases, it’s believed that prenatal exposure to oestrogens, progestins, and antiandrogenic chemicals could suppress endogenous testosterone production by interfering with the hypothalamic-pituitary-testicular axis. However, studies have focused largely on sexual preference as a result of this exposure, rather than gender identity, and in general these drugs were primarily only given to pregnant women between 1940-1970. (Gooren, 2006) There is some evidence that exposure to DDT could be responsible for increased polycystic ovary syndrome (PCOS) in women, increased idiopathic oligospermia (IO) in men, and increased transsexualism. Notably, transmen are found to often have PCOS, while transwomen often have IO. (Balen, Dorner) One study found transmen were 32.5% more likely to have endocrine dysfunction than XX karyotype women. (Futterweit)
Example 6: Kallmann’s Syndrome, a condition which occurs due to deficiency of gonadotropin-releasing hormone. The result can be an adult who has a loss of secondary sex characteristics. It is found much more frequently in genetic males than in genetic females, and male sufferers typically have what the medical literature describes as “eunuchoid growth,” with delayed or absent puberty, undeveloped infantile genitals, sparse body hair growth, a high-pitched voice, and other feminine features. Some of those with Kallmann’s Syndrome will become transsexual, although this is rare. (Meyenburg, 2001)
Even in these factual cases, questions remain about the connection between genetic and physical factors and gender identity. For example, why wouldn’t a preponderance of those with cloacal exstrophy feel they were boys? This likely attests either to the complexity of the physical processes involved, randomness in our development process, or the intense pressures social upbringing can exert upon both our gender and sexual attraction.
Other recent studies cast some question on what is more important in creating a feminized brain – the presence of two X chromosomes, or the presence of a Y chromosome and a sufficient level of testosterone. It’s a subtle argument, which essentially is trying to determine if hormones are the only differentiator between male and female brains, or whether there are other factors. One study which compared XX, XXY, and XY individuals came to the conclusion that having two X chromosomes is responsible for differences in the formation of the amount of grey matter in the cerebrum and precentral areas of the brain. However, the presence of testosterone appeared to be responsible for differences in the amygdala, parahippocampus, and occipital cortex. Thus, any condition which would reduce or interfere with the testosterone that the foetus was exposed to could result in an intersex or transgender brain. However, it is also possible that XXY individuals may have other compounding factors which can skew the data. (Lentini).
Heredity Studies
Transwomen who are sexually attracted to men have been found to be more likely to be the younger or youngest children in families with more brothers than sisters. (Bao) A study of 417 transwomen and 96 transmen found that transwomen had significantly more maternal aunts than uncles, while transmen showed no clear trends. Interestingly, this trend was strongest in lesbian transwomen, while an even stronger trend was seen for asexual transsexuals of both birth sexes, where they had more maternal uncles than aunts. (Green & Keverne) There is some speculation that this could be a result of a defect in the X chromosome from the mother, similar to fragile-X syndrome. Twin studies have shown a hereditary component for gender identity disorder (GID). (Swaab) One study of gender identity disorder in 314 twins found a heritable trait – and thus, implying strong genetic trait – as being 62% likely. (Coolidge) In some rare cases, two or more transsexuals have been born into a single family generation, (Green, Sabalis, Sadeghi) and in some cases transsexualism has been inherited from a transsexual parent. (Green)
Karyotype Aberrations
None of the cases above address profound karyotype aberrations, such as Klinefelter’s syndrome (47,XXY karyotype males, or 47,XXY/46,XY mosaics, or even the exceedingly rare 47,XXY/46,XX mosaicism), which can occur in 1 out of 1,000 male births. (Khandelwal) Other karyotype aberrations of note include 47,XYY males and 47,XXX females. In all of these cases the individual can develop gender identity disorder and become a transsexual (Khandelwal); indeed, this author personally knows individuals in this category who have become transsexuals.
Evidence for Physical Differences in the Transgender Brain
Despite the many profound genetic variations which can occur to create a transgender individual, most do not fall under any of the examples listed above. More subtle evidence must be examined, and the majority of studies searching for a physical cause for transgender individuals have found physiological and genetic differences which can be tested and measured. And most of these differences are found in our brains.
Before the results of brain studies are examined, there are some points of scientific fairness which need to be addressed. The first one is that all of the physical manifestations which are listed below are subtle effects. These will not be observed on an X-ray, nor even an MRI without specifically looking for them. If the differences in the brains of transsexuals were significant and profound, we wouldn’t be faced with having to continually justify our existence and alleged “motivations” in the first place. The second thing to note is that the uncertainty values of many of these studies are quite high, because there is significant variation in the brains of individuals from person to person. Finally, we need to recognize that because we are “rare and beautiful creatures,” and so many of us are closeted and unwilling to participate in studies, many of these studies have only examined a very small sample sizes of transsexuals.
Keeping all of that in mind, let us look at the evidence.
- XY karyotype men have about twice the volume and twice the number of neurons as XX karyotype women in two regions of the brain, called the BSTc and INAH3 regions. (Bao, Kruijver) An early study of cadaver brains found that transwomen have roughly the same numbers of neurons in these areas as XX women (Zhou), and this has been backed up by further non-invasive imaging studies. (Bao, Kruijver) A single transman who was tested was found to have an XY male number of neurons.(Bao, Kruijver) However, it should be noted that in the imaging study, the differences from person to person were somewhat wide-ranging, and the sample sizes were very small.
From Bao:
MRI data from 24 transwomen who had not started hormone treatment revealed that while their overall grey matter appeared similar to that of XY karyotype males, they possessed a significantly larger amount of grey matter in the right putamen. In fact, the grey matter structure of the transwomen was much closer to those seen in XX karyotype female subjects. In short, while the brains of the transwomen resembled XY male brains in terms of grey matter, in one specific region their brains appeared to be “feminized.” (Luders)
- A study of the white matter in the brains of 18 transmen, 24 XY karyotype males, and 19 XX karyotype females using diffusion tensor imaging (DTI) showed that the white matter structure of transmen was much closer to that of XY males than XX females. In fact, the white matter of their brain differed from the XY males only in a single region of the brain, whereas they differed from the XX women in three regions of the brain. None of the transmen had received hormone treatment at the time of the study. (Rametti, 2011) A follow-up study by the same researchers found that after the transmen had received hormone treatment, significant changes occurred in their brains, making them appear even more masculinized in certain regions which are associated with XY males. (Rametti, 2012)
From Rametti (2011):
A positron emission tomography (PET) study showed that smelling androgens (male pheromones) caused transwomen to respond in the hypothalamus region of their brain in a manner similar to XX karyotype women. However, smelling oestrogen-based pheromones also caused them to respond in the hypothalamus region in a manner similar to XY karyotype men. This combination of results suggests that transwomen occupy an “intermediate position with predominantly female features” in the way the hypothalamus reacted. (Berglund)
- An MRI study of 22 transwomen and 28 transmen examined the shape of the corpus callosum in the brain at a specific cross-sectional plane, and compared this shape with that observed in 211 XY karyotype males and 211 XX karyotype females. Their results demonstrated that not only could the sex of the patient be determined with 74% accuracy from the MRI picture, but the shapes of the brains in the transsexuals strongly reflected their gender, and not their biological sex. (Yokota)
From Yokota – MTF subjects are closer to females than males, and FTM subjects are closer to males than females.
- A recent study examined cortical thickness in the brain between 29 XY karyotype males, 23 XX karyotype females, 24 transmen, and 18 transwomen. None of the transsexual subjects had received any hormone treatment prior to the study. Using an MRI, the researchers found that the transwomen had more cortical thickness than the XY males in three regions of the brain. The transmen showed evidence of masculinization of their grey matter. In all transsexuals studied, the key differences from their biological sex were found in the right hemisphere. (Zubiaurre)
- Testing of a chemical produced in our bodies called “brain-derived neurotropic factor” (BDNF) in 45 transwomen found that when they were compared with 66 XY karyotype male control subjects, the transwomen had significantly lower levels of BDNF. However, this could be a result of higher stress levels and higher emotional trauma levels in the transsexual sampling. It should also be noted that no women control subjects were compared in this study. (Fontanari)
- Genetic testing of 112 transwomen and 258 XY karyotype male control subjects found that the transwomen had significant differences in androgen receptor genes. The result of this difference could lead to less effective testosterone signaling, meaning that there would be significantly less “masculinization” of the brain in the womb. This would result in a brain which was much more feminized, leading to a female gender identity. (Hare)
- An admittedly small study of 9 post-operative transwomen showed their brain activation was similar to women when viewing pictures showing erotic male images. (Oh) However, this study doesn’t so much address the root cause of the transsexuality as it shows that their sexual attraction towards men led to the same brain reaction as seen in heterosexual women.
Evidence Which May Indicate or Imply Physical Differences in the Transgender Brain
A 2013 study from Taiwan compared transsexuals with control subjects using two different assessments. In the first comparison, 41 transwomen were compared against 38 control subjects in a behavioural study to see how they would respond to pornographic short films. The results showed that transwomen overwhelmingly saw themselves in the role of their mental gender while watching the films. The second study was objective rather than subjective, and used functional MRI to compare the brains of 23 transwomen who had not been treated with hormones with 23 age-matched control subjects. The result was a significant difference in brain activity, primarily in the dorsal and pregenual ACC regions of the brain, between the transwomen and the controls. These regions of the brain are typically associated with processing feelings of social exclusion and emotional conflicts, so this may not indicate a difference in the brain due to gender identity differences, but rather a difference due to the negative social results of gender identity differences. (Ku, 2013)
Evidence Against Physical Differences in the Transgender Brain
Presenting a counter interpretation, however, there are some studies which have found no significant differences between the brains of transsexuals and the population at large.
- Early studies directly examining the corpus callosum in the brains of 20 transsexuals found no significant differences on a gross level between their brains and those of 40 control subjects. (Emory) However, The MRI technology which was employed was relatively new at the time of the study (1991).
- A study of four sex-sensitive mental processes (rotation of an object, visualization of objects, perception, and verbal skills) found no significant differences between transwomen and XY karyotype males. However, analysis of the results actually showed biological sex only influenced rotation and visualization, and previous results showing XY versus XX differences in perception and verbalization were not shown. This could point to a flaw in the study, as other studies have shown significant differences. (Haraldsen)
- Many studies have pointed to the difference between the length of the index finger and the ring finger being an indicator of androgen exposure before birth. In a “normal” XY karyotype male, the index finger is significantly shorter than the ring finger, which has led some to question whether transwomen with that same finger pattern have any significant physiological differences from XY males. However, as noted above gendering of the brain is not due to just simple androgen exposure, and studies have found the finger-length test to be poor, with a 60% overlap between XY men and XX women. (Gooren, 2006)
- A study of 30 transwomen and 31 transmen found only two transwomen possessed a detectable DNA defect. (Hengstschläger) This study has been criticized for being too small and for not looking deep enough into the genome to find potentially subtle differences in genetics. However, a sample size of 61 transsexuals is at least average, if not larger than average, and the study otherwise seems sound.
- Recently, there has been some focus on differentiating transsexual women who are attracted to men, versus those attracted to women. A criticism is that many of these brain studies do not account for these differences (e.g., Luders) and should do such, and some researchers claim that their studies of the brains of lesbian transwomen show no significant differences from male brains. (Savic) This has led to debate within the research community as to whether or not differentiation is even needed, with no clear resolution forthcoming. (e.g. Cantor, Italiano)
- Some researchers feel that the evidence is intriguing, but too subtle and difficult to study or replicate, and therefore not conclusive enough to say that transsexuality is a brain structure-focused intersex condition. (Meyer-Bahlburg)
Summary
Taking the entire breadth of the findings uncovered by my research, it appears that there is more than sufficient evidence that transgender persons either have a serious hormonal-based birth defect, have been exposed to exogenous chemicals which have impacted their gender development in the womb, have a genetic karyotype which differs from the general population, or via some other process have a brain structure which is different than would be indicated by their chromosomes. While no single study presents proof beyond any shadow of a doubt or with metaphysical certainty, taken together they do present a preponderance of evidence such that one can say with confidence that transgender individuals have a congenital gene-based difference from cissexual individuals.
References
Balen, Adam H., et al. “Polycystic ovaries are a common finding in untreated female to male transsexuals.” Clinical Endocrinology 38.3 (1993): 325-329.
Bao, Ai-Min and Swaab, Dick F. “Sexual differentiation of the human brain: Relation to gender identity, sexual orientation and neuropsychiatric disorders” Frontiers in Neuroendocrinology 32 (2011): 214–226.
Berglund, H. et al. “Male-to-Female Transsexuals Show Sex-Atypical Hypothalamus Activation When Smelling Odorous Steroids” Cerebral Cortex 18 (August, 2008): 1900—1908.
Cantor, James M. “New MRI Studies Support the Blanchard Typology of Male-to-Female Transsexualism” Arch Sex Behav 40 (2011): 863–864.
Coolidge, Frederick L., Linda L. Thede, and Susan E. Young. “The heritability of gender identity disorder in a child and adolescent twin sample.” Behavior Genetics 32.4 (2002): 251-257.
Dessens, Arianne B., et al. “Prenatal exposure to anticonvulsants and psychosexual development.” Archives of Sexual Behavior 28.1 (1999): 31-44.
Dorner, Gunter, et al. “Genetic and Epigenetic Effects on Sexual Brain Organization Mediated by Sex Hormones.” Neuroendocrinology Letters 22.6 (2001): 403-409.
Emory, Lee E., et al. “Anatomic variation of the corpus callosum in persons with gender dysphoria.” Archives of Sexual Behavior 20.4 (1991): 409-417.
Fontanari, Anna-Martha V. et al. “Serum concentrations of brain-derived neurotrophic factor in patients with gender identity disorder” Journal of Psychiatric Research (2013): 1-3 (advance copy).
Futterweit, Walter, Richard A. Weiss, and Richard M. Fagerstrom. “Endocrine evaluation of forty female-to-male transsexuals: Increased frequency of polycystic ovarian disease in female transsexualism.” Archives of Sexual Behavior 15.1 (1986): 69-78.
Gooren, Louis “The biology of human psychosexual differentiation” Hormones and Behavior 50 (2006): 589–601.
Green, Richard, and Eric B. Keverne. “The disparate maternal aunt–uncle ratio in male transsexuals: an explanation invoking genomic imprinting.” Journal of Theoretical Biology 202.1 (2000): 55-63.
Green, Richard. “Family cooccurrence of “gender dysphoria”: Ten sibling or parent–child pairs.” Archives of Sexual Behavior 29.5 (2000): 499-507.
Haraldsen, I. R. et al. “Sex-sensitive cognitive performance in untreated patients with early onset gender identity disorder” Psychoneuroendocrinology 28 (2003): 906–915.
Hare, Lauren et al. “Androgen Receptor Repeat Length Polymorphism Associated with Male-to-Female Transsexualism” Biol Psychiatry 65.1 (January 1, 2009): 93–96.
Hengstschläger, Markus, et al. “Sex chromosome aberrations and transsexualism.” Fertility and sterility 79.3 (2003): 639-640.
Hines, Melissa, Charles Brook, and Gerard S. Conway. “Androgen and psychosexual development: Core gender identity, sexual orientation, and recalled childhood gender role behavior in women and men with congenital adrenal hyperplasia (CAH).” Journal of Sex Research 41.1 (2004): 75-81.
Italiano, M. “Comment on Cantor” Arch Sex Behav 41 (2012):1079.
Khandelwal, Ashish et al. “A 47,XXY Female with Gender Identity Disorder” Arch Sex Behav 39 (2010):1021–1023.
Kruijver, Frank P. M. et al. “Male-to-Female Transsexuals Have Female Neuron Numbers in a Limbic Nucleus” The Journal of Clinical Endocrinology & Metabolism 85.5 (2000): 2034-2041.
Ku, Hsiao-Lun et al. “Brain Signature Characterizing the Body-Brain-Mind Axis of Transsexuals” PLOS ONE 8.7 (July, 2013).
Lentini, E. et al. “Sex Differences in the Human Brain and the Impact of Sex Chromosomes and Sex Hormones” Cerebral Cortex 23 (October, 2013): 2322-2336.
Luders, Eileen et al. “Regional gray matter variation in male-to-female transsexualism” Neuroimage 46.4 (July 15, 2009): 904–907.
Meyenburg, Bernd, and Volkmar Sigusch. “Kallmann’s Syndrome and Transsexualism.” Archives of Sexual Behavior 30.1 (2001): 75-81.
Meyer-Bahlburg, Heino FL. “Transsexualism (“Gender Identity Disorder”)–A CNS-Limited Form of Intersexuality?.” Hormonal and Genetic Basis of Sexual Differentiation Disorders and Hot Topics in Endocrinology: Proceedings of the 2nd World Conference. Springer New York, 2011.
Oh, Seok-Kyun et al. “Brain Activation in Response to Visually Evoked Sexual Arousal in Male-to-Female Transsexuals: 3.0 Tesla Functional Magnetic Resonance Imaging” Korean J Radiol 2012;13(3):257-264
Rametti, Giuseppina et al. “White matter microstructure in female to male transsexuals before cross-sex hormonal treatment. A diffusion tensor imaging study” Journal of Psychiatric Research 45 (2011): 199-204.
Rametti, Giuseppina et al. “Effects of androgenization on the white matter microstructure of female-to-male transsexuals. A diffusion tensor imaging study” Psychoneuroendocrinology 37 (2012): 1261—1269.
Sabalis, Robert F. et al. “The Three Sisters: Transsexual Male Siblings” Am J Psychiatry 131 (August 8, 1974): 907-909.
Sadeghi, Majid, and Ali Fakhrai. “Transsexualism in female monozygotic twins: A case report.” Australasian Psychiatry 34.5 (2000): 862-864.
Savic, Ivanka and Arver, Stefan. “Sex Dimorphism of the Brain in Male-to-Female Transsexuals” Cerebral Cortex 21 (November, 2011): 2525—2533.
Swaab, D.F. “Sexual differentiation of the human brain: relevance for gender identity, transsexualism and sexual orientation” Gynecol Endocrinol 19 (2004): 301–312.
Yokota, Y. et al. “Callosal Shapes at the Midsagittal Plane: MRI Differences of Normal Males, Normal Females, and GID” Proceedings of the 2005 IEEE Engineering in Medicine and Biology 27th Annual Conference Shanghai, China, September 1-4, 2005.
Zhou, Jiang-Ning, et al. “A Sex Difference in the Human Brain and its Relation to Transsexuality.” Nature 378.6552 (1995): 68-70.
Zubiaurre-Elorza, Leire et al. “Cortical Thickness in Untreated Transsexuals” Cerebral Cortex Advance Access, published August 31, 2012.
Zucker, Kenneth J., et al. “Psychosexual development of women with congenital adrenal hyperplasia.” Hormones and Behavior 30.4 (1996): 300-318.
NIH Public Access Author Manuscript – Reprod Toxicol. Author manuscript; available in PMC 2007 July 20.
Published in final edited form as: NIH-PA Author Manuscript NIH-PA Author Manuscript NIH-PA Author Manuscript – txflTextFlow3cdirFont0Reprod Toxicol. 2007 ; 23(3): 374–382.
From: Biological sex classification with structural MRI data shows increased misclassification in transgender women. Flint C et al. 2020. Neuropsychopharmacology in Nature.
Being transgender describes the stable feeling of belonging to the opposite sex rather than the biological sex assigned at birth, while the term cisgender (CG) describes the feeling of coherence between biological sex and perceived gender.
Although there is an ongoing social and political debate regarding the terms and phrases used to describe gender, little is known about how a divergence between biological sex and perceived gender emerges. A popular view is that sexual brain differentiation and body development diverge in transgender individuals (TIs). Evidence for this comes from studies in female infants with congenital adrenal hyperplasia, who develop male playing behaviour. Due to prenatally circulating testosterone, the brain of such female infants is structurally organized as a male brain, while their body development is female.
Previous research provides extensive information on how brain structure differs as a function of biological sex. Briefly, localized sex differences show higher grey matter volume in CG-men, while the volume of limbic structures is particularly increased in CG-women. However, sexual differentiation seems less prominent in the brain compared with physical appearance. Hence, brains cannot easily be classified into dimorphic gender categories.
Few ROI-based approaches have studied how the brain structure of TIs differs from CG-individuals. Compared with CG men, transgender women (biological sex male, perceived gender female, TW) show structural alterations of areas associated with body perception. Brain structures that repeatedly showed alterations across multiple studies are the putamen and the insula. However, the alterations are highly heterogeneous in their direction and the reported studies only investigated individuals before cross-sex hormone treatment (CHT). Comparisons between TW-pre/post-CHT with CG-individuals again exhibited heterogeneous results. CHT in TW combines treatment with antiandrogens and oestradiol and is associated with region-specific structural alterations of the brain such as local volume and cortical thickness decreases. However, longitudinal studies are scarce.
In the present study, we developed an SVM using hyperparameter optimization resulting in an accurate classification of biological sex based on structural MRI images. The classifier, trained on a large training set of healthy CG-individuals, performed equally well in three independent validation samples of healthy CG-individuals, and CG-participants suffering from MDD. When applying the same classifier to structural MRI data of TW, the SVM shows a much lower TPR, resulting in significantly more misclassifications of the biological sex of TW (male) in favour of their perceived gender (female). Moreover, the descriptive statistics of classification probabilities regarding TW indicate a pattern of prediction uncertainty that is not observable in CG.
Hence, our results shed light on two important aspects in biological psychiatry of TIs: The impact of hormonal treatment on brain structure, the separation of psychological distress (i.e., depression), hormonal treatment, and trait characteristics of being a TI.
Our results replicate the finding that biological sex is increasingly misclassified in TIs, as previously described. This might encourage further investigations into the cause for increased misclassifications in TW. Most notably and in contrast to previous studies, we could rule out that our findings are biased by comorbid depression and antidepressant medication. Given that the results of the first validation sample of healthy CG-participants were replicated in a large clinical sample of CG-patients suffering from major depression, the classifier is reliable and robust to noise even from psychiatric disorders such as MDD and medication, which have been associated with structural brain changes.
In comparison to CG-men, TW-pre-CHT showed larger volumes of the putamen, while TW-post-CHT showed lower volumes of both insula and putamen. Thus, TW independent of treatment state show brain-structural alterations in our regions of interest in comparison to both, CG-men and-women.
Detailed analysis of TW-pre compared with-post-CHT revealed a less pronounced pattern of structural brain alterations in TW-post CHT compared with CG-women. Comparing TW-pre with TW-post CHT revealed lower volume of TW-post-CHT in both regions of interest, as well as the whole-brain analysis. This implies that CHT induces a further feminization of brain structure in TW. This result fits with previous longitudinal studies that have shown reductions of cortical thickness in TW-pre to post-CHT [26]. Structural and functional alterations of the insula have consistently been associated with TIs compared to CG-individuals. The insula is associated with body and self-perception. Behaviourally, TW perceive an incoherence between their biological sex and perceived gender that is accompanied by altered insula activity in response to bodily sensations.
Brain structural alterations of the putamen have been associated with TW across multiple studies and independent of treatment state. We examined the putamen volume across different treatment states. Our study reveals that TW-pre show a higher volume of the putamen compared with CG-men and CG-women, while TW-post show lower volume of the putamen compared with CG-men, but not to CG-women. However, it remains unknown how CHT influences these structural alterations of TW. Longitudinal examinations are required to reveal region-specific structural alterations to estimate the impact of CHT of brain structure.
Our combined univariate and multivariate approach revealed associations of CHT with lower accuracy in detecting the biological sex of TW. Our results show that the brain structure of TW aligns with neither their biological sex (male) nor their perceived gender (female). This implies that there is a biological basis for being transgender and thus, destigmatizes TIs. Further, this evidence can be used in psychoeducation during treatment of gender dysphoria. The diagnosis of gender dysphoria is new to DSM-5 to allow for treatment if TIs suffers from distress due to incoherence between perceived gender and biological sex. Our results could relieve distress in transgender patients in case of the experience of guilt or shame due to the discrepancy between biological sex and perceived gender.
In line with this idea, hormonal processes, brain-structural development, and the development of gender identity are intertwined. Intrauterine hormones drive the development of gender identity, rather than social learning processes. The male physical appearance is formed in the first trimester, due to effects of testosterone, and the female body develops due to the lack of androgens in this period. While the maturation of reproductive organs is more or less limited to the first trimester, brain development is continuing throughout pregnancy. Hormonal influences after the first trimester do not change the biological sex, but the experience of gender and thus might be responsible for the incoherence between biological and experienced sex. Since hormonal influences change gender perception as well as brain structure, CHT may lead to misclassifications in the TW-group after treatment. Our univariate data indeed show that CHT is associated with structural brain alterations comparing TW-pre and post CHT to CG-individuals. A previous study showed increased misclassification of biological sex even in untreated TW, which we could not statistically support due to the small sample size of our untreated group. Therefore, further studies should follow up on this effect, with higher sample sizes of untreated TW to increase power. An extension of the design with a second control group (women with hormonal treatment) should be used to clarify whether misclassification is an effect of treatment only, due to the combination of being transgender and CHT.
In conclusion, this study, we present a highly accurate biological sex classifier in CG-individuals that shows a significantly decreased accuracy in TIs after CHT. Our results underline that the brain structure of TIs is similar to both, the brain structure of their perceived gender and biological sex. This implies that brain structure of TW differs from both CG-men and-women. Based on our brain-structural data, we suggest a dimensional rather than binary gender construct which will contribute to the destigmatization of Tis.
From: Brain Sex in Transgender Women Is Shifted towards Gender Identity. Kurth F et al. 2022. Journal of Clinical Medicine.
Transgender people report discomfort with their birth sex and a strong identification with the opposite sex. Transgender women are assigned male at birth but identify as female; transgender men are assigned female at birth but identify as male. Worldwide, the reported prevalence of transgender identities is rising [1], but our scientific understanding of how gender identity develops is still limited. Social explanations pointing to psychosocial and environmental influences [2,3] are complemented by biological explanations that include genetic predispositions and hormonal exposures [4–9]. Some (or perhaps all) of the aforementioned variables may have contributed to neuroanatomical variations in transgender brains, as repeatedly observed in both post mortem and in vivo studies published over the past three decades.
The overarching question addressed in those recent studies is whether the brains of transgender people are concordant with their birth sex or their gender identity, which is usually based on a so-called “classification accuracy” (i.e., how well can a brain be classified as male or as female). Interestingly, some studies reported that the classification accuracy was reduced in transgender individuals, albeit not all studies observed this effect. The reasons for divergences in study outcomes may be due to including individuals at different points in their gender-affirming process, using univariate classifiers and/or applying binary classifiers contrary to the notion that a mere binary classification may be insufficient to capture interactions between biological sex and gender identity.
The observed shift away from a male-typical brain anatomy towards a female-typical one in people who identify as transgender women suggests a possible underlying neuroanatomical correlate for a female gender identity. That is, all transgender women included in this study were confirmed to be genetic males who had not undergone any gender-affirming hormone therapy. Thus, these transgender women have been subject to the influence of androgens and grown up (at least up until a certain age) in an environment that presumably treated them as males. The combination of male genes ,androgens ,and (to some degree) male upbringing should ordinarily be expected to result in a male-typical brain, making a female-typical brain anatomy extremely unlikely. Yet, the brain anatomy in the current sample of transgender women is shifted towards their gender identity
Brain Sex in Transgender Women Is Shifted towards Gender Identity
From: Transgender brains are more like their desired gender from an early age. J Bakker 2018. European Society of Endocrinology.
Brain structure and function in gender dysphoria The concept of gender identity is uniquely human. Hence we are left with the phenomenon of men and women suffering from Gender Dysphoria (GD) also known as transsexualism to study the origins of gender identity in humans. It has been hypothesized that atypical levels of sex steroids during a perinatal critical period of neuronal sexual differentiation may be involved in the development of GD.
In order to test this hypothesis, brain structure and function in individuals diagnosed with GD were investigated using magnetic resonance imaging (MRI). Since GD is often diagnosed in childhood and puberty has been proposed to be an additional organizational period in brain differentiation, both prepubertal children and adolescents with GD were included in the studies.
First, brain activation upon exposure to androstadienone was measured, a putative male chemo-signal which evokes sex differences in hypothalamic activation (women > men). It was found that hypothalamic responses of both adolescent girls and boys diagnosed with GD were more similar to their experienced gender than their birth sex, which supports the hypothesis of a sex-atypical brain differentiation in these individuals. At the structural level, both regional gray matter (GM) volumes and white matter (WM) microstructure were analyzed using diffusion tensor imaging. In cis gender girls, larger GM volumes were observed in the bilateral superior medial frontal and left pre/postcentral cortex, while cis-gender boys had more volume in the bilateral superior-posterior cerebellum and hypothalamus. Within these regions of interest representing sexually dimorphic brain structures, GM volumes of both GD groups deviated from the volumetric characteristics of their birth sex towards those of individuals sharing their gender identity.
Furthermore, it was found that intermediate patterns in WM microstructure in adolescent boys with GD, but only sex-typical ones in adolescent girls with GD. These results on brain structure are thus partially in line with a sex-atypical differentiation of the brain during early development in individuals with GD, but might also suggest that other mechanisms are involved. Indeed, using resting state MRI, it was observed that GD-specific functional connectivity in the visual network in adolescent girls with GD. The latter is in support of a more recent hypothesis on alterations in brain networks important for own body perception and self-referential processing in individuals with GD.
Brain activity and structure in transgender adolescents more closely resembles the typical activation patterns of their desired gender, according to findings to be presented in Barcelona, at the European Society of Endocrinology annual meeting, ECE 2018. These findings suggest that differences in brain function may occur early in development and that brain imaging may be a useful tool for earlier identification of transgenderism in young people.
Transgenderism is the experience, or identification with, a gender different to the assigned biological sex, whilst gender dysphoria (GD) is the distress experienced by transgender people, and may be present from a very young age. Although GD incidence is rare, gender identity is an essential part of psychological health, and if unaddressed can lead to serious psychological issues. Current strategies for addressing GD in younger people involve psychotherapy, or delaying puberty with hormones, so that decisions on transgender therapy can be made at an older age.
Genetics and hormones contribute to sex differences in brain development and function that lead to more male- or female-typical characteristics; however, these processes are not well established. Furthermore, little is known on how early in life, or to what extent, the gender-typical characteristics of transgender people become established. Earlier diagnosis or better understanding of transgenderism could help to improve quality of life for young transgender people, and help families to make more informed decisions on treatment.
In this study, Dr. Julie Bakker from the University of Liège, Belgium, and her colleagues from the Center of Expertise on Gender Dysphoria at the VU University Medical Center, the Netherlands, examined sex differences in the brain activation patterns of young transgender people. The study included both adolescent boys and girls with gender dysphoria and used magnetic resonance imaging (MRI) scans to assess brain activation patterns in response to a pheromone known to produce gender-specific activity.
The pattern of brain activation in both transgender adolescent boys and girls more closely resembled that of non-transgender boys and girls of their desired gender. In addition, GD adolescent girls showed a male-typical brain activation pattern during a visual/spatial memory exercise.
Finally, some brain structural changes were detected that were also more similar, but not identical, to those typical of the desired gender of GD boys and girls. Dr Bakker says, “Although more research is needed, we now have evidence that sexual differentiation of the brain differs in young people with GD, as they show functional brain characteristics that are typical of their desired gender.”
Dr Bakker’s research will now investigate the role of hormones during puberty on brain development and transgender differences, to help guide and improve future diagnosis and therapy for GD adolescents.
Dr Bakker comments, “We will then be better equipped to support these young people, instead of just sending them to a psychiatrist and hoping that their distress will disappear spontaneously.” Transgender brains are more like their desired gender from an early age.
